Abstract
The aim of this study was to evaluate longitudinal changes in dialysate cancer antigen 125 (dCA125) levels over time and to analyze relationships between dCA125 and peritoneal glucose exposure (PGE) in children undergoing long-term peritoneal dialysis (PD). The study group included seven boys and four girls (mean age 13 ± 5.1 years) with a mean PD duration of 84.0 ± 1.1 months. A peritoneal equilibration test (PET) was performed, and dCA125 levels were measured in all patients. Peritoneal appearance rates (AR) of dCA125, the velocity of the decrease in dCA125AR values, and annual PGE levels were also calculated. The final tests were performed at a mean of 63.3 ± 3.5 months after the initial ones. Both dCA125 and dCA125AR levels showed statistically significant decrements during the follow-up period (p = 0.003), with the velocity of decrease in dCA125AR found to be 52.6 ± 19.4%. There were no significant differences in peritoneal transport parameters between the beginning and end of the study period. PGE values were significantly higher in the last year of the study than in the first year (p = 0.014), but the velocity of the decrease in dCA125AR levels was not related to total PGE. In conclusion, a significant decline was found in dCA125 and CA125 AR levels, reflecting mesothelial cell mass, in children undergoing long-term PD (>5 years), but these were not related to PGE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-term peritoneal dialysis (PD) is associated with the development of various structural and functional alterations to the peritoneal membrane and may eventually lead to the loss of function of the dialysis membrane in some patients. These alterations include loss of mesothelial cells, thickening of the submesothelial compact zone, and changes in vascularization [1–5]. At least some of these effects are thought to be associated with chronic peritoneal glucose exposure (PGE) to non-physiological PD fluids. In addition, glucose degradation products formed during autoclaving of the glucose-based solutions seem to be strongly cytotoxic towards the peritoneal mesothelium [6–8]. On a cellular level, chronic PD is associated with the phenomenon of epithelial to mesothelial cell transformation as well as the premature aging and senescence of mesothelial cells [9] .
Since peritoneal biopsy is not routinely performed due to its invasive nature, studies of peritoneal membrane structure have to rely on a number of biomarkers that are secreted by the peritoneal membrane and which can bee assayed in the effluent of PD. Of these, the most important in terms of usefulness in studies and clinical practice are cancer antigen 125 (CA125), interleukin-6 and, to a lesser degree, vascular endothelial growth factor [10].
Effluent CA125 can be considered as a marker of the mass of viable mesothelial cells and their turnover, and is recommended as a tool for longitudinal membrane status evaluation [11, 12]. Dialysate CA125 levels have been shown in some studies to decrease in long-term PD treatment [13–16], but there are currently limited longitudinal data on children undergoing long-term PD [17]. The aim of the study reported here was to evaluate changes in dCA125 levels in peritoneal effluent over time and to analyze relationships between dCA125 and PGE in children treated with long-term PD.
Patients and methods
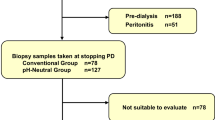
We previously published a cross-sectional study of dCA125 levels and peritoneal transport parameters in a group of 32 pediatric PD patients [18]. Of these children, 11 were still on PD at the time of writing this paper; these children comprised the patient group of this study. The values obtained from these patients in our earlier study were considered to be baseline values and were used to make a comparison with the results of the present study, which was performed 5 years later. The underlying renal diseases in these 11 children were: malformations of the urinary tract, including reflux nephropathy (n = 5); miscellaneous hereditary nephropathies (n = 4); chronic glomerulonephritis (n = 2). Demographic data and clinical characteristics of the patients are listed in Table 1.
The patients were stable on PD and had been free of peritonitis for at least 3 months before the peritoneal equilibration test (PET) analysis. However, all patients had experienced at least two peritonitis episodes prior to inclusion in this study. All 11 patients were grouped at the beginning of the study according to their urinary volumes; only one patient was anuric, three had urinary volumes of <400 ml/m2/day, and the remaining seven had urinary volumes of >400 ml/m2/day. During the course of the study, a number of children became anuric: at the end of the first year of follow-up, two children; by the end of the second year, three children; by the end of the study, five children. It is sometimes difficult to get pediatric patients to cooperate and they are occasionally hypertensive due to volume overload even if they have residual renal functions. Therefore, in our study, we had to prescribe hypertonic peritoneal dialysis solutions to our patients very often. A total of six patients had used hypertonic glucose solutions [2.27 g/dl glucose (395 mOsm/l) or 3.86 g/dl glucose (484 mOsm/l)] in the last 12 months prior to the present study, while four of these had used hypertonic glucose solutions from the very beginning of the initial study. The remaining five children were dialyzed with standard glucose-containing PD solutions.
Peritoneal transport characteristics
A standardized 4-h PET developed by the Pediatric Peritoneal Dialysis Study Consortium using an exchange volume of 1,100 ml/m2 (2.27% dextrose) was performed [19]. Dialysate and blood glucose levels were measured by the hexokinase method and creatinine by the kinetic method (U-240 autoanalyzer; Tectron, Tokyo, Japan) on the same day as the PET. All serum values were expressed as concentrations per unit volume of plasma water by dividing the serum values by a factor of 0.93 [19]. Because of the very high glucose concentration of the dialysate samples, the measurements were performed after diluting the dialysate samples 1:10 with distilled water. The dialysate-to-plasma (D/P) ratio for creatinine and the ratio of dialysate glucose to initial dialysate glucose concentration (D/D0) and mass transfer area coefficient (MTAC) of creatinine were calculated using PD Adequest software [20].
CA125 measurements
Dialysate samples for the CA125 measurements were taken from a test bag after 4 h and stored at −70°C until CA125 analysis. All samples were assayed at the same time to avoid interbatch variation using a commercially available chemiluminescent enzyme immunometric assay (Immulite OM-MA; Siemens Healthcare Diagnostics, Plainfield, IN). The Immulite OM-MA assay is designed specifically for the quantitative measurement of CA125 antigen. The detection limit of the assay is approximately 0.2 U/ml, defined as the concentration two standard deviations above the signal response at zero dose. The antibody used in the Immulite OM-MA procedure is highly specific for CA125 with low cross-reactivity to other substances that may be present in patient samples.
The peritoneal appearance rates (AR) of dCA125 (dCA125 AR) were calculated as the dCA125 (units per milliliter) multiplied by the drained volume (in milliliters), divided by the dwell time (in minutes) [21] and corrected for body surface area [22].
The velocity of the decrease in dCA125 AR was calculated as follows: \( {\left( {\hbox{dCA125 AR}} \right)_{\rm{first}}}--{\left( {\hbox{dCA125 AR}} \right)_{\rm{present}}}/{ }{\left( {\hbox{dCA125 AR}} \right)_{\rm{first}}} \)
Peritoneal glucose exposure
Peritoneal glucose exposure was reviewed annually according to each patient’s PD prescription, and expressed as grams per square meter per day for each patient. The average 24-h peritoneal glucose exposure was calculated from the volume and glucose concentration of the prescribed PD fluid in automated PD (APD) patients, ignoring the percentage of glucose absorption and the dwell time (range 100–150 min). For example, for an APD patient who was using six 1-l exchanges, five of 1.36% and one of 2.27%, the PGE would be estimated as 90.7 g of glucose per day. However, this approach cannot be used for continuous ambulatory PD (CAPD) patients due to the long dwell time. Thus, in PGE calculations for CAPD patients, individual D2/D0 and D4/D0 glucose values from PET analysis were used, and the PGE was separately estimated for each 2 h of dwell time, as follows:
-
$$ {\hbox{PG}}{{\hbox{E}}_{{1}}} = {\hbox{V}}\, \times \,{13},{\hbox{6 for first 2}} - {\hbox{h of the dwell time}} $$
-
$$ {\hbox{PG}}{{\hbox{E}}_{{2}}} = {\hbox{V}}\, \times \,{13},{6}\, \times \,\left( {{{\hbox{D}}_{{2}}}/{{\hbox{D}}_0}} \right)\,{\hbox{for second 2}} - {\hbox{h of the dwell time}} $$
-
$$ {\hbox{PG}}{{\hbox{E}}_{{3}}} = {\hbox{V}}\, \times \,{13},{6}\, \times \,\left( {{{\hbox{D}}_{{4}}}/{{\hbox{D}}_0}} \right)\,{\hbox{for third 2}} - {\hbox{h of the dwell time}} $$
For example, for a CAPD patient who was using four 1-l (1.36%) exchanges and who had D2/D0 = 0,50 and D4/D0 = 0.30, the PGE would be calculated as follows;
-
$$ {\hbox{PG}}{{\hbox{E}}_{{1}}} = {1}\, \times \,{13},{6}\,{\hbox{for first 2}} - {\hbox{h of the dwell time}} $$
-
$$ {\hbox{PG}}{{\hbox{E}}_{{2}}} = {1}\, \times \,{13},{6}\, \times \,0,{5}0\,{\hbox{for second 2}} - {\hbox{h of the dwell time}} $$
-
$$ {\hbox{PG}}{{\hbox{E}}_{{3}}} = {1}\, \times \,{13},{6}\, \times \,0,{3}0\,{\hbox{for third 2}} - {\hbox{h of the dwell time}} $$
-
$$ {\hbox{PGE total}} = {24},{28} {\hbox{g of glucose per exchange}},{\hbox{ and 4}}\, \times \,{24},{28} = {97},{12} {\hbox{g of glucose per day}}. $$
Statistics
Data are expressed as the mean ± standard deviation (SD). Differences during the follow-up were estimated using the paired standard t test. Correlations between the different parameters were estimated using Pearson correlations. Calculations were made using SPSS ver. 15 statistical software for Windows (SPSS, Chicago, IL). p values < 0.05 were considered to be significant.
Results
The final tests were performed on 11 children at a mean of 63.3 ± 3.5 (range 59.0–66.8) months after the initial tests, which in turn were carried out 22.7 ± 13.6 (range 1.5–47.7) months after the initiation of PD. dCA125, peritoneal transport properties, and glucose exposure values at the first and final measurement, respectively, are listed in Table 2. Both dCA125 and dCA125 AR levels were found to have significantly decreased during the follow-up period (p = 0.003). However, no significant difference was found for the PET parameters.
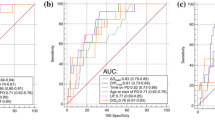
Final dCA125 and dCA125 AR values were lower than the first values in all patients (Fig. 1), and the velocity of the decrease in dCA125 AR were found to be 52.6 ± 19.4% (range 13-73%).
PGE estimations tended to increase steadily during the study period, beginning at 100 ± 43 (initial measurement) and increasing to 104 ± 49, 114 ± 42, 118 ± 47 and 130 ± 56 g/m2/day for each subsequent year. PGE values were significantly higher in the last year than in the first year (p = 0.014). The velocity of the decrease in dCA125 AR levels were not related to total peritoneal glucose exposure values (r = 0.34, p = 0.30) (Fig. 2).
Discussion
The peritoneal effluent of PD patients contains many substances. These can appear due to diffusion from the circulation, local peritoneal production, or both. The diffusion of a substance can be ignored when its local peritoneal production approaches or exceeds the serum concentration, such as CA125, for example, which is produced constitutively by mesothelial cells [10]. The concentration of CA125 increases linearly during a dwell of 4 h and is not influenced by the dialysis solution used. Consequently, CA125 can be a good marker to study in vivo peritoneal mesothelial cell mass or turn-over in PD patients. However, in this context, it has been recommended to express effluent CA125 as its dialysate appearance rate (CA125 AR) to avoid any influence of dwell time and ultrafiltration volume [11, 14, 15, 23]. In addition, the levels of CA125 should be corrected by the body surface area, especially in children, since they are physically more variable than adults [22].
The most important finding of our study is the observed significant decline in dCA125 concentrations and the dCA125 AR in children treated more than 5 years with PD. This result in accordance with those from published longitudinal studies [15–17]. This downward trend with time suggests a decrease in mesothelial cell mass. In an earlier cross-sectional analysis [18], we failed to observe a correlation between dCA125 levels and the duration of PD and had speculated that significant mesothelial cell mass reduction is unlikely to occur within the first few years of PD treatment. On the other hand, in a longitudinal study, Rodrigues et al. showed a significant decrease in effluent CA125 levels after 3 years of PD treatment [16]. The children comprising our study cohort showed a large inter-individual variability in dCA125 concentrations, but these were <25 U/ml/1.73 m2 in all patients at the end of the study. Pannekeet et al. [13] found both high and low dCA125 concentrations during the first 3 years of peritoneal dialysis treatment, but after 5 years of treatment they were only able to detect low dCA125 levels [13]. Interestingly, not all mesothelial cells express CA125, and there are two populations of peritoneal mesothelial cells, namely CA125-positive and CA125 -negative mesothelial cells [24]. However, the ratio of positive to negative CA125 mesothelial cells does not change with duration of PD, even though the mesothelial cell mass, similarly to CA125 concentration, decreases with time on PD [25]. This feature can partly explain inter-individual differences in the release of CA125 by mesothelial cells.
Using a one-point analysis to interpret CA125 levels in a group of patients is very difficult, since substantial inter-individual differences exist in both dCA125 AR and velocity of the decrease in dCA125 levels with the duration of PD treatment. dCA125 AR measurements may be more useful for the follow-up of individual patients than for comparisons of patient groups due to possible inter-individual differences in the release of CA125 by mesothelial cells. Our data confirm that serial determinations of dCA125 AR allow only the longitudinal follow-up of mesothelial cell mass in individual patients [14, 15].
However, there are a number of limitations to using dialysate CA125 as a clinical marker of mesothelial cell or membrane integrity [26]. It appears that the magnitude of CA125 release by mesothelial cells may depend not only on their number but also on their functional properties, which can be modulated by low pH, high lactate levels, and exposure to high glucose [7, 8]. The initial data on the relationship between dCA125 concentrations and PGE were obtained from PD biocompatibility studies [27–31]. The most consistent finding observed in all of these trials was that of an increased CA125 concentration in the effluent during dialysis with new biocompatible dialysis solutions. In a cross-over study in children, Haas et al. [31] reported that the peritoneal release of dCA125 increased twofold during bicarbonate APD compared with lactate APD. This finding was consistent with the recovery of the mesothelial cell layer, indicating improved in vivo mesothelial cell tolerance to high-dose glucose with the neutral pH PD solutions containing reduced glucose degradation products. In addition, previous studies confirmed that even the short-term exposure of mesothelial cells to acidic standard PD fluid results in a significant loss of cell viability and function [32, 33]. Schmitt et al. [33] found that with the standard lactate PD fluid, the peritoneal tissues were exposed to an acidic milieu for more than 1 h before lactate absorption and bicarbonate diffusion into the PD fluid resulted in peritoneal pH equilibration. In contrast, the pH remained in full equilibrium throughout the dialysis cycle when a bicarbonate-buffered solution was used. These results suggest that the pH of the dialysis fluid might be particularly relevant for APD, in which frequent short cycles continuously expose the peritoneal membrane to a cytotoxic acidic milieu [33]. The findings of the biocompatibility studies indicate that CA125 levels are a measure of mesothelial cell homeostasis because in a relatively short period, mesothelial cell mass is unlikely to change two- to four-fold; as such, the change in levels likely reflects synthesis by the resident mesothelial cell population, which are more sensitive to the less biocompatible standard fluid. Although Breborowicz et al. [34] reported limitations of CA125 as an index of peritoneal mesothelial cells in an in vitro study, they also showed a reduction of CA125 secretion and expression with chronic exposure to glucose solution. These divergent results emphasize the paucity of knowledge currently available on the control of CA125 synthesis, but they also reveal that CA125 synthesis can be up-regulated and down-regulated.
In our study, we found a significant increase in the PGE 5 years after the first measurement. However, no significant correlation was established between changes in the dCA125 AR levels and the total PGE. Inter-individual differences in the velocity of the decrease in dCA125 AR levels might have led to insignificant results.
Functional changes in the peritoneal membrane after long-term PD have indeed been described. However, there is no evidence that the mesothelium is a size-selective barrier to solute transport. In our study, we were unable to establish a relationship between dCA125 AR values and peritoneal transport parameters, although the results do support the hypothesis that mesothelial cells are not likely to play a direct role in peritoneal transport during stable PD treatment [13]. PGE may not have had any influence on the peritoneal transport parameters of those patients with a longer duration of PD in our study. In a longitudinal study in adults, Davies et al. [6] showed that an increase in solute transport with time was preceded by increased peritoneal exposure to hypertonic glucose, and further increases in glucose exposure were observed as solute transport continued to rise. In our study, although we noted only obvious significant increases in glucose exposure rates in last 2 years of follow-up, no increments could be shown in D/P creatinine levels with time on PD. This finding could be attributed to our patients’ multiple peritonitis episodes [35, 36]. On the other hand, a U-shaped curve of the D/P creatinine ratio was also present in a previous study on peritoneal transport [16].
In conclusion, based on our longitudinal results, dCA125 would appear to be a good marker for mesothelial cell mass or mesothelial cell turn over; as such, it can be used during a longitudinal follow-up of PD patients. However, dCA125 levels were found to vary considerably among the PD patients, and changes in the peritoneal mesothelial cell mass cannot be assessed using a single low value. Therefore, serial measurements of dCA125 might be a more valuable marker in the follow-up of individual patients. However, despite clinical experience with CA125, its current pre-eminent place as a marker of membrane integrity in PD needs to be confirmed by both in vitro investigations of CA125 regulation and studies to define longitudinal changes in large cohorts of PD patients and controls.
References
Williams JD, Kathrine JC, Topley N, von Ruhland C, Fallon M, Newman GR, Mackenzie RK, Williams GT (2002) Morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol 13:470–479
Saxena R (2008) Pathogenesis and treatment of peritoneal membrane failure. Pediatr Nephrol 23:695–703
Davies S, Phillips L, Griffiths AM, Russell LH, Naish PF, Russell GI (1998) What really happens to people on long-term peritoneal dialysis? Kidney Int 54:2207–2217
Fusshoeller A (2008) Histomorphological and functional changes of the peritoneal membrane during long-term peritoneal dialysis. Pediatr Nephrol 23:19–255
Schaefer F, Klaus G, Muller-Wiefel DE, Mehls O, Mid European Pediatric Peritoneal Dialysis Study Group (MEPPS) (1999) Current practice of peritoneal dialysis in children: results of a longitudinal survey. Perit Dial Int 19:S445–S449
Davies SJ, Phillips L, Naish PF, Russell GI (2001) Peritoneal glucose exposure and changes in membrane solute transport with time on peritoneal dialysis. J Am Soc Nephrol 12:1046–1051
Witowski J, Wisniewska J, Korybalska K, Bender TO, Breborowicz A, Gahl GM, Frei U, Passlick-Deetjen J, Jörres A (2001) Prolonged exposure to glucose degradation products impairs viability and function of human peritoneal mesothelial cells. J Am Soc Nephrol 12:2434–2441
Witowski J, Jörres A (2005) Effects of peritoneal dialysis solutions on the peritoneal membrane: clinical consequences. Perit Dial Int 25(S3):S31–S34
Yanez-Mo M, Lara-Pezzi E, Selgas R, Ramírez-Huesca M, Domínguez-Jiménez C, Jiménez-Heffernan JA, Aguilera A, Sánchez-Tomero JA, Bajo MA, Álvarez V, Castro A, del Peso G, Cirujeda A, Gamallo C, Sánchez-Madrid F, López-Cabrera M (2003) Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med 348:403–413
Krediet RT, Sampimon DE, Vlijm A, Coester AM, Struijk DG, Smit W (2009) Biological markers in the peritoneal dialysate effluent: are they useful. Contrib Nephrol 163:90–95
Visser CE, Brouwer-Steenbergen JJE, Betjes MGH, Koomen GCM, Belen RHJ, Krediet RT (1995) Cancer antigen 125: a bulk marker for the mesothelial mass in stable peritoneal dialysis patients. Nephrol Dial Transplant 10:64–69
Krediet RT (2001) Dialysate cancer antigen 125 concentration as marker of peritoneal membrane status in patients treated with chronic peritoneal dialysis. Perit Dial Int 21:560–567
Pannekeet MM, Koomen GCM, Struijk DG, Krediet RT (1995) Dialysate CA125 in stable CAPD patients: no relation with transport parameters. Clin Nephrol 44:248–254
Ho-dac-Pannekeet MM, Hiralall JK, Struijk DG, Krediet RT (1997) Markers of peritoneal mesothelial cells during treatment with peritoneal dialysis. Adv Perit Dial 13:17–22
Ho-dac-Pannekeet MM, Hiralall JK, Struijk DG, Krediet RT (1997) Longitudinal follow-up of CA125 in peritoneal effluent. Kidney Int 51:888–893
Rodrigues AS, Martins M, Korevaar JC, Silva S, Oliveira JC, Cabrita A, Castro e Melo J, Krediet RT (2007) Evaluation of peritoneal transport and membrane status in peritoneal dialysis: focus on incident fast transporters. Am J Nephrol 27:84–91
Bouts AHM, Groothoff JW, van Amstel SP, Zweers MM, Davin JC, Krediet RT (2000) Dialysate CA125 levels in children treated with peritoneal dialysis. Adv Perit Dial 16:328–331
Turhan P, Sever L, Caliskan S, Kasapcopur Ö, Sever A, Hacibekiroglu M, Arisoy N (2005) Dialysate CA125 levels in children on continuous peritoneal dialysis. Pediatr Nephrol 20:1615–1621
Warady BA, Alexander SR, Hossli S, Vonesh E, Geary D, Watkins S, Salusky IB, Kohaut EC (1996) Peritoneal membrane transport function in children receiving long-term dialysis. J Am Soc Nephrol 7:2385–2891
Vonesh EF, Burkart J, McMurray SD, Williams PF (1996) Peritoneal dialysis kinetic modelling: validation in a multicenter clinical study. Perit Dial Int 16:471–481
Pannekeet MM, Zemel D, Koomen GCM, Struijk DG, Krediet RT (1995) Dialysate markers of peritoneal tissue during peritonitis and in stable CAPD. Perit Dial Int 15:217–225
Kawanishi H, Moriishi M, Harada Y, Sakikubo NT, Tsuchiya S (2000) Necessity of correcting cancer antigen 125 appearance rates by body surface area. Adv Perit Dial 16:22–25
Jimenez C, Diaz C, Selgas R, Bajo MA, del Paso G, Sanchez-Tomero JA, Gonzalez-Gancedo P (1999) Peritoneal kinetics of cancer antigen 125 in peritoneal dialysis patients: the relationship with peritoneal outcome. Adv Perit Dial 15:36–39
Koomen GC, Betjes MG, Zemel D, Krediet RT, Hoek FJ (1994) Cancer antigen 125 is locally produced in the peritoneal cavity during continuous ambulatory peritoneal dialysis. Perit Dial Int 14:132–136
Sanusi AA, Zweers MM, Weening JJ, de Waart DR, Struijk DG, Krediet RT (2001) Expression of cancer antigen 125 by peritoneal mesothelial cells is not influenced by duration of peritoneal dialysis. Perit Dial Int 21:495–500
Topley N, Michael D, Bowen T (2005) CA125: Holy grail or a poisoned chalice. Nephron Clin Pract 100:c52–c54
Jones S, Holmes CJ, Krediet RT, Mackenzie R, Faict D, Tranaeus A, Williams JD, Coles GA, Topley N (2001) Bicarbonate/lactate-based peritoneal dialysis solution increases cancer antigen 125 and decreases hyaluronic acid levels. Kidney Int 59:1529–1538
Fusshoeller A, Plail M, Grabensee B, Plum J (2004) Biocompatibility pattern of a bicarbonate/lactate-buffered peritoneal dialysis fluid in APD: a prospective, randomized study. Nephrol Dial Transplant 19:2101–2106
Zeier M, Schwenger V, Deppisch R, Haug U, Weigel K, Bahner U, Wanner C, Schneider H, Henle T, Ritz E (2003) Glucose degradation products in PD fluids: do they disappear from the peritoneal cavity and enter the systemic circulation? Kidney Int 63:298–305
Williams JD, Topley N, Craig KJ, Mackenzie RK, Pischetsrieder M, Lage C, Passlick-Deetjen J, Euro Balance Trial Group (2004) The Euro-Balance Trial: the effect of a new biocompatible peritoneal dialysis fluid (balance) on the peritoneal membrane. Kidney Int 66:408–418
Haas S, Schmitt CP, Arbeiter K, Bonzel KE, Fischbach M, John U, Pieper AK, Schaub TP, Passlick-Deetjen J, Mehls O, Schaefer F (2003) Improved acidosis correction and recovery of mesothelial cell mass with neutral-pH bicarbonate dialysis solution among children undergoing automated peritoneal dialysis. J Am Soc Nephrol 14:2632–2638
Witowski J, Topley N, Jörres A, Liberek T, Coles GA, Williams JD (1995) Effect of lactate-buffered peritoneal dialysis fluids on human peritoneal mesothelial cell interleukin-6 and prostaglandin synthesis. Kidney Int 47:282–293
Schmitt CP, Haraldsson B, Doetschmann R, Zimmering M, Greiner C, Böswald M, Klaus G, Passlick-Deetjen J, Schaefer F (2002) Effects of pH-neutral, bicarbonate-buffered dialysis fluid on peritoneal transport kinetics in children. Kidney Int 61:1527–1536
Breborowicz A, Breborowicz M, Pyda M, Polubinska A, Oreopoulos D (2005) Limitations of CA125 as an index of peritoneal mesothelial cell mass. Nephron Clin Pract 100:c46–c51
Davies SJ, Bryan J, Phillips L, Russell GI (1996) Longitudinal changes in peritoneal kinetics: the effects of peritoneal dialysis and peritonitis. Nephrol Dial Transplant 11:498–506
del Peso G, Fernández-Reyes MJ, Hevia C, Bajo MA, Castro MJ, Cirugeda A, Sánchez-Tomero JA, Selgas R (2005) Factors influencing peritoneal transport parameters during the first year on peritoneal dialysis: peritonitis is the main factor. Nephrol Dial Transplant 20:1201–1206
Acknowledgments
This work was supported by the Turkish Foundation of Pediatrics. It was presented at the 15th Congress of the International Pediatric Nephrology Association, August 29–September 2, 2010, New York, USA, and has been published in abstract form (abstract; Candan C et al., Pediatr Nephrol 25:1940, 2010). The authors thank the nurses of the Children’s Hospital Peritoneal Dialysis Unit of Cerrahpasa Medical Faculty, especially Gulseren Pehlivan for her assistance in performing this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Candan, C., Turhan, P., Sever, L. et al. Dialysate CA125 levels after 5 years on continuous peritoneal dialysis. Pediatr Nephrol 26, 783–788 (2011). https://doi.org/10.1007/s00467-011-1764-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-1764-6