Abstract
Oral steroid treatment is the first line of therapy for childhood nephrotic syndrome (NS). Nonetheless, some patients are resistant to this treatment. Many efforts have been made to explain the differences in the response to steroid treatment in patients with NS based on the genetic background. We have investigated single nucleotide polymorphisms of the MDR1 [C1236T (rs1128503), G2677T/A (rs2032582), and C3435T (rs1045642)] and MIF (G-173C, rs755622) genes in 170 children with NS. Of these children, 69 (40.6%) were initial steroid non-responders, and 23 (13.5% of total) developed chronic kidney disease. Renal biopsy findings, which were available for 101 patients, showed that 35 patients had minimal change lesion and 66 had focal segmental glomerulosclerosis. The frequencies of the MDR1 1236 CC (18.8 vs 7.2%) or TC (53.5 vs 43.5%) genotype and C allele (45.5 vs 29.0%) were significantly higher in the initial steroid responders than in the non-responders. Analysis of MDR1 three-marker haplotypes revealed that the frequency of the TGC haplotype was significantly lower in the initial steroid responders than in the non-responders (15.8 vs 29.0%). There was no association between the MIF G-173C polymorphism and clinical parameters, renal histological findings, and steroid responsiveness. These data suggest that the initial steroid response in children with NS may be influenced by genetic variations in the MDR1 gene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (NS) is one of the most common primary glomerular diseases in children. It can be clinically classified as steroid sensitive (SSNS) and steroid resistant (SRNS) according to the responsiveness to oral steroid treatment, which is the first line of therapy in childhood idiopathic NS. Responsiveness to the initial oral steroid treatment is one of the major prognostic factors of this disease. However, the detailed therapeutic mechanism of steroids on idiopathic NS is currently unknown, as is the pathogenesis.
Strenuous efforts have been made to explain the differences in the response to steroid treatment in patients with NS with various genetic backgrounds. These efforts have focused on the analysis of polymorphisms in a number of genes, including those coding for angiotensin-converting enzyme (ACE) [1–6], cytokines or growth factors [7–18], apolipoprotein E (APOE) [19–21], paraoxonase 1 (PON1) [22], multiple drug resistance 1 (MDR1, also known as ABCB1, ATP-binding cassette, sub-family B member 1) [23], and glucocorticoid receptor (NR3C1) [24, 25]. However, the results of these studies have not been consistent.
In the study reported here, we have focused on three of the above-mentioned genes, which are known to have some direct functional role in glucocorticoid metabolism: (1) the NR3C1 (glucocorticoid receptor) gene, (2) the MIF gene encoding macrophage migration inhibitory factor (MIF), a proinflammatory cytokine with a unique role as the physiological counter-regulator of the immunosuppressive effects of glucocorticoids [26], and (3) the MDR1 gene encoding P-glycoprotein (P-gp), which has a function in the elimination of specific corticosteroids from the cytoplasm [27]. In a previous study, we analyzed three NR3C1 gene polymorphisms [ER22/23EK (rs6189/rs6190), N363S (rs56149945), and BclI (rs number was not assigned)] in 190 Korean children with NS and 100 Korean control subjects [28]. Variant alleles of 22/23EK and N363S were not found in any of the patients or control subjects, and the BclI polymorphism was not found to be correlated with the development of NS, onset age, initial steroid responsiveness, renal pathologic findings, or the progression to end-stage renal disease (ESRD). In this study, therefore, the genotypes of the MDR1 and MIF SNPs were identified in children with NS to determine the correlation between the genotypes/allotypes and clinico-pathological features.
Materials and methods
Patients
A total of 170 Korean children diagnosed with idiopathic NS by the Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea between 1985 and 2006 were enrolled in this study. NS was defined as massive proteinuria of ≥40 mg/h/m2 with hypoalbuminemia of ≤2.5 g/dL without known causes [29]. In all patients, oral prednisolone 60 mg/m2/day or an equivalent dose of deflazacort was administered for 4 weeks at initial presentation, followed by 40 mg/m2 every other day for 4 weeks. Remission of NS was defined as the absence of proteinuria (≤4 mg/h/m2 or negative dipstick test) for 3 or more consecutive days. The responsiveness to later treatment with steroids and/or other immunosuppressive or cytotoxic drugs in relapsing patients or initial steroid non-responders could not be evaluated because the treatment modalities for those patients were not uniform. Chronic kidney disease (CKD) was arbitrarily defined as persistently high serum creatinine of ≥2.0 mg/dL.
Patients with a positive family history of NS and patients with a syndromic form of NS were excluded. Mutational analyses of the NPHS2 and the WT1 (exons 8 and 9) genes were performed on all patients with SRNS or focal segmental glomerulosclerosis (FSGS), and patients with mutations in either of these genes were excluded. Patients with congenital or infantile NS were also excluded.
Informed consent for the genetic analysis was obtained from all patients and/or their parents.
Genotyping
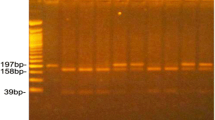
The genotypes of three known SNPs in the MDR1 gene (C1236T, G2677T/A, and C3435T) and one SNP in the MIF gene (G-173C) were determined by PCR–restriction fragment length polymorphism (RFLP) (Table 1). Genomic DNA was extracted and purified from peripheral blood using a QIA Amp DNA Blood Mini kit (Qiagen, Hilden, Germany), and the PCR products were purified using a QIA Quick PCR Purification kit (Qiagen), following which they were digested with the corresponding restriction enzymes. The digested PCR products were visualized in an ethidium bromide-stained 2.5% agarose gel using a UV camera. The genotypes of 100 healthy blood donors who comprised the normal control group were also determined.
Analysis of MDR1 three-marker haplotypes
Three-marker MDR1 haplotype analysis (C1236T, G2677T/A, and C3435T) was performed using software package PHASE ver. 2.1.1 (available online at: https://doi.org/www.stat.washington.edu/stephens/software.html) [30, 31].
Statistical analyses
The Hardy–Weinberg equilibrium (HWE) assumption was assessed for both the patient and control groups by comparing the observed numbers of each genotype with those expected under the HWE for the estimated allele frequency. Logistic regression analysis was used to estimate the odds ratios (OR) and 95% confidence intervals (CI) for the association between the genotypes, alleles or haplotypes and the risk of NS or initial steroid responsiveness. The results are presented as the mean values ± 1 standard deviation (SD), and a P value of ≤0.05 was considered to indicate statistical significance.
Results
The clinico-pathological profiles of the patients
Of the 170 patients enrolled in this study, 119 (70.0%) were male. The mean age at the onset of NS was 5.17 ± 3.31 years (range 1 year 2 months to approx. 16 years). Sixty-seven (39.4%) patients were resistant to initial steroid treatment, and 23 (13.5% of total) of these progressed to CKD. Renal histological examinations were available for 101 patients; 66 (65.3%) were FSGS patients and 35 (34.7%) were minimal change nephrotic syndrome (MCNS) patients (Table 2).
Influence of genotype on the NS onset in the patients
There was no significant difference in the distribution of genotypes and allotypes in all four SNPs in both genes between the patient group and the control group (Table 3). Also, the onset age of NS was not affected by any genotype or allotype variations in either gene (data not shown).
Influence of genotype on initial steroid responsiveness of the patients
The frequencies of the MDR1 1236 CC (18.8 vs 7.2%; OR 4.61, 95% CI 1.53–13.93, P = 0.007) or CT (53.5 vs 43.5%; OR 2.19, 95% CI 1.12–4.27, P = 0.022) genotype and C allele (45.5 vs. 29.0%; OR 2.05, 95% CI 1.29–3.25, P = 0.002) were significantly higher in the initial steroid responders than in the non-responders. The distribution of the genotypes and allotypes of MDR1 C2677T/A, MDR1 C3435T, and MIF G-173 C was comparable between the groups (Table 4).
Influence of genotype on the renal pathology and the renal functional outcome of the patients
There were no significant differences in genotype and allotype distribution for both genes between patients with MCNS and those with FSGS. In addition, progression to ESRD was not influenced by any of the genotype or allotype variations (data not shown).
Analysis of MDR1 three-marker haplotypes
Haplotype analysis of three polymorphisms (C1236T, G2677T/A, and C3435T) in the MDR1 gene revealed five major haplotypes; there was no difference in the distribution of these haplotypes between the patients and the control subjects (Table 5). When each haplotype was controlled for the remaining haplotype set, the frequency of the TGC haplotype in one or both alleles was significantly lower in the initial steroid responders than in the non-responders (15.8 vs 29.0%; OR 0.46, 95% CI 0.27–0.78, P = 0.004) (Table 6). Haplotype variations did not influence renal pathology or progression to ESRD (data not shown).
Discussion
In this study, we genotyped four known SNPs in the MDR1 and MIF genes in a group of pediatric patients with idiopathic NS to determine the correlation between the genotypes/allotypes and their clinico-pathological features. Two positive results emerged from this study: (1) the frequencies of the MDR1 1236 CC or TC genotype and C allele were significantly higher in the initial steroid responders than in the non-responders, and (2) the frequency of the MDR1 TGC haplotype was significantly lower in the initial steroid responders than in the non-responders.
The MDR1 gene encodes a membrane P-gp that functions as an ATP-dependent exporter of xenobiotics from cells [32]. P-gp is expressed in normal tissue, such as the intestine, liver, and kidneys, which have excretory functions, as well as in capillary endothelial cells of the brain, placenta, and testis and in peripheral blood cells [32]. In the kidney, P-gp is expressed in the brush border membrane of proximal tubular epithelial cells [32, 33]. Various types of structurally unrelated drugs, including steroids, are known to be substrates for P-gp [34, 35]. Several studies have been conducted to evaluate the association of P-gp expression with the responsiveness to steroids in patients with idiopathic NS [36–38]. Wasilewska et al. [38] measured P-gp expression on CD3-positive lymphocytes and found that CD3/P-gp expression was significantly higher in patients with NS than in the controls and that the difference was higher in steroid-dependent and frequent relapsing groups than in the non-frequent relapsing group. Funaki et al. [36] reported that the MDR1 mRNA expression level in nucleated cells of peripheral blood was variable in patients with idiopathic NS prior to remission, but apparently decreased after complete remission. In another study [37], MDR1 activity and mRNA expression in peripheral lymphocytes were higher in patients with steroid-, cyclophosphamide-, or cyclosporine-resistant NS than in patients who were sensitive to those drugs.
To date, approximately 50 SNPs have been reported in the MDR1 gene [39, 40]. Among these SNPs, C1236T, G2677T/A, and C3435T are the most common variants in the coding region of MDR1 [41]. While C1236T and C3435T are synonymous SNPs, G2677T/A causes an amino acid substitution (Ala899Ser/Thr). These three SNPs are in strong linkage disequilibrium, and we identified five major haplotypes (TTT, CGC, TGC, CAC, and TTC) in the patients and control groups. This haplotype distribution is similar to that reported in other studies conducted in Korean or Chinese subjects [42, 43]. Many studies have revealed that some SNPs of the MDR1 gene result in changes in P-gp expression and function among different ethnicities and subjects, with most of the attention focused on the MDR1 C3435T SNP. Although this SNP is a synonymous variation, it is associated with altered protein expression [35]. The mechanism by which the MDR1 C3435T SNP affects P-gp expression may be through possible linkage disequilibrium between the C3435T SNP and other MDR1 variants that control expression, including the nonsynonymous G2677T/A and synonymous C1236T SNPs [40]. In addition, the MDR1 C3435T SNP has been known to result in functional alteration of P-gp by affecting the timing of cotranslational folding and insertion of P-gp into the membrane, thereby altering the structure of substrate and inhibitor interaction sites [44].
There has been only one study [23] conducted to evaluate MDR1 SNPs in children with idiopathic NS. In that study, Wasilewska et al. evaluated MDR1 C1236T, G2677T/A, and C3435T SNPs in 108 children with idiopathic NS [23] . The results showed that the frequencies of the minor alleles in these three SNPs (1236 TT, 2677 TT, and 3435 TT) and the TTT haplotype were higher in late responders to oral prednisone (time to remission >7 days) than in early responders (time to remission <7 days). These researchers also observed the presence of three minor alleles and the 2677 TT genotype were more frequently in frequent relapsers than in non-frequent relapsers; there was no genotype–phenotype correlation in other clinical features, including the age of NS onset, the use of cytotoxic drugs, and total dose of steroids. However, the influence of the genotypes/allotype on the steroid responsiveness could not be evaluated because all patients in their study had SSNS. In contrast, our study found that the presence of the MDR1 1236 CC genotype and the C allele predicted a better initial response to steroids in children with idiopathic NS. Unfortunately, we could not compare early and late responders because the exact date of remission was unclear in some patients.
One of the more recent issues attracting the attention of researchers is the association of MDR1 genetic variation with the development and progression of certain diseases, especially those that involve impaired cellular barrier function at the level of the blood–brain barrier (Parkinson’s disease) [45, 46], small intestine (ulcerative colitis) [47], or kidney (non-clear cell renal carcinoma) [48]. Most of these studies [46–48] have revealed that the frequency of the MDR1 3435 TT genotype and/or T allele was significantly higher in patients with these diseases than in control subjects. Such an increased disease risk is explained by a lower P-gp expression and/or impaired tissue barrier function in patients with the TT genotype or T allele, which results in an ineffective protection of the body from potential environmental and metabolic toxins [49, 50]. Nonetheless, in our study, the genotype and the allele distribution of three MDR1 SNPs, including C3435T, were not significantly different between the patient and the control groups, suggesting that the expression level of P-gp may not be an important pathogenetic factor in idiopathic NS in children.
In a Chinese study [51] of 244 patients with ESRD, MDR1 3435 TT homozygotes were found to have a significantly higher serum creatinine level than CC homozygotes. This finding suggests that a low renal P-gp expression in 3435 TT homozygotes could lead to the exposure to higher concentrations of toxic agents, resulting in increased susceptibility to their effects. However, in our study, progression to ESRD was not influenced by any of the genetic variations studied.
We studied three MDR1 SNPs in the coding region. However, nucleotide and/or haplotype variants not only in the coding region but also in the promoter region of the MDR1 gene may be important for interindividual differences in P-gp expression [52]. In addition, the methylation status of certain CpG sites on the MDR1 promoter and/or other epigenetic mechanisms play a critical role in switch-on or -off of MDR1 gene expression [53].
MIF is expressed in glomerular parietal and visceral epithelial cells and in tubular epithelial cells in the kidney [51]. This factor plays important physiological roles in the regulation of macrophage function, lymphocyte immunity, and endocrine functions [18], as well as a pathogenetic role in some immunologically induced kidney diseases [26, 54–56]. Glucocorticoid counter-regulates MIF expression; low glucocorticoid level up-regulates MIF expression, while a high glucocorticoid level down-regulates it [26]. The association of MIF G-173C SNP with the progression of disease and response to steroid treatment in childhood NS has been studied in several recent studies [17, 18]. Vivarelli et al. [17] genotyped MIF G-173C in 257 Italian children with idiopathic NS and found that the frequency of the C allele (high producer) was higher in patients than in controls and also higher in patients with SRNS than with SSNS. This difference was particularly evident in patients with FSGS. In addition, carriers of the C allele were found to have a significantly higher probability of ESRD when compared with GG homozygous patients. Similarly, Berdeli et al. [18] investigated the MIF G-173C SNP in 214 children with idiopathic NS and found that the frequencies of the GC genotype and C allele were higher in the patients than in the control subjects. They also found an increased CC genotype frequency in patients with SRNS compared to those with SSNS, as well as an increased C allele frequency in patients with FSGS compared to other histopathological groups. Both the CC genotype and C allele were detected more frequently in patients with ESRD. Furthermore, age of onset was younger in patients with the CC genotype than in patients with the GC and GG genotypes. These findings suggest that the MIF -173C allele confers an increased risk of susceptibility to childhood idiopathic NS and plays a crucial role in steroid responsiveness. However, in our study, the MIF G-173C SNP was not associated with disease susceptibility, renal pathology, steroid responsiveness, or renal functional outcome in Korean children with idiopathic NS.
In summary, we found that the frequencies of the MDR1 1236 CC or TC genotype and C allele were significantly higher in the initial steroid responders than in the non-responders and that the TGC haplotype in MDR1 was significantly lower in the initial steroid responders than in the non-responders in Korean children with idiopathic NS. These findings suggest that the MDR1 1236 CC genotype and C allele may be a predictor for better initial steroid responsiveness. Further studies focusing on MDR1 mRNA and protein expression in these patients are needed to confirm a correlation.
References
Sasse B, Hailemariam S, Wüthrich RP, Kemper MJ, Neuhaus TJ (2006) Angiotensin converting enzyme gene polymorphisms do not predict the course of idiopathic nephrotic syndrome in Swiss children. Nephrology (Carlton) 11:538–541
Celik US, Noyan A, Bayazit AK, Büyükçelik M, Dursun H, Anarat A, Attila G, Matyar S (2006) ACE gene polymorphism in Turkish children with nephrotic syndrome. Ren Fail 28:401–403
Tsai IJ, Yang YH, Lin YH, Wu VC, Tsau YK, Hsieh FJ (2006) Angiotensin-converting enzyme gene polymorphism in children with idiopathic nephrotic syndrome. Am J Nephrol 26:157–162
Tabel Y, Berdeli A, Mir S, Serdaroğlu E, Yilmaz E (2005) Effects of genetic polymorphisms of the renin–angiotensin system in children with nephrotic syndrome. J Renin Angiotensin Aldosterone Syst 6:138–144
Serdaroglu E, Mir S, Berdeli A, Aksu N, Bak M (2005) ACE gene insertion/deletion polymorphism in childhood idiopathic nephrotic syndrome. Pediatr Nephrol 20:1738–1743
Al-Eisa A, Haider MZ, Srivastva BS (2001) Angiotensin converting enzyme gene insertion/deletion polymorphism in idiopathic nephrotic syndrome in Kuwaiti Arab children. Scand J Urol Nephrol 35:239–242
Ikeuchi Y, Kobayashi Y, Arakawa H, Suzuki M, Tamra K, Morikawa A (2009) Polymorphisms in interleukin-4-related genes in patients with minimal change nephrotic syndrome. Pediatr Nephrol 24:489–495
Tripathi G, Jafar T, Mandal K, Mahdi AA, Awasthi S, Sharma RK, Kumar A, Gulati S, Agrawal S (2008) Does cytokine gene polymorphism affect steroid responses in idiopathic nephrotic syndrome? Indian J Med Sci 62:383–391
Müller-Berghaus J, Kemper MJ, Hoppe B, Querfeld U, Müller-Wiefel DE, Morahan G, Schadendorf D, Tenbrock K (2008) The clinical course of steroid-sensitive childhood nephrotic syndrome is associated with a functional IL12B promoter polymorphism. Nephrol Dial Transplant 23:3841–3844
Wei CL, Cheung W, Heng CK, Arty N, Chong SS, Lee BW, Puah KL, Yap HK (2005) Interleukin-13 genetic polymorphisms in Singapore Chinese children correlate with long-term outcome of minimal-change disease. Nephrol Dial Transplant 20:728–734
Acharya B, Shirakawa T, Pungky A, Damanik P, Massi MN, Miyata M, Matsuo M, Gotoh A (2005) Polymorphism of the interleukin-4, interleukin-13, and signal transducer and activator of transcription 6 genes in Indonesian children with minimal change nephrotic syndrome. Am J Nephrol 25:30–35
Kim SD, Park JM, Kim IS, Choi KD, Lee BC, Lee SH, Hong SJ, Jin SY, Lee HJ, Hong MS, Chung JH, Lee TW, Ihm CG, Cho BS (2004) Association of IL-1beta, IL-1ra, and TNF-alpha gene polymorphisms in childhood nephrotic syndrome. Pediatr Nephrol 19:295–299
Kobayashi Y, Arakawa H, Suzuki M, Takizawa T, Tokuyama K, Morikawa A (2003) Polymorphisms of interleukin-4-related genes in Japanese children with minimal change nephrotic syndrome. Am J Kidney Dis 42:271–276
Holt RC, Ralph SA, Webb NJ, Watson CJ, Clark AG, Mathieson PW, Brenchley PE (2003) Steroid-sensitive nephrotic syndrome and vascular endothelial growth factor gene polymorphisms. Eur J Immunogenet 30:1–3
Tenbrock K, Schubert A, Stapenhorst L, Kemper MJ, Gellermann J, Timmermann K, Müller-Wiefel DE, Querfeld U, Hoppe B, Michalk D (2002) Type I IgE receptor, interleukin 4 receptor and interleukin 13 polymorphisms in children with nephrotic syndrome. Clin Sci (Lond) 102:507–512
Parry RG, Gillespie KM, Parnham A, Clark AG, Mathieson PW (1999) Interleukin-4 and interleukin-4 receptor polymorphisms in minimal change nephropathy. Clin Sci (Lond) 96:665–668
Vivarelli M, D’Urbano LE, Stringini G, Ghiggeri GM, Caridi G, Donn R, Tozzi A, Emma F, De Benedetti F (2008) Association of the macrophage migration inhibitory factor −173*C allele with childhood nephrotic syndrome. Pediatr Nephrol 23:743–748
Berdeli A, Mir S, Ozkayin N, Serdaroglu E, Tabel Y, Cura A (2005) Association of macrophage migration inhibitory factor -173C allele polymorphism with steroid resistance in children with nephrotic syndrome. Pediatr Nephrol 20:1566–1571
Hu P, Qin YH, Jing CX, Lei FY, Chen P, Li MF (2009) Association of polymorphisms at restriction enzyme recognition sites of apolipoprotein B and E gene with dyslipidemia in children undergoing primary nephrotic syndrome. Mol Biol Rep 36:1015–1021
Kim SD, Kim IS, Lee BC, Choi KD, Chung JH, Ihm CG, Cho BS (2003) Apolipoprotein E polymorphism and clinical course in childhood nephrotic syndrome. Pediatr Nephrol 18:230–233
Attila G, Noyan A, Karabay Bayazit A, Acartürk E, Anarat A (2002) Apolipoprotein E polymorphism in childhood nephrotic syndrome. Pediatr Nephrol 17:359–362
Biyikli NK, Alpay H, Yildiz N, Agachan B, Ergen A, Zeybek U, Bozkurt N, Ispir T (2006) Paraoxonase 1 192 and 55 polymorphisms in nephrotic children. Pediatr Nephrol 21:649–654
Wasilewska A, Zalewski G, Chyczewski L, Zoch-Zwierz W (2007) MDR-1 gene polymorphisms and clinical course of steroid-responsive nephrotic syndrome in children. Pediatr Nephrol 22:44–51
Zalewski G, Wasilewska A, Zoch-Zwierz W, Chyczewski L (2008) Response to prednisone in relation to NR3C1 intron B polymorphisms in childhood nephrotic syndrome. Pediatr Nephrol 23:1073–1078
Ye J, Yu Z, Ding J, Chen Y, Huang J, Yao Y, Xiao H, Yang J, Shen Y, Meng Q (2006) Genetic variations of the NR3C1 gene in children with sporadic nephrotic syndrome. Biochem Biophys Res Commun 348:507–513
Lolis E (2001) Glucocorticoid counter regulation: macrophage migration inhibitory factor as a target for drug delivery. Curr Opin Pharmacol 1:662–668
Webster JI, Carlstedt-Duke J (2002) Involvement of multidrug resistance proteins (MDR) in the modulation of glucocorticoid response. J Steroid Biochem Mol Biol 82:277–288
Cho HY, Choi HJ, Lee SH, Lee HK, Kang HG, Ha IS, Choi Y, Cheong HI (2009) Polymorphisms of the NR3C1 gene in Korean children with nephrotic syndrome. J Korean Pediatr Soc 52:1260–1266
International Study of Kidney Disease in Children (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. J Pediatr 98:561–564
Stephens M, Smith N, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Stephens M, Donnelly P (2003) A comparison of Bayesian methods for haplotype reconstruction from population genotype data. Am J Hum Genet 73:1162–1169
Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC (1987) Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci USA 84:7735–7738
Cordon-Cardo C, O’Brien JP, Casals D, Rittman-Grauer L, Biedler JL, Melamed MR, Bertino JR (1989) Multidrug-resistance gene (P-glycoprotein) is expressed by endothelial cells at blood-brain barrier sites. Proc Natl Acad Sci USA 86:695–698
Dilger K, Schwab M, Fromm MF (2004) Identification of budesonide and prednisone as substrates of the intestinal drug efflux pump P-glycoprotein. Inflamm Bowel Dis 10:578–583
Sakaeda T (2005) MDR1 genotype-related pharmacokinetics: fact or fiction? Drug Metab Pharmacokinet 20:391–414
Funaki S, Takahashi S, Wada N, Murakami H, Harada K (2008) Multiple drug-resistant gene 1 in children with steroid-sensitive nephrotic syndrome. Pediatr Int 50:159–161
Stachowski J, Zanker CB, Runowski D, Zaniew M, Peszko A, Medyńska A, Zwolińska D, Rogowska-Kalisz A, Hyla-Klekot L, Szprygner K, Weglarska J, Sieniawska M, Musiał W, Maciejewski J, Baldamus CA (2000) Resistance to therapy in primary nephrotic syndrome: effect of MDR1 gene activity. Pol Merkuriusz Lek 8:218–221
Wasilewska A, Zoch-Zwierz W, Pietruczuk M, Zalewski G (2006) Expression of P-glycoprotein in lymphocytes from children with nephrotic syndrome, depending on their steroid response. Pediatr Nephrol 21:1274–1280
Ieiri I, Takane H, Otsubo K (2004) The MDR1 (ABCB1) gene polymorphism and its clinical implications. Clin Pharmacokinet 43:553–576
Kroetz DL, Pauli-Magnus C, Hodges LM, Huang CC, Kawamoto M, Johns SJ, Stryke D, Ferrin TE, DeYoung J, Taylor T, Carlson EJ, Herskowitz I, Giacomini KM, Clark AG (2003) Sequence diversity and haplotype structure in the human ABCB1 (MDR1, multidrug resistance transporter) gene. Pharmacogenetics 13:481–494
Siegsmund M, Brinkmann U, Scháffeler E, Weirich G, Schwab M, Eichelbaum M, Fritz P, Burk O, Decker J, Alken P, Rothenpieler U, Kerb R, Hoffmeyer S, Brauch H (2002) Association of the P-glycoprotein transporter MDR1(C3435T) polymorphism with the susceptibility to renal epithelial tumors. J Am Soc Nephrol 13:1847–1854
Kim HJ, Hwang SY, Kim JH, Park HJ, Lee SG, Lee SW, Joo JC, Kim YK (2009) Association between genetic polymorphism of multidrug resistance 1 gene and Sasang constitutions. Evid Based Complement Alternat Med 6[Suppl 1]:73–80
Xu P, Jiang Z-P, Zhang B-K, Tu J-Y, Li H-D (2008) Impact of MDR1 haplotypes derived from C1236T, G2677T/A and C3435T on the pharmacokinetics of single-dose oral digoxin in healthy Chinese volunteers. Pharmacology 82:221–227
Kimchi-Sarfaty C, Oh JM, Kim I-W, Sauna ZE, Calcagno AM, Ambudkar SV, Gottesman MM (2007) A “silent” polymorphism in the MDR1 gene. Science 315:525–528
Furuno T, Landi MT, Ceroni M, Caporaso N, Bernucci I, Nappi G, Martignoni E, Schaeffeler E, Eichelbaum M, Schwab M, Zanger UM (2002) Expression polymorphism of the blood-brain barrier component P-glycoprotein (MDR1) in relation to Parkinson’s disease. Pharmacogenetics 12:529–534
Drozdzik M, Bialecka M, Mysliwiec K, Honczarenko K, Stankiewicz J, Sych Z (2003) Polymorphism in the P-glycoprotein drug transporter MDR1 gene: a possible link between environmental and genetic factors in Parkinson’s disease. Pharmacogenetics 13:259–263
Schwab M, Schaeffeler E, Marx C, Fromm MF, Kaskas B, Metzler J, Stange E, Herfarth H, Schoelmerich J, Gregor M, Walker S, Cascorbi I, Roots I, Brinkmann U, Zanger UM, Eichelbaum M (2003) Association between the C3435T MDR1 gene polymorphism and susceptibility for ulcerative colitis. Gastroenterology 124:26–33
Siegsmund M, Brinkmann U, Schaffeler E, Weirich G, Schwab M, Eichelbaum M, Fritz P, Burk O, Decker J, Alken P, Rothenpieler U, Kerb R, Hoffmeyer S, Brauch H (2002) Association of the P-glycoprotein transporter MDR1(C3435T) polymorphism with the susceptibility to renal epithelial tumors. J Am Soc Nephrol 13:1847–1854
Pauli-Magnus C, Kroetz DL (2004) Functional implications of genetic polymorphisms in the multidrug resistance gene MDR1 (ABCB1). Pharm Res 21:904–913
Marzolini C, Paus E, Buclin T, Kim RB (2004) Polymorphisms in human MDR1 (P-glycoprotein): Recent advances and clinical relevance. Clin Pharmacol Ther 75:13–33
Zhang WX, Chen B, Zhang W, Chen N, Yu ZC, Cai WM (2007) Effect of MDR1 gene polymorphism on progression of end-stage renal disease. Acta Pharmacol Sin 28:579–583
Kuwano M, Uchiumi T, Hayakawa H, Ono M, Wada M, Izumi H, Kohno K (2003) The basic and clinical implications of ABC transporters, Y-box-binding protein-1 (YB-1) and angiogenesis-related factors in human malignancies. Cancer Sci 94:9–14
Takane H, Kobayashi D, Hirota T, Kigawa J, Terakawa N, Otsubo K, Ieiri I (2004) Haplotype-oriented genetic analysis and functional assessment of promoter variants in the MDR1 (ABCB1) gene. J Pharmacol Exp Ther 311:1179–1187
Lan HY, Yang N, Nikolic-Paterson DJ, Yu XQ, Mu W, Isbel NM, Metz CN, Bucala R, Atkins RC (2000) Expression of macrophage migration inhibitory factor in human glomerulonephritis. Kidney Int 57:499–509
Lan HY, Bacher M, Yang N, Mu W, Nicolic-Paterson DJ, Metz C, Meinhardt A, Bucala R, Atkins RC (1997) The pathogenic role of macrophage migration inhibitory factor in immunologically induced kidney disease in the rat. J Exp Med 185:1455–1465
Santos L, Hall P, Metz C, Bucala R, Morand EF (2001) Role of macrophage migration inhibitory factor (MIF) in murine antigen-induced arthritis: interaction with glucocorticoids. Clin Exp Immunol 123:309–314
Acknowledgments
This study was supported by a grant from Seoul National University Hospital, Seoul, Korea (03-2007-028-0) and a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A080588).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, H.J., Cho, H.Y., Ro, H. et al. Polymorphisms of the MDR1 and MIF genes in children with nephrotic syndrome. Pediatr Nephrol 26, 1981–1988 (2011). https://doi.org/10.1007/s00467-011-1903-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-1903-0