Abstract
There is an association between growing slowly before birth, accelerated growth in early postnatal life and the emergence of insulin resistance, visceral obesity and glucose intolerance in adult life. In this review we consider the pathway through which intrauterine growth restriction (IUGR) leads to the initial increase in insulin sensitivity and to catch-up growth. We also discuss the importance of the early insulin environment in determining later visceral adiposity and the intrahepatic mechanisms that may result in the emergence of glucose intolerance in a subset of IUGR infants. We present evidence that a key fetal adaptation to poor fetal nutrition is an upregulation of the abundance of the insulin receptor in the absence of an upregulation of insulin signalling in fetal skeletal muscle. After birth, however, there is an upregulation in the abundance of the insulin receptor and the insulin signalling pathway in the IUGR offspring. Thus, the origins of the accelerated postnatal growth rate experienced by IUGR infants lie in the fetal adaptations to a poor nutrient supply. We also discuss how the intracellular availability of free fatty acids and glucose within the visceral adipocyte and hepatocyte in fetal and neonatal life are critical in determining the subsequent metabolic phenotype of the IUGR offspring. It is clear that a better understanding of the relative contributions of the fetal and neonatal nutrient environment to the regulation of key insulin signalling pathways in muscle, visceral adipose tissue and the liver is required to support the development of evidence-based intervention strategies and better outcomes for the IUGR infant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
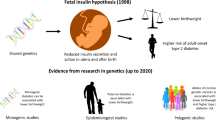
A world-wide series of epidemiological, clinical and experimental animal studies have demonstrated that there is an association among growing slowly before birth, accelerated growth in early postnatal life and the emergence of glucose intolerance, insulin resistance, type 2 diabetes and obesity in later life [1–5]. It has been proposed that when the fetal nutritional environment is suboptimal, adaptive responses result in the development of a “thrifty phenotype” in which there is a relative decrease in overall body growth and in the growth of organs such as the gut and liver, while there is differential sparing of the growth of key organs such as the brain and heart [6]. In the developed world, poor fetal substrate supply is more likely to be a consequence of placental insufficiency or maternal smoking than poor maternal nutrition, whereas in the developing world, intrauterine growth restriction (IUGR) is more likely a consequence of poor maternal energy intake before and throughout pregnancy [1–5]. For the IUGR infant, it appears, however, that being born into a postnatal environment characterised by a relative increase in nutrition has long-term adverse consequences [1–5].
To determine the type and timing of nutritional interventions that might be appropriate for the IUGR offspring, a number of important questions need to be addressed. These include determining how IUGR leads to the initial postnatal increase in insulin sensitivity and the associated acceleration in early postnatal growth. It is also unclear whether the origins of visceral obesity lie in the early fetal adaptations to a decreased substrate supply, or in the metabolic interactions among the adipose tissue, muscle and liver that occur after birth in offspring undergoing catch-up growth in postnatal life. Finally, while it is known that liver growth may be reduced as part of the adaptive response to a poor fetal substrate supply and that hepatic gluconeogenesis plays a key role in the fetal response to under-nutrition, it is not known to what extent these in utero changes contribute to the emergence of glucose intolerance in IUGR offspring.
Experimental studies on small animals including the rat and mouse have been of immense benefit in addressing each of these issues and have been well summarised in recent comprehensive reviews [1, 2, 4]. There are, however, a number of known limitations in using animal models with a short gestational period, in which organ system development may extend into the early postnatal period, for studies of developmental programming of those organ systems. In the rodent, for instance, it may be possible to achieve “lactational rescue” during the postnatal period to prevent the loss of structural units such as the nephron, cardiomyocyte and pancreatic β cell in IUGR offspring [1, 2, 4]. In the human, however, organogenesis occurs during early, rather than late, gestation and therefore the timing of such a rescue strategy in the postnatal lactational period may not apply. Furthermore, development of adipose tissue and the hypothalamic neural network that controls energy balance occur during the immediate postnatal period in the rat and mouse, rather than in fetal life as in the human, and this has consequences for the design and development of appropriate intervention strategies to limit the metabolic consequences of IUGR. Therefore, in this review we will consider some of the recent insights from studies in a large animal model of human IUGR resulting from experimentally induced placental restriction of growth in the sheep, in which the consequences for organ system development, including the physiological development of fetal muscle, adipose tissue and hepatic function, more closely reflects that of the IUGR human fetus. Where helpful we will compare findings from this large animal model of fetal growth restriction with findings from studies of fetal growth restriction in the rodent to determine which mechanisms appear to be recruited, independent of the type of animal model used and which are therefore likely to be of most interest when designing intervention strategies.
Patterns of early growth, insulin sensitivity and the emergence of insulin resistance
At birth, small-for-gestational-age (SGA) infants have low circulating insulin and insulin-like growth factor-1 (IGF1) concentrations [7, 8]. By 48 h after birth they are more insulin-sensitive and have higher plasma “free” non-esterified fatty acid (FFA) levels than their average-for-gestational-age (AGA) counterparts and then undergo a period of accelerated postnatal growth [9, 10] that is associated with the increased insulin sensitivity. This early period of increased insulin sensitivity and accelerated growth precedes the subsequent emergence of insulin resistance in later life [11–15].
Insulin signalling is mediated by a series of molecular pathways. In the presence of insulin, insulin receptor substrate proteins are phosphorylated, resulting in an interaction with the Src homology 2 (SH2) domain of the p85 regulatory subunit of phosphatidylinositol 3 kinase (PI3K). The catalytic subunit of PI3K, p110, then phosphorylates phosphatidylinositol (4,5) bisphosphate (PIP2) resulting in the formation of PI-3,4,5-triphosphate (PIP3). Protein kinase B/Akt is then recruited to the plasma membrane and Akt activation results in upregulation of the cellular metabolic responses to insulin and the mitogenic Ras-mitogen-activated protein kinase (MAPK) pathway, which mediates cell growth and differentiation (Fig. 1). The insulin signalling pathway, therefore, plays a critical role in nutrient sensing and in the control of tissue growth during development [16].
Rodent models of IUGR, including the maternal low protein diet and global maternal nutrient restriction, have also shown that fetal growth restriction is associated with an early postnatal phase of enhanced insulin sensitivity, followed by the subsequent emergence of insulin resistance and type 2 diabetes [17–19]. The offspring of rats fed a low protein diet during pregnancy have improved glucose tolerance at 3 months and muscle from these offspring exhibits enhanced basal and insulin-stimulated glucose uptake associated with an increase in the abundance of insulin receptors. By 15 months of age, however, the skeletal muscle from the protein-restricted offspring shows a decrease in insulin sensitivity associated with a decreased abundance of signalling molecules downstream of the insulin receptor, including the PI3K p85α regulatory subunit and PKCζ [19].
It has been shown that men who were born at a low birth weight (LBW) have reduced skeletal muscle expression of the insulin signalling molecules, including the PI3K p85α regulatory subunit and p110β catalytic subunit, the zeta-isoform of protein kinase C (PKCζ) and one of the PKCζ-regulated proteins, the insulin-dependent glucose transporter, GLUT4 [20]. In a recent follow-up study, these LBW men were shown to have a higher insulin-stimulated upregulation of PI3K p85α and p110β subunits in muscle compared with their control counterparts [21]. Interestingly, increased expression of p85α has been implicated in the development of insulin resistance, as excess p85α may act to sequester insulin receptor substrate-1 (IRS-1) and PI3K enzymatic activity into inert cellular foci incapable of PIP3 generation. In the LBW cohort there was also reduced phosphorylation of PKCζ and phospho-Akt at Ser 473 in response to insulin stimulation and again, each of these changes would be expected to be associated with reduced glucose uptake [21].
Therefore, experimental and clinical studies have demonstrated that poor growth in utero results in an initial increase in insulin sensitivity that is associated with accelerated postnatal growth and that these events precede the emergence of insulin resistance. What are not clear are the mechanisms through which IUGR leads to the initial increase in insulin sensitivity and catch-up growth during postnatal life. We have recently investigated the relationship between poor growth before birth and the emergence of increased insulin sensitivity after birth using a large animal model of placental insufficiency.
The placental origins of accelerated postnatal growth
Placental dysfunction that results in a restriction of fetal substrate supply is a major cause of an altered or reduced fetal growth trajectory, and placental size has been shown to predict fetal and neonatal weight across the entire birth weight range [1]. Several different experimental approaches have been used to produce placental insufficiency with resultant fetal growth restriction in small and large animal models, including surgical removal of the majority of endometrial caruncles from the uterus of the non-pregnant ewe prior to mating [22, 23]. This procedure restricts the number of placentomes that are formed from the beginning of pregnancy, thereby limiting placental growth and function. The placental delivery of oxygen and glucose to the fetus is restricted, and produces fetal hypoxaemia, hypoglycaemia and hypoinsulinaemia in late gestation and asymmetrical fetal growth [22–25]. There is evidence that there is a redistribution of cardiac output as the growth of the fetal brain, adrenal and heart are relatively spared, whereas fetal muscle, gut and liver mass are decreased [22–25]. The blood gas values and levels of nutrients and metabolic hormones in the placentally restricted IUGR sheep fetus are similar to that observed in fetal blood sampling studies of SGA infants [22–25].
In a recent study of the impact of placental restriction and IUGR on the mRNA and protein abundance of insulin signalling molecules in skeletal muscle samples during both late gestation (135–140 days’ gestation: term = 150±3 days’ gestation) and after birth in the sheep [26], it was shown that there was increased abundance of the insulin and IGF1 receptor (IGF1R) protein in the skeletal muscle of the IUGR fetus. Despite the increase in abundance of insulin receptor protein in the skeletal muscle of the IUGR fetus, there was no upregulation of the expression of any of the post-insulin receptor molecules in the skeletal muscle of the IUGR fetus [26]. In the IUGR fetus, the abundance of Akt2, PKCζ and GLUT4 were each lower in muscle compared with the normally grown control animal. Therefore, while growth-restricted fetuses had increased abundance of the insulin receptor in skeletal muscle, they had reduced abundance of signalling molecules responsible for the activation of GLUT4 [26]. This suggests that, while the hypoglycaemic, hypoinsulinaemic environment of the IUGR fetus may result in upregulation of the insulin receptor in muscle, there are mechanisms that limit the extent to which this increase in receptor expression can generate an increased metabolic or growth response in the muscle. One possibility is that the myocellular response to insulin in the IUGR fetus is limited primarily by the low circulating concentrations of insulin present.
At birth, IUGR lambs in this study were smaller and thinner, and demonstrated a higher daily fractional growth rate in the first 2 weeks of life compared with controls [26]. At 3 weeks after birth there was a persistence of the relative abundance of insulin receptor protein in skeletal muscle, and in addition there was now also an increase in protein expression of PI3K p85, Akt1, Akt2 and both GLUT4 and the insulin-independent GLUT1 transporters. These changes are consistent with an increase in both basal insulin-independent and insulin-stimulated glucose uptake that has been shown to occur in the skeletal muscle of the postnatal lambs during the phase of accelerated growth [27]. The findings from this study therefore suggest that fetal growth restriction due to a low placental substrate supply results in increased abundance of the insulin receptor in skeletal muscle that persists into postnatal life and can then, in the presence of the higher levels of nutrition present in postnatal life, result in the accelerated growth of the IUGR infant (Fig. 2). These findings may have direct relevance to IUGR in humans, particularly since it has been recently shown that early catch-up growth is related to the fetal growth pattern itself, irrespective of the final birth weight, and is associated with higher insulin sensitivity after birth [28].
Placental restriction results in an increase in the abundance of the insulin receptor in the fetal skeletal muscle in the absence of an increase in the abundance of the insulin signalling molecules or GLUT4. We propose that this is a consequence of the low plasma insulin concentrations that are present in the growth-restricted fetus. After birth, however, the increase in the abundance of the insulin receptor in the skeletal muscle persists and together with the transition to the higher level of nutrition present in postnatal life, this results in an increase in the abundance of the insulin signalling molecules, GLUT4 and with accelerated postnatal growth
Patterns of early growth and the development of visceral adiposity
Small-for-gestational-age infants have a reduced body fat mass at birth, but then develop a relative increase in body fat mass from 2 to 12 months of age, and go on to have a higher body mass index, fat mass and truncal fat distribution during childhood and adult life [29–32]. While catch-up growth is associated with an increased period of insulin sensitivity as summarised above, people who are thin at birth and develop obesity later in life have the highest risk of insulin resistance in adulthood [1–5]. In the sheep or pig, adipogenesis and lipogenesis occur in fetal life and, unlike the rodent, there is evidence in the sheep that the fetal fat can synthesise adipokines, including leptin, and that leptin may play a regulatory role in fat development before birth [33–36]. As in the human, LBW lambs and pigs also grow faster in the postnatal period and have a higher proportion of body fat in later life [27, 37–39]. We have reported that the major fat depot present in the fetal sheep is the perirenal adipose tissue and that the growth of this depot is relatively spared in IUGR fetuses in late gestation [36]. We have therefore investigated the impact of placental restriction and IUGR on the growth and functional development of visceral fat depots in the fetal and newborn lamb.
The normal growth and development of adipose tissue requires the sequential action of a suite of growth factors, hormones and transcription factors. IGF1 stimulates both proliferation and differentiation of preadipocytes in cell culture, and along with cAMP and glucocorticoids, is required for induction of adipose tissue differentiation [40–42]. After experimental induction of differentiation with supraphysiological levels of IGF1, growth-arrested preadipocytes go through clonal expansion prior to a significant increase in the expression of proliferator-activated receptor-γ (PPARγ), a key adipogenic transcription factor when heterodimerised with retinoid-X-receptor-α (RXRα). PPARγ activation initiates the transcription of genes involved in lipid accumulation and glucose metabolism, including lipoprotein lipase (LPL), and the adipokines, leptin and adiponectin. This then signals the terminal differentiation of the adipocyte [40–44]. There is evidence that the effect of IGF1R signalling on PPARγ mRNA expression may be via p38MAPK, which modulates the transcriptional activity of C/EBPβ, an adipocyte differentiation factor that induces PPARγ mRNA expression [43, 44].
We have recently shown that placental restriction of fetal growth results in decreased expression of IGF1 mRNA, but not IGF2, IGF1R, IGF2 receptor (IGF2R), or PPARγ mRNA in fetal perirenal adipose tissue in late gestation [36]. There was no effect of IUGR, on the expression of RXRα, adiponectin LPL, G3PDH, or GAPDH in the perirenal adipose tissue in the sheep fetus. Interestingly, the expression of IGF2 and that of PPARγ mRNA in perirenal fat were strongly related, suggesting that during fetal life IGF2 binding at the IGF1R may stimulate PPARγ mRNA expression in adipose tissue [36]. There was also a positive relationship between PPARγ and adiponectin mRNA expression, indicating that there may be functional activation of the PPRE in the promoter region of the adiponectin gene in perirenal adipose tissue in fetal life [36]. Importantly, we found that leptin mRNA was significantly decreased in the perirenal adipose tissue of the IUGR sheep fetus [36]. Evidence for a reduction in basal circulating leptin and higher relative increases in BMI have been described in adults who were born IUGR [2, 3, 45, 46].
In a follow-up study of the IUGR lamb in postnatal life, we found that measures of the perinatal nutritional environment were different between IUGR and control lambs and that the development of the visceral fat cells and depot were dependent on perinatal insulin and FFA concentrations. Furthermore, we determined that the relationships between visceral fat development and perinatal insulin and FFA concentrations were different in male and female lambs [47].
Independently of birth weight, female lambs had a greater relative perirenal fat mass than males during early postnatal life, and as there was no difference in the size of the adipocytes between the female and male lambs, the increase in fat mass in females is most likely due to their having more fat cells, i.e. hyperplasia of the adipocytes [47]. Interestingly, in both male and female lambs, the mean size of the perirenal adipocytes at 3 weeks of age was directly related to plasma insulin concentrations during the first 24 h after birth (Fig. 3). Therefore, there appears to be an important action of insulin in the immediate peripartum period on the triglyceride storage capacity of the adipocyte during later life. As plasma insulin concentrations are lower in female than male lambs, it appears that the adipocyte is more insulin-sensitive in the female. Circulating FFA concentrations were lower after birth in the IUGR female and IUGR male offspring compared with the normal birth weight lambs. Fatty acids are known inducers of adipocyte differentiation [48, 49], and consistent with this there was a strong relationship between plasma FFA concentrations during the first 24 h after birth and perirenal PPARγ mRNA expression and the mass of perirenal fat present in IUGR and control female, but not male, lambs at 3 weeks of age. We have therefore proposed that in the presence of relatively low insulin concentrations and thus a lower antilipolytic effect of insulin within the adipocyte in the female lamb, that the intracellular level of fatty acids is sufficient to activate PPARγ expression and adipogenesis resulting in a greater perirenal fat mass in the female compared with the male lamb (Fig. 4a) [47].
There is a relationship between plasma insulin concentrations during the first 24 h after birth and the mean cross-sectional area of perirenal adipocytes at 3 weeks of age in male (open circles, appropriate birth weight, and closed circles, low birth weight) and female (open triangles, appropriate birth weight, and closed triangles, low birth weight) lambs and this is independent of birth weight. This is an important relationship as it shows the importance of exposure to insulin in the immediate perinatal period in determining the triglyceride storage capacity of the adipocytes in later life [47]
Summary diagrams highlighting the effects of early insulin and non-esterified fatty acid (NEFA) exposure on the development of perirenal fat and on proliferator-activated receptor-γ (PPARγ) and leptin mRNA expression in a the female and b male lamb (reproduced with permission from Duffield et al. [47]). a In the female lamb, in the presence of lower plasma insulin concentrations, plasma NEFA concentrations during the first 24 h after birth drive the expression of PPARγ mRNA and the relative mass of perirenal fat at 3 weeks of age. We propose that this is a consequence of the lower antilipolytic actions of insulin in the female, which result in a higher concentration of NEFAs in the adipocyte. This results in NEFA activation of PPARγ expression, hyperplasia of the perirenal adipocytes, and a greater relative mass of perirenal fat in female compared with male lambs at 3 weeks of age. b In the male lamb, in the presence of higher plasma insulin concentrations, there is a greater antilipolytic action of insulin in the adipocyte. In IUGR males, the plasma NEFA concentrations are also lower than those of control counterparts and this results in lower PPARγ and leptin gene expression in the perirenal fat of IUGR male offspring at 3 weeks of age
In male lambs, the size of the perirenal adipocytes and perirenal fat mass at 3 weeks of age were each significantly related to plasma insulin concentrations during the first 24 h after birth. Interestingly, in contrast to the female lambs, there was no relationship between plasma FFA concentrations on day 1 and either perirenal fat mass or PPARγ mRNA expression in the male lambs. Again, in contrast to the IUGR female lambs, PPARγ and leptin mRNA expression in perirenal fat were each lower in the IUGR male compared with the control counterpart. We proposed that in the presence of higher plasma insulin concentrations in the male that insulin has a stronger antilipolytic action in the visceral adipocyte, which together with the lower FFAs present in the IUGR male results in reduced fatty acid activation of PPARγ and leptin gene expression (Fig. 4b). A decrease in PPARγ mRNA expression in adipose tissue has been shown to be associated with a decrease in adipose tissue and hepatic insulin sensitivity, particularly during periods of high caloric intake [50]. The lower level of PPARγ expression in the perirenal visceral fat of the male IUGR lamb may therefore predispose the male IUGR lambs to the subsequent emergence of insulin resistance.
As discussed above, leptin expression is also lower in the perirenal adipose tissue in IUGR fetuses in late gestation and this decrease appears to persist into postnatal life in the male, but not the female lamb. While leptin expression was lower, there was no reduction in circulating plasma leptin levels in the IUGR males. This may be a consequence of the relatively small contribution of leptin synthesis and secretion in the perirenal depot to systemic leptin concentrations. Relatively lower leptin secretion from this or other visceral fat depots may have an important impact, however, on the paracrine or hepatic regulation of lipid metabolism and insulin sensitivity [1–3].
This study highlights that the transition from the hypoglycaemic, hypoinsulinaemic environment of fetal life to the higher glucose and insulin environment of postnatal life represents a critical period during which the availability of circulating insulin and FFAs may determine the future adipogenic and lipogenic capacity of the visceral adipocyte. These data suggest that the early nutrition and insulin environment may be important during the in utero period in the human given that there is development of both the visceral and subcutaneous fat depots in human fetuses before birth, and also during the transition that occurs from placental to enteral nutrition at birth. Further work is required to determine the relationship between circulating insulin and FFAs in cord blood samples or during the immediate postpartum period on the development of visceral fat beyond the first month of life.
IUGR, liver growth and metabolic development
In the rat, IUGR induced by bilateral uterine artery ligation in late pregnancy results in fasting hyperglycemia and hyperinsulinemia in later life [51, 52]. In this model peroxisome proliferator-activated receptor gamma, coactivator 1 alpha (PGC1α) is increased in the livers of the offspring at birth and at 21 days of life [52]. PGC1α is a transcriptional coactivator of nuclear receptors that control expression of gluconeogenic enzymes including glucose-6-phosphatase and phosphoenolpyruvate carboxykinase 2 (PEPCK) [53]. In rats, dexamethasone administration in the third week of pregnancy, also results in a permanent upregulation of hepatic PEPCK mRNA expression and activity and exposure to excess glucocorticoids have therefore been implicated in the prenatal programming of glucose intolerance after prenatal substrate restriction [54]. Thus, hepatic growth and development is altered by exposure to early under-nutrition and/or excess glucocorticoids in a species in which organogenesis and rapid cellular proliferation occurs in the liver in late gestation and early postnatal life. Relatively few studies, however, have investigated the impact of poor fetal substrate supply on hepatic development in species such as the sheep, in which the period of rapid hepatocyte proliferation and liver growth occurs during early pregnancy.
In a range of studies using the placental restriction model of IUGR, we have found that whilst relative fetal liver weight tends to decrease as fetal weight decreases, the liver growth response in IUGR fetal sheep is variable, with relative liver weights ranging between 12 g/kg and 25 g/kg at a fetal body weight of ~3 kg in late gestation (term = 150 ± 3 days’ gestation) [23, 55]. This suggests that there may be different intrahepatic responses to fetal substrate restriction and that some of these responses may act to protect liver growth. In those IUGR fetuses in which liver growth was maintained, the hepatic expression of the insulin-independent glucose transporter, GLUT1, was increased, there was no decrease in IGF1 mRNA expression, and there was no stimulation of either PGC1α and PEPCK mRNA expression [55]. In contrast, in those IUGR fetuses in which liver growth was decreased, there was a decrease in hepatic IGF1 mRNA expression and an upregulation of hepatic 11 β hydroxysteroid dehydrogenase-1 (11βHSD1), PGC1α and PEPCK mRNA expression compared with control fetuses or with IUGR fetuses in which liver growth was not reduced [55].
GLUT 1 is the predominant fetal glucose transporter that mediates glucose transport into rapidly growing cells and is expressed in relatively high concentrations in fetal tissues compared with the adult [56–59]. One possibility is that in the absence of an increase in hepatic GLUT1 mRNA expression in the IUGR fetus, hypoglycaemia will result in a decrease in hepatic IGF1 mRNA levels and a consequent decrease in liver growth. We have suggested that low hepatic glucose uptake results in the stimulation of increased expression of 11βHSD1, the enzyme that converts cortisone to cortisol in the hepatocyte. Cortisol plays a key role in the upregulation of hepatic PEPCK activity and expression in the late gestation fetus [60, 61] and so the increase in hepatic 11βHSD1 mRNA expression and intra-hepatic cortisol production may lead to an increase in PEPCK mRNA expression.
These results indicate that in a subset of IUGR fetuses, there may be specific intra-hepatic mechanisms that ensure that hepatic IGF1 expression and liver growth are maintained, whereas in a different subset, there is no compensatory increase in hepatic glucose transport and liver growth is sacrificed. These differential patterns of hepatic growth and gene expression in IUGR fetuses may be of potential importance in determining whether there will be programming of glucose intolerance in postnatal life. Thus, in the sheep and in humans, unlike in the rat, there may be intrahepatic responses to fetal substrate restriction that protect the fetus and offspring from decreased liver growth and from a decreased responsiveness to the actions of insulin in postnatal life.
The metabolic legacy of IUGR: mechanisms and interventions
During the past decade there have been a number of mechanistic frameworks proposed to explain the biological basis of the associations observed between birth weight and later health outcomes. In 1992, Hales and Barker coined the term, the “thrifty phenotype” hypothesis—derived from the prior “thrifty genotype” hypothesis [6, 62]. Neel had proposed that “thrifty” genes were selected during evolution at a time when food resources were limited and that they resulted in a “fast insulin trigger”, an enhanced capacity to store fat and an increased risk of insulin resistance and type 2 diabetes [63, 64]. The thrifty phenotype hypothesis, proposed, however, that when the fetal nutritional environment is poor, there is an adaptive response, which optimises the growth of key body organs to the detriment of others and leads to an altered postnatal metabolism, designed to enhance postnatal survival under conditions of poor nutrition. It was proposed that these adaptations only became detrimental when nutrition was more abundant in the postnatal environment than it had been in the prenatal environment [6, 62].
Developmental physiologists and physicians have used the term “programming” to describe the process whereby a stimulus or insult at a sensitive or critical period of development, has long-lasting effects, although it has been proposed that the term “developmental plasticity”, rather than programming, would be more appropriate. Developmental plasticity is defined as “the ability of a single genotype to produce more than one alternative form of structure, physiological state or behaviour in response to environmental conditions” [65]. Bateson and colleagues propose that for individuals whose conditions in fetal life predicted poor adult nutrition, the expected outcomes may be better, when the postnatal environment matches that experienced prenatally and conversely that the individual would be worse off when there is a relative excess of nutrition in postnatal life [65]. This general model is therefore consistent with the original thrifty phenotype hypothesis. Whilst the evolutionary view provides a clear biological framework to understand the importance of the prenatal environment for the continued reproductive success and health of subsequent adult populations [66], it is recognised that not all responses to an adverse prenatal environment may be potentially predictive of the postnatal environment. In small animal models, where organogenesis and growth through cellular hyperplasia occurs during late gestation, exposure to adverse fetal substrate supply will result in the loss of structural units such as nephrons, cardiomyocytes or pancreatic β cells. Such decreases in structural and hence the lifelong functional capacity of an organ system may represent an inadvertent “teratogenic” consequence of a decrease in energy supply rather than a selective trade-off evoked to maintain the development of more important tissues, such as the brain. At this stage it is not clear that such responses are either “adaptive” or “predictive”, although it is clear that they will result in the programming of a reduced functional capacity for life.
There has also been intense recent interest in the role of epigenetic modification of key genes in the association between IUGR and the development of insulin resistance. Epigenetics refers to covalent modifications of DNA and core histones that regulate gene activity without altering the nucleotide sequence of DNA [67]. The best characterised epigenetic modification of DNA is the methylation of cytosine residues within CpG dinucleotides and it has been demonstrated that early nutrition may influence the establishment and maintenance of cytosine methylation [67]. Recently, there has also been specific interest in the role of microRNAs (miRNAs), a novel group of small non-coding RNAs in the pathology of diabetes [68] and future work on the role of specific miRNAs in the developmental programming of insulin resistance will be of particular interest in this field.
In summary, the concept of the thrifty phenotype [62] has been of seminal value in highlighting that it is the fetal adaptive response to a suboptimal nutritional environment and the consequent nutritional mismatch between the resulting phenotype and the postnatal nutritional environment, which results in adverse consequences for metabolic health. It is now becoming apparent from large animal models of IUGR that the early insulin environment and the intracellular availability of free fatty acids and glucose in the visceral adipocyte, skeletal muscle cell and hepatocyte are important in determining the metabolic phenotype of these cells in the IUGR offspring. These studies therefore provide key insights into the potential benefits and possible adverse consequences of different types of nutritional interventions in the IUGR neonate.
References
McMillen IC, Robinson JS (2005) Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiol Rev 85:571–633
Stocker CJ, Cawthorne MA (2008) The influence of leptin on early life programming of obesity. Trends Biotechnol 26:545–551
Briana DD, Malamitsi-Puchner A (2009) Intrauterine growth restriction and adult disease: the role of adipocytokines. Eur J Endocrinol 160:337–347
Evans SC (2009) Nutritional programming of disease: unravelling the mechanism. J Anat 215:36–51
Yajnik CS (2009) Nutrient-mediated teratogenesis and fuel-mediated teratogenesis: two pathways of intrauterine programming of diabetes. Int J Gynaecol Obstet 104 [Suppl 1]:S27–S31
Hales C, Barker D (1992) Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia 135:595–601
Economides DL, Nicolaides KH, Campbell S (1991) Metabolic and endocrine findings in appropriate and small for gestational age fetuses. J Perinat Med 19:97–105
Enzi G, Zanardo V, Caretta F, Inelmen EM, Rubaltelli F (1981) Intrauterine growth and adipose tissue development. Am J Clin Nutr 34:1785–1790
Fitzhardinge PM, Steven EM (1972) The small-for-date infant. I. Later growth patterns. Pediatrics 49:671–681
Albertsson-Wikland K, Wennergren G, Wennergren M, Vilbergsson G, Rosberg S (1993) Longitudinal follow-up of growth in children born small for gestational age. Acta Paediatr 82:438–443
Curhan GC, Willett WC, Rimm EB, Spiegelman D, Ascherio AL, Stampfer MJ (1996) Birth weight and adult hypertension, diabetes mellitus and obesity in US men. Circulation 94:3246–3250
Whincup PH, Cook DG, Adshead F, Taylor SJ, Walker M, Papacosta O, Alberti KG (1997) Childhood size is more strongly related than size at birth to glucose and insulin levels in 10–11-year-old children. Diabetologia 40:319–326
Bavdekar A, Yajnik C, Fall C, Bapat S, Pandit A, Deshpande V, Bhave S, Kellingray S, Joglekar C (1999) Insulin resistance syndrome in 8-year-old Indian children: small at birth, big at 8 years, or both? Diabetes 48:2422–2429
Eriksson J, Forsen T, Tuomilehto J, Osmond C, Barker D (2001) Size at birth, childhood growth and obesity in adult life. Int J Obes Relat Metab Disord 25:735–740
Levy-Marchal C, Jaquet D (2004) Long-term metabolic consequences of being born small for gestational age. Pediatr Diabetes 5:147–153
Hietakangas V, Cogen SM (2009) Regulation of tissue growth through nutrient sensing. Annu Rev Genet 43:389–410
Holemans K, Verhaeghe J, Dequeker J, Van Assche FA (1996) Insulin sensitivity in adult female rats subjected to malnutrition during the perinatal period. J Soc Gynecol Investig 3:71–77
Ozanne SE, Wang CL, Coleman N, Smith GD (1996) Altered muscle insulin sensitivity in the male offspring of protein-malnourished rats. Am J Physiol Endocrinol Metab 271:E1128–E1134
Ozanne SE, Olsen GS, Hansen LL, Tingey KJ, Nave BT, Wang CL, Hartil K, Petry CJ, Buckley AJ, Mosthaf-Seedorf L (2003) Early growth restriction leads to down regulation of protein kinase C zeta and insulin resistance in skeletal muscle. J Endocrinol 177:235–241
Ozanne SE, Jensen CB, Tingey KJ, Storgaard H, Madsbad S, Vaag AA (2005) Low birthweight is associated with specific changes in muscle insulin-signaling protein expression. Diabetologia 48:547–552
Jensen CB, Martin-Gronert MS, Storgaard H, Madsbad S, Vaag A, Ozanne SE (2008) Altered PI3-Kinase/Akt signaling in skeletal muscle of young men with low birth weight. PLoS One 3:e3738
Edwards LJ, Simonetta G, Owens JA, Robinson JS, McMillen IC (1999) Restriction of placental and fetal growth in sheep alters fetal blood pressure responses to angiotensin II and captopril. J Physiol 515:897–904
Mc Millen IC, Adams MB, Ross JT, Coulter CL, Simonetta G, Owens JA, Robinson J, Edwards LJ (2001) Fetal growth restriction: adaptations and consequences. Reproduction 122:195–204
Morrison JL, Botting KJ, Dyer JL, Williams SJ, Thornburg KL, McMillen IC (2007) Restriction of placental function alters heart development in the sheep fetus. Am J Physiol Regul Integr Comp Physiol 293:R306–R313
Morrison JL (2008) Sheep models of intrauterine growth restriction: fetal adaptations and consequences. Clin Exp Pharmacol Physiol 35:730–743
Muhlhausler BS, Duffield JA, Ozanne SE, Pilgrim C, Turner N, Morrison JL, McMillen IC (2009) The transition from fetal growth restriction to accelerated postnatal growth: a potential role for insulin signaling in skeletal muscle. J Physiol 587:4199–4211
De Blasio MJ, Gatford KL, McMillen IC, Robinson JS, Owens JA (2006) Placental restriction of fetal growth increases insulin action, growth and adiposity in the young lamb. Endocrinology 148:1350–1358
Beltrand J, Nicolescu R, Kaguelidou F, Verkauskiene R, Sibony O, Chevenne D, Claris O, Lévy-Marchal C (2009) Catch-up growth following fetal growth restriction promotes rapid restoration of fat mass but without metabolic consequences at one year of age. PLoS One 4:e5343
Hediger ML, Overpeck MD, Kuczmarski RJ, McGlynn A, Maurer KR, Davis WW (1998) Muscularity and fatness of infants and young children born small- or large-for-gestational-age. Pediatrics 102:e60
Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB (2000) Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ 320:967–971
Law CM, Barker DJ, Osmond C, Fall CH, Simmonds SJ (1992) Early growth and abdominal fatness in adult life. J Epidemiol Community Health 46:184–186
Parsons TJ, Power C, Manor O (2001) Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study. BMJ 323:1331–1335
Yuen BS, McMillen IC, Symonds ME, Owens PC (1999) Abundance of leptin mRNA in fetal adipose tissue is related to fetal body weight. J Endocrinol 163:R11–R14
Yuen BS, Owens PC, McFarlane JR, Symonds ME, Edwards LJ, Kauter KG, McMillen IC (2002) Circulating leptin concentrations are positively related to leptin messenger RNA expression in the adipose tissue of fetal sheep in the pregnant ewe fed at or below maintenance energy requirements during late gestation. Biol Reprod 67:911–916
Yuen BSJ, Owens PC, Muhlhausler BS, Roberts CT, Symonds ME, Keisler DH, McFarlane JR, Kauter KG, Evens Y, McMillen IC (2003) Leptin alters the structural and functional characteristics of adipose tissue before birth. FASEB J 17:1102–1104
Duffield JA, Vuocolo T, Tellam R, Yuen BS, Muhlhausler BS, McMillen IC (2008) Placental restriction of fetal growth decreases IGF1 and leptin mRNA expression in the perirenal adipose tissue of late gestation fetal sheep. Am J Physiol Regul Integr Comp Physiol 294:R1413–R1419
Greenwood PL, Hunt AS, Hermanson JW, Bell AW (1998) Effects of birth weight and postnatal nutrition on neonatal sheep. I. Body growth and composition, and some aspects of energetic efficiency. J Anim Sci 76:2354–2367
Poore KR, Fowden AL (2004) The effects of birth weight and postnatal growth patterns on fat depth and plasma leptin concentrations in juvenile and adult pigs. J Physiol 558:295–304
Louey S, Cock ML, Harding R (2005) Long term consequences of low birthweight on postnatal growth, adiposity and brain weight at maturity in sheep. J Reprod Dev 51:59–68
Holzenberger M, Hamard G, Zaoui R, Leneuve P, Ducos B, Beccavin C, Perin L, Le Bouc Y (2001) Experimental IGF-1 receptor deficiency generates a sexually dimorphic pattern of organ-specific growth deficits in mice, affecting fat tissue in particular. Endocrinology 142:4469–4478
Gregoire FM, Smas CM, Sul HS (1998) Understanding adipocyte differentiation. Physiol Rev 78:783–809
Lefterova MI, Lazar MA (2009) New developments in adipogenesis. Trends Endocrinol Metab 20:107–114
Aouadi M, Laurent K, Prot M, Le Marchand-Brustel Y, Binetruy B, Bost F (2006) Inhibition of p38MAPK increases adipogenesis from embryonic to adult stages. Diabetes 55:281–289
Picard F, Auwerx J (2002) PPAR (gamma) and glucose homeostasis. Annu Rev Nutr 22:167–197
Jaquet D, Gaboriau A, Czernichow P, Levy-Marchal C (2001) Relatively low serum leptin levels in adults born with intra-uterine growth retardation. Int J Obes Relat Metab Disord 25:491–495
Leger J, Limoni C, Collin D, Czernichow P (1998) Prediction factors in the determination of final height in subjects born small for gestational age. Pediatr Res 43:808–812
Duffield JA, Vuocolo T, Tellam R, McFarlane JR, Kauter KG, Muhlhausler BS, McMillen IC (2009) Intrauterine growth restriction and the sex specific programming of leptin and peroxisome proliferator-activated receptor gamma (PPARgamma) mRNA expression in visceral fat in the lamb. Pediatr Res 66:59–65
Sampath H, Ntambi JM (2005) Polyunsaturated fatty acid regulation of genes of lipid metabolism. Annu Rev Nutr 25:317–340
Ailhaud G, Amri EZ, Grimaldi PA (1995) Fatty acids and adipose cell differentiation. Prostaglandins Leukot Essent Fatty Acids 52:113–115
He W, Barak Y, Hevener A, Olson P, Liao D, Le J, Nelson M, Ong E, Olefsky JM, Evans RM (2003) Adipose-specific peroxisome proliferator-activated receptor gamma knockout causes insulin resistance in fat and liver but not in muscle. Proc Natl Acad Sci USA 100:15712–15717
Simmons RA, Templeton LJ, Gertz SJ (2001) Intrauterine growth retardation leads to the development of type 2 diabetes in the rat. Diabetes 50:2279–2286
Lane RH, MacLennan NK, Hsu JL, Janke SM, Pham TD (2002) Increased hepatic peroxisome proliferator-activated receptor-γ coactivator-1 gene expression in a rat model of intrauterine growth retardation and subsequent insulin resistance. Endocrinology 143:2486–2490
Yoon JC, Puigserver P, Chen G, Donovan J, Wu Z, Rhee J, Adelmant G, Stafford J, Kahn CR, Granner DK, Newgard CB, Spiegelman BM (2001) Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature 413:131–138
Nyirenda MJ, Lindsay RS, Kenyon CJ, Burchell A, Seckl JR (1998) Glucocorticoid exposure in late gestation permanently programs rat hepatic phosphoenolpyruvate carboxykinase and glucocorticoid receptor expression and causes glucose intolerance in adult offspring. J Clin Invest 101:2174–2181
Gentili S, Morrison JL, McMillen IC (2009) Intrauterine growth restriction and differential patterns of hepatic growth and expression of IGF1, PCK2, and HSDL1 mRNA in the sheep fetus in late gestation. Biol Reprod 80:1121–1127
Postic C, Leturque A, Printz P, Maulard M, Loizeau M, Granner DK, Girard J (1994) Development and regulation of glucose transporter and hexokinase expression in rat. Am J Physiol 266:E548–E559
Santalucia T, Camps M, Castello A, Munoz P, Nuel A, Testar X, Palacin M, Zorzano A (1992) Developmental regulation of GLUT-1 (erythroid/Hep G2) and GLUT-4 (muscle/fat) glucose transporter expression in rat heart, skeletal muscle, and brown adipose tissue. Endocrinology 130:837–846
Werner H, Adamo M, Lowe WLJ, Roberts CTJ, LeRoith D (1989) Developmental regulation of rat brain/Hep G2 glucose transporter gene expression. Mol Endocrinol 3:273–279
Leturque A, Postic C, Ferre P, Girard J (1991) Nutritional regulation of glucose transporter in muscle and adipose tissue of weaned rats. Am J Physiol 260:E588–E593
Forhead AJ, Poore KR, Mapstone J, Fowden AL (2003) Developmental regulation of hepatic and renal gluconeogenic enzymes by thyroid hormones in fetal sheep during late gestation. J Physiol 548:941–947
Franko KL, Giussani DA, Forhead AJ, Fowden AL (2007) Effects of dexamethasone on the glucogenic capacity of fetal, pregnant, and non-pregnant adult sheep. J Endocrinol 192:67–73
Hales CN, Barker DJP (2001) The thrifty phenotype hypothesis. Br Med Bull 60:5–20
Neel JV (1962) Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet 14:353–362
Neel JV (1999) The “thrifty genotype” in 1998. Nutr Rev 57:S2–S9
Bateson P, Barker D, Clutton-Brock T, Debal D, D'Udine B, Foley R, Gluckman P, Godfrey K, Kirkwood T, Lahr M, McNamara J, Metcalfe N, Monaghan P, Spencer H, Sultani S (2004) Developmental plasticity and human health. Nature 430:419–421
Gluckman PD, Hanson MA (2004) The developmental origins of the metabolic syndrome. Trends Endocrinol Metab 15:183–187
Waterland RA, Jirtle RL (2004) Early nutrition, epigenetic changes at transposons and imprinted genes, and enhanced susceptibility to adult chronic diseases. Nutrition 20:63–68
Pandey AK, Agarwal P, Kaur K, Datta M (2009) MicroRNAs in diabetes: tiny players in big disease. Cell Physiol Biochem 23:221–232
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morrison, J.L., Duffield, J.A., Muhlhausler, B.S. et al. Fetal growth restriction, catch-up growth and the early origins of insulin resistance and visceral obesity. Pediatr Nephrol 25, 669–677 (2010). https://doi.org/10.1007/s00467-009-1407-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1407-3