Abstract
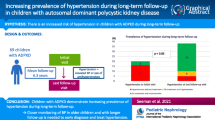
Autosomal dominant polycystic kidney disease (ADPKD) in children is sometimes considered to be a benign condition, with morbidity manifesting in adulthood. Therefore, diagnostic screening of children at risk is controversial. The aim of our study was to to compare the manifestations of ADPKD in children diagnosed by postnatal ultrasound (US) screening versus those presenting with symptoms. This was a retrospective chart review of children with ADPKD assessed in a single centre between 1987 and 2007. Age and reason for diagnosis were noted, and children were separated into two groups: (1) those diagnosed on the basis of family-based screening; (2) those presenting with a symptom. The two groups were compared for renal size, number of cysts, estimated glomerular filtration rate (eGFR), the presence of hypertension and microalbuminuria. In the 47 children with ADPKD (21 females) from 33 families who satisfied the enrollment criteria, mean (standard deviation) age at referral and last follow-up was 7.2 (4.4) and 12.9 (5.1) years, respectively, and the mean follow-up duration was 5.7 (3.6) years. Diagnosis was based on postnatal US screening in 31 children, whereas 16 were diagnosed after presenting with symptoms. The proportions of children with nephromegaly, hypertension, microalbuminuria and decreased eGFR, respectively, were similar in both groups. Based on these results, we conclude that renal-related morbidities, including hypertension and microalbuminia, do occur in children with ADPKD and at a similar frequency in those diagnosed after presenting with symptoms and those diagnosed upon postnatal screening. We suggest that at-risk children should have regular checks to detect hypertension. Moreover, affected children may benefit from novel therapies to minimise cystic disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is a common genetic disorder, with an incidence of 1:400–1000, characterised by progressive growth of renal cysts manifested by nephromegaly, often leading to end-stage kidney disease (ESKD). It is associated with intracranial arterial aneurysms, cardiac valvular defects and cysts in the liver, spleen and pancreas [1]. The mean age at death in the present era of renal replacement therapy in ADPKD is 59 years, and the main cause of death is cardiovascular disease including intra- and extracranial aneurysms [2–4]. ADPKD is caused by mutations in either PKD1 (85%) or PKD2 (15%). The identification of these genes and the drive to elucidate functions of encoded proteins, polycystin-1 and polycystin-2 are providing the basis for novel therapies to slow cyst growth, with some trials already ongoing in adults with ADPKD [1, 5].
Ideally, treatments for both the primary renal lesion (i.e cystogenesis) and complications (e.g. systemic hypertension) would be commenced before severe and irreversible damage occurs. ADPKD in children is sometimes considered to be a benign condition, with morbidity manifesting in adulthood. Therefore, screening children of affected adults to establish the diagnosis is controversial. Nevertheless, ADPKD lesions may originate as early as the fetal period [6–8]. In the study reported here, our aim was to compare the manifestations of ADPKD in children diagnosed by postnatal ultrasound (US) screening with those in children who presented with symptoms.
Methods
Starting with a comprehensive Nephrology Database, all records of children referred to our tertiary Paediatric Nephrology unit at Great Ormond Street Hospital between 1987 and 2007 with a clinical suspicion of ADPKD were analysed. We first excluded children with cystic kidneys with other diagnoses associated with renal cysts, including tuberous sclerosis (TS) [9], autosomal recessive PKD [10], oral-facial digital syndrome type 1 [11], hypomelanosis of Ito [12] and renal cysts and diabetes syndrome [13]. A diagnosis of childhood ADPKD was accepted when three or more cysts were visualised on US scans and there was either a positive familial history [14, 15] or a lack of evidence of other cystic disease, as outlined above. One of our index cases (who had multiple cysts in each kidney) had no family history, consistent with a de-novo mutation, as reported in about 10% of patients with ADPKD [16].
The cohort was divided in two groups: children with a history of ADPKD in one of their parents, who were asymptomatic at diagnosis and identified by postnatal US screening (group 1), and children who presented with symptoms (group 2). Case notes were reviewed for family history, pre- or postnatal presentation features, renal US reports, number and size of cysts, estimated glomerular filtration rate (eGFR) and the presence of complications, such as hypertension and microalbuminuria at presentation and at last follow-up. Children were generally seen in clinics every other year when blood pressure (BP), albumin excretion and US scans were evaluated. Plasma creatinine results were available in only seven children with ADPKD at diagnosis and in 33 at last follow-up, reflecting a lack of consensus between physicians whether to measure this parameter. The eGFR was calculated from plasma creatinine and patient height using the Schwartz–Haycock formula [17], with a k value of 33, which is specific for our laboratory [18], and patients were classified according to chronic kidney disease (CKD) stages [19].
US reports were assessed for kidney length as well as for the presence, number and size of renal cysts. If >10 cysts were present in either kidney, the patient was reported to have “multiple cysts”.
Kidney length was defined as the average of the longitudinal diameter of the right and left kidney in each patient and related to age-matched normal ranges [20]. The renal growth of our cohort was calculated by applying a linear fit to a plot of the kidney length from all of the patients (regression line), and the slope of this regression line was compared to the slopes of the normal ranges [20]. Unilateral nephromegaly was defined as being present when one kidney was of a normal length and the other was >2 standard deviations (SD) versus the controls. At presentation, only 19 patients had an exact kidney size from our radiology department. The others were referred with the US-based report without an exact kidney size.
Hypertension (or borderline hypertension) was defined as being present when systolic (SBP) and/or diastolic blood pressure (DBP) were >95th percentile (or between the 95th and 75th percentile) for gender-, age- and height-matched children on at least three measurements [21]. Children with previously diagnosed hypertension who were on antihypertensive therapy were also labelled “hypertensive”. Microalbuminuria was defined as being present when the spot urine albumin/creatinine ratio was ≥30 mg/g (3.4 mg/mmol) [22].
Numerical data were expressed as the mean (SD) and median (range), with differences between the two groups determined by the Student t test. The proportions between certain subgroups were compared with the chi-square test or, when at least one of the groups had ≤10 individuals, the Fishers exact test. Significance was defined as p < 0.05.
Results
Overview of the ADPKD cohort
Eighty children were identified with a possible diagnosis of ADPKD (Fig. 1). Thirty-three were excluded from further analysis. Of these, 19 were siblings of ADPKD patients but had overtly normal US scans. In five additional children, other diagnoses had eventually been made: one each with hypomelanosis of Ito, oro-facial-digital syndrome type 1 and renal cysts and diabetes syndrome and two with cystic dysplastic kidneys. Four others had cystic kidneys associated with TS and accordingly excluded to preserve the purity of the final ADPKD cohort. In five children, the mode of presentation was not documented, and these were also excluded from the analysis. The final cohort comprised 47 children from 33 overtly unrelated families, of whom 46 had a positive family history of ADPKD. Only one child, presenting with bilateral, markedly cystic kidneys, had a negative family history with both parents having a normal US scan when assessed in their third decade of life.
Mean (SD) ages at referral and last follow-up were 7.2 (4.4) and 12.9 (5.1) years, respectively, and the follow-up duration was 5.7 (3.6) years (Table 1). Survival was 100%.
Thirty-one children were asymptomatic and diagnosed by postnatal US screening based on their family history (group 1), whereas 16 presented with symptoms (group 2) comprising antenatal enlarged, echobright kidneys (n = 3), urinary tract infection (n = 6), abdominal, back or loin pain (n = 5), macroscopic hematuria (n = 1) and enuresis (n = 1).
Gender distribution was similar in both groups (p = 0.47): 21 were female (14 from group 1 and 7 from group 2) and 26 were male (17 from group 1 and 9 from group 2).
Mean age (SD) was similar in both groups at presentation (p = 0.31) and at last follow up (p = 0.49): 7.7 (4.4) and 12.4 (5.8) years for group 1 and 6.3 (4.3) and 11.1 (6.3) years for group 2, respectively. The average length of follow-up was 5.8 (3.6) and 5.6 (3.7) years, respectively (Table 2).
Of the 47 patients, eight had imaging performed to assess for intracranial aneurysms, but all scans were normal.
Renal ultrasound
At presentation, the majority of children (63%) had normal-sized kidneys with 16% unilateral nephromegaly. However, the cohort had accelerated kidney growth relative to the normal population (p < 0.001) (Fig. 2), and at the last follow-up 53% had enlarged kidneys and 26% had unilateral nephromegaly (Fig. 3). Similarly, only 38% had multiple cysts at presentation, but 81% presented multiple cysts at last follow-up (Table 1). Mean (SD) cyst diameter was 2.2 (1.2) cm. Two patients had a solitary cyst in the liver, and one patient had a solitary cyst in the pancreas.
Average kidney length in each patient at last ultrasound (US) scan. Solid circles Average kidney length of each patient at last US scan, top, middle and bottom lines the 95th, 50th and 5th centiles for age based on published percentiles [19] used in our hospital. Adapted from [19] to accommodate nephromegaly of ADPKD patients (original graph limited at 13 cm). Regression line (line in bold) was calculated using a linear fit of the most recent kidney length of all the patients as a total line, and the slope of this regression line was compared to the slopes of the normal ranges. The cohort had accelerated renal growth, as assessed by renal lengths, relative to the normal population (p < 0.001)
The proportions of patients with uni- or bilateral nephromegaly or multiple cysts were similar in both groups (Table 2).
Blood pressure
Hypertension was noted in 6 and 15% of the patients at presentation and at last follow-up, respectively (Table 1). There was no statistically significant difference between the groups (p = 0.74) (Table 3). However, no one had borderline hypertension at presentation, and 15% had reached this stage at the last follow-up.
Microalbuminuria
Eight (17%) and 17 (36%) of patients had microalbuminuria and at presentation and last follow-up, respectively (Table 1). Again, this was comparable in both group (p = 0.44).
Renal function
Of the patients, 39% had a decreased eGFR at the last follow-up, and this was similar in both groups (p = 0.59). One patient, diagnosed by US screening, had reached ESKD at last follow-up.
Discussion
Diagnostic screening, especially genetic testing, of children with a family history of ADPKD remains controversial, in part because establishing the diagnosis may cause psychological stress and affect the ability to obtain life or medical insurance [23] and in part because there is currently an absence of effective treatment preventing ADPKD cyst formation and growth. Furthermore, it would appear that there is a perception in the medical community that ADPKD is generally a rather benign condition in children.
Our study, which is not epidemiological in design, confirms that nephromegaly, decreased kidney function, hypertension and microalbuminuria can indeed occur in children with ADPKD. It is therefore the first study to highlight the fact that complications in children with ADPKD diagnosed by postnatal US screening and those diagnosed in children with ADPKD based on symptoms are similar.
Indeed, because all of the cases were assessed at a tertiary Paediatric Nephrology centre, one could contend that there had been a bias towards more severely affected patients. To account for this potential bias, we separated those children diagnosed solely because of their at-risk status and without overt symptoms from those who presented with overt symptoms, thereby obtaining two patient subgroups. It was striking that the proportions of cases with nephromegaly, decreased kidney function, hypertension and microalbuminuria were similar between the groups. Notably, at last follow-up, the child with the fastest progression, reaching ESKD at the age of 17 years, had been diagnosed by screening. Moreover, the three patients who were diagnosed antenatally and who were aged 1.5, 2.4 and 5.1 years, respectively, at last follow-up had normal BP and normal eGFR. However, all of three had microalbuminuria. Boyer et al. reported that 73% of 26 children who were diagnosed in utero or at day 1 of life were asymptomatic after a mean follow-up duration of 76 months [7] and that only two of the 26 reached CKD stage 4 at a mean age of 19 years.
Therefore, the most important finding of our study is that we found that clinically relevant ADPKD-associated morbidities, such as CKD stage ≥2, hypertension and microalbuminuria, can be present in children who do not present overt symptoms that would otherwise prompt a medical consultation. As such, our results emphasise the need to screen at-risk children in order to instigate appropriate treatment.
Grootendorst et al. describe relevant considerations in screening for CKD [24] that can also be applied to the ADPKD population. Several reports demonstrate that hypertension and albuminuria in adults with ADPKD are associated with progression of the renal disease, with an increased risk for development of cardiovascular disease and mortality [2, 3, 25, 26].
Hypertension is a well-recognised complication of ADPKD in adults, often being present before the onset of ESKD. It is probably in part mediated by renin overexpression within cystic kidneys [26, 27]. It has recently been reported that hypertensive children with ADPKD are also at risk for nephromegaly, increased left ventricular mass index (LVMI) and decreased renal function [25, 28–30]. The increase of LVMI even occurs in patients with borderline hypertension (75th and 95th percentile) and may be ameliorated by therapeutic blockade of the renin–angiotensin system [25]. These findings suggest that cardiovascular involvement, which is currently the main cause of death in ADPKD adults, starts very early in the course of ADPKD [2–4]. Seven (15%) of our paediatric cohort were found to have hypertension and seven (15%) had borderline hypertension at the last follow-up, which is consistent with findings from previous studies [7, 31]. The rate of hypertension among our patient cohort was lower than that reported in a number of other studies, which was around 30% [28, 32]. This may be related to the fact that these other studies used either home BP recordings or ambulatory blood pressure monitoring (ABPM), while we assessed office measurements. If this were to be the reason accounting for the difference, our findings emphasise the need to perform ABPM in order to better diagnose and treat hypertension.
Azurmendi et al. showed that even modest increases in albuminuria in adults with ADPKD are associated with subtle markers of renal (urine monocyte chemoattractant protein-1 levels) and vascular (carotid intima-media thickness) damage [33]. Seventeen (36%) of patients were found to have microalbuminuria at the last follow-up, and this was comparable in both groups. Shamshirsaz et al. reported overt proteinuria in 34% of 153 patients with a diagnosis of ADPKD between 18 months and 18 years and in 45% of 46 patients diagnosed before the age of 18 months [34].
Hypertension and microalbuminuria are modifiable risks factors and can be managed with optimal BP treatment and the early initiation of treatment with angiotensin-converting enzyme inhibitors (ACEi), as has been shown for adult patient populations [25, 35]. Consequently, more attention should be paid for monitoring the BP and albumin excretion in these children, with the aim of minimising the cardiovascular risks.
It was striking that more than half (53%) of our patient cohort had an increased average renal length >2 SD versus the age-matched controls at last follow-up and that the renal growth of our cohort was significantly increased compared to that of the normal population. Because nephromegaly in adults with ADPKD positively correlates with the progression of renal excretory failure [36, 37], clinical trials with the aim of reducing kidney cyst growth are currently underway in this population [1, 38–41]. The availability of proven effective treatment would clearly affect the indication for diagnostic screening of at-risk children.
In contrast, the proportion of children with CKD stage ≥2 was higher (39% for the entire cohort) than that found in most other studies which report normal renal function in the vast majority of children with ADPKD [8, 15, 42]. This apparent discrepancy may be explained by the fact that the commonly used Schwartz–Haycock formula overestimates GFR in CKD. Indeed, Schwartz et al. recently revised their originally published k-factor because of exactly this problem [43]. To account for this, we used a “k factor” specific for our unit and derived from Cr51–EDTA GFR measurements in order to obtain a more accurate estimate of GFR in the CKD population [18].
In accordance with the definition of our study cohort, we had excluded 19 siblings with normal renal US scans and due to the lack of facilities for PKD1/PKD2 mutation testing and/or linkage analyses, we could not definitively assign an “affected” or “non-affected” status. According to a recent large study, only about 10% of genetically affected individuals aged 15–29 years lack cysts on US scans [14], while no comparable data exist for children <15 years. The proportion of “missed” affected siblings may be even lower in our study, as there is some concordance with respect to age of onset within families [44]. Moreover, the mean age (SD) of the 19 sibling was 18.8 (3.1) years, and the US scan showed normal-sized kidneys without any cysts.
In summary, our results reveal that clinically relevant manifestations can indeed occur in children with ADPKD, even in those without overt symptoms. We believe that our data provide strong support for the need to screen children with a family history of ADPKD in order to monitor their BP and urine albumin measurement and to start appropriate treatment aimed at minimising the cardiovascular risks. Furthermore, because overt nephromegaly can develop in children with ADPKD, these children may be candidates for novel therapies to slow cyst growth.
References
Torres VE, Harris PC (2009) Autosomal dominant polycystic kidney disease: the last 3 years. Kidney Int 76(2):149–168
Ecder T, Schrier RW (2009) Cardiovascular abnormalities in autosomal-dominant polycystic kidney disease. Nat Rev Nephrol 5(4):221–228
Kelleher CL, McFann KK, Johnson AM, Schrier RW (2004) Characteristics of hypertension in young adults with autosomal dominant polycystic kidney disease compared with the general U.S. population. Am J Hypertens 17(11 Pt 1):1029–1034
Fick GM, Johnson AM, Hammond WS, Gabow PA (1995) Causes of death in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 5(12):2048–2056
Chang MY, Ong AC (2008) Autosomal dominant polycystic kidney disease: recent advances in pathogenesis and treatment. Nephron Physiol 108(1):1–7
MacDermot KD, Saggar-Malik AK, Economides DL, Jeffery S (1998) Prenatal diagnosis of autosomal dominant polycystic kidney disease (PKD1) presenting in utero and prognosis for very early onset disease. J Med Genet 35(1):13–16
Boyer O, Gagnadoux MF, Guest G, Biebuyck N, Charbit M, Salomon R, Niaudet P (2007) Prognosis of autosomal dominant polycystic kidney disease diagnosed in utero or at birth. Pediatr Nephrol 22(3):380–388
Fick GM, Johnson AM, Strain JD, Kimberling WJ, Kumar S, Manco-Johnson ML, Duley IT, Gabow PA (1993) Characteristics of very early onset autosomal dominant polycystic kidney disease. J Am Soc Nephrol 3(12):1863–1870
Consugar MB, Wong WC, Lundquist PA, Rossetti S, Kubly VJ, Walker DL, Rangel LJ, Aspinwall R, Niaudet WP, Ozen S, David A, Velinov M, Bergstralh EJ, Bae KT, Chapman AB, Guay-Woodford LM, Grantham JJ, Torres VE, Sampson JR, Dawson BD, Harris PC (2008) Characterization of large rearrangements in autosomal dominant polycystic kidney disease and the PKD1/TSC2 contiguous gene syndrome. Kidney Int 74(11):1468–1479
Denamur E, Delezoide AL, Alberti C, Bourillon A, Gubler MC, Bouvier R, Pascaud O, Elion J, Grandchamp B, Michel-Calemard L, Missy P, Zaccaria I, Le Nagard H, Gerard B, Loirat C, de Foetopathologie Société Française, Barbet J, Beaufrère AM, Berchel C, Bessières B, Boudjemaa S, Buenerd A, Carles D, Clemenson A, Dechelotte P, Devisme L, Dijoud F, Espérandieu O, Fallet C, Gonzalès M, Hillion Y, Jacob B, Joubert M, Kermanach P, Lallemand A, Laquerrière A, Laurent N, Liprandi A, Loeuillet L, Loget P, Martinovic J, Ménez F, Narcy F, Roux JJ, Rouleauto-Dubois C, Sinico M, Tantau J, Wann AR (2010) Genotype-phenotype correlations in fetuses and neonates with autosomal recessive polycystic kidney disease. Kidney Int 77(4):350–358
Feather SA, Winyard PJ, Dodd S, Woolf AS (1997) Oral-facial-digital syndrome type 1 is another dominant polycystic kidney disease: clinical, radiological and histopathological features of a new kindred. Nephrol Dial Transplant 12(7):1354–1361
Coward RJ, Risdon RA, Bingham C, Hattersley AT, Woolf AS (2001) Kidney disease in hypomelanosis of Ito. Nephrol Dial Transplant 16(6):1267–1269
Adalat S, Woolf AS, Johnstone KA, Wirsing A, Harries LW, Long DA, Hennekam RC, Ledermann SE, Rees L, van’t Hoff W, Marks SD, Trompeter RS, Tullus K, Winyard PJ, Cansick J, Mushtaq I, Dhillon HK, Bingham C, Edghill EL, Shroff R, Stanescu H, Ryffel GU, Ellard S, Bockenhauer D (2009) HNF1B mutations associate with hypomagnesemia and renal magnesium wasting. J Am Soc Nephrol 20(5):1123–1131
Pei Y, Obaji J, Dupuis A, Paterson AD, Magistroni R, Dicks E, Parfrey P, Cramer B, Coto E, Torra R, San Millan JL, Gibson R, Breuning M, Peters D, Ravine D (2009) Unified criteria for ultrasonographic diagnosis of ADPKD. J Am Soc Nephrol 20(1):205–212
Fick GM, Duley IT, Johnson AM, Strain JD, Manco-Johnson ML, Gabow PA (1994) The spectrum of autosomal dominant polycystic kidney disease in children. J Am Soc Nephrol 4(9):1654–1660
Reed B, McFann K, Kimberling WJ, Pei Y, Gabow PA, Christopher K, Petersen E, Kelleher C, Fain PR, Johnson A, Schrier RW (2008) Presence of de novo mutations in autosomal dominant polycystic kidney disease patients without family history. Am J Kidney Dis 52(6):1042–1050
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34(3):571–590
Gonzalez Celedon C, Bitsori M, Tullus K (2007) Progression of chronic renal failure in children with dysplastic kidneys. Pediatr Nephrol 22(7):1014–1020
Stevens LA, Levey AS (2009) Current status and future perspectives for CKD testing. Am J Kidney Dis 53[3 Suppl 3]:S17–S26
Han BK, Babcock DS (1985) Sonographic measurements and appearance of normal kidneys in children. AJR Am J Roentgenol 145(3):611–616
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114[2 Suppl 4th Rep]:555–576
Rademacher ER, Sinaiko AR (2009) Albuminuria in children. Curr Opin Nephrol Hypertens 18(3):246–251
Grantham JJ (2008) Clinical practice. Autosomal dominant polycystic kidney disease. N Engl J Med 359(14):1477–1485
Grootendorst DC, Jager KJ, Zoccali C, Dekker FW (2009) Screening: why, when, and how. Kidney Int 76(7):694–699
Schrier RW (2009) Renal volume, renin-angiotensin-aldosterone system, hypertension, and left ventricular hypertrophy in patients with autosomal dominant polycystic kidney disease. J Am Soc Nephrol 20(9):1888–1893
Loghman-Adham M, Soto CE, Inagami T, Cassis L (2004) The intrarenal renin-angiotensin system in autosomal dominant polycystic kidney disease. Am J Physiol Renal Physiol 287(4):F775–F788
Torres VE, Donovan KA, Scicli G, Holley KE, Thibodeau SN, Carretero OA, Inagami T, McAteer JA, Johnson CM (1992) Synthesis of renin by tubulocystic epithelium in autosomal-dominant polycystic kidney disease. Kidney Int 42(2):364–373
Cadnapaphornchai MA, McFann K, Strain JD, Masoumi A, Schrier RW (2009) Prospective change in renal volume and function in children with ADPKD. Clin J Am Soc Nephrol 4(4):820–829
Cadnapaphornchai MA, McFann K, Strain JD, Masoumi A, Schrier RW (2008) Increased left ventricular mass in children with autosomal dominant polycystic kidney disease and borderline hypertension. Kidney Int 74(9):1192–1196
Chapman AB, Guay-Woodford LM (2009) Renal volume in children with ADPKD: size matters. Clin J Am Soc Nephrol 4(4):698–699
Tee JB, Acott PD, McLellan DH, Crocker JF (2004) Phenotypic heterogeneity in pediatric autosomal dominant polycystic kidney disease at first presentation: a single-center, 20-year review. Am J Kidney Dis 43(2):296–303
Fencl F, Janda J, Blahova K, Hribal Z, Stekrova J, Puchmajerova A, Seeman T (2009) Genotype–phenotype correlation in children with autosomal dominant polycystic kidney disease. Pediatr Nephrol 24(5):983–989
Azurmendi PJ, Fraga AR, Galan FM, Kotliar C, Arrizurieta EE, Valdez MG, Forcada PJ, Stefan JS, Martin RS (2009) Early renal and vascular changes in ADPKD patients with low-grade albumin excretion and normal renal function. Nephrol Dial Transplant 24(8):2458–2463
Shamshirsaz AA, Reza Bekheirnia M, Kamgar M, Johnson AM, McFann K, Cadnapaphornchai M, Nobakhthaghighi N, Schrier RW (2005) Autosomal-dominant polycystic kidney disease in infancy and childhood: progression and outcome. Kidney Int 68(5):2218–2224
Ecder T, Chapman AB, Brosnahan GM, Edelstein CL, Johnson AM, Schrier RW (2000) Effect of antihypertensive therapy on renal function and urinary albumin excretion in hypertensive patients with autosomal dominant polycystic kidney disease. Am J Kidney Dis 35(3):427–432
Grantham JJ, Torres VE, Chapman AB, Guay-Woodford LM, Bae KT, King BF Jr, Wetzel LH, Baumgarten DA, Kenney PJ, Harris PC, Klahr S, Bennett WM, Hirschman GN, Meyers CM, Zhang X, Zhu F, Miller JP, Investigators CRISP (2006) Volume progression in polycystic kidney disease. N Engl J Med 354(20):2122–2130
Grantham JJ, Chapman AB, Torres VE (2006) Volume progression in autosomal dominant polycystic kidney disease: the major factor determining clinical outcomes. Clin J Am Soc Nephrol 1(1):148–157
Chapman AB (2008) Approaches to testing new treatments in autosomal dominant polycystic kidney disease: insights from the CRISP and HALT-PKD studies. Clin J Am Soc Nephrol 3(4):1197–1204
Cowley BD Jr (2008) Introduction: new insights, treatments, and management strategies for ADPKD. Clin J Am Soc Nephrol 3(4):1195–1196
Rizk D, Chapman A (2008) Treatment of autosomal dominant polycystic kidney disease (ADPKD): the new horizon for children with ADPKD. Pediatr Nephrol 23(7):1029–1036
van Keimpema LV, Nevens F, Vanslembrouck R, van Oijen MG, Hoffmann AL, Dekker HM, de Man RA, Drenth JP (2009) Lanreotide reduces the volume of polycystic liver: a randomized, double-blind, placebo-controlled trial. Gastroenterology 137(5):1661–1668
Fick-Brosnahan GM, Tran ZV, Johnson AM, Strain JD, Gabow PA (2001) Progression of autosomal-dominant polycystic kidney disease in children. Kidney Int 59(5):1654–1662
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20(3):629–637
Zerres K, Rudnik-Schöneborn S, Deget F (1993) Childhood onset autosomal dominant polycystic kidney disease in sibs: clinical picture and recurrence risk. German Working Group on Paediatric Nephrology (Arbeitsgemeinschaft für Pädiatrische Nephrologie). J Med Genet 30(7):583–588
Acknowledgements
Our research is supported by Great Ormond Street Hospital Special Trustees. A.S.W’s research is supported by the Manchester Biomedical Research Centre and the University of Manchester.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mekahli, D., Woolf, A.S. & Bockenhauer, D. Similar renal outcomes in children with ADPKD diagnosed by screening or presenting with symptoms. Pediatr Nephrol 25, 2275–2282 (2010). https://doi.org/10.1007/s00467-010-1617-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1617-8