Abstract
Infants with chronic renal failure (CRF) are at high risk of experiencing severe growth retardation. We report a study of 12 infants with CRF who have been treated with recombinant human growth hormone (rhGH) since the age of 0.5 ± 0.3 years. A control group comprised 15 infants with less severe CRF who were being treated during the same period, but who did not receive rhGH. Despite the infants in the rhGH group had more severe renal failure, they grew at least as well as those in the control group and experienced catch-up growth that started earlier and was more sustained; they also gained more weight. Between the age of 0.5 and 2.5 years, the height standard deviation score (HtSDS) improved from −2.0 ± 1.2 to −0.9 ± 0.9 in the rhGH group (p < 0.005) and from −1.6 ± 1.6 to −1.0 ± 1.9 in the control group (p=non significant, n.s.). The average gain in HtSDS was +1.1 ± 0.8 in the treated group and +0.6 ± 1.4 in the control group (p = n.s.). During the same period, the weight SDS improved from −2.2 ± 0.9 to −0.6 ± 1.2 (p < 0.005) and from −1.9 ± 1.2 to −1.3 ± 1.2 (p=n.s.) in the treatment and control groups, respectively. Nutritional intake was similar in both groups, while parathyroid hormone levels tended to increase, although not significantly, after rhGH treatment (p=n.s.). The results of this pilot study suggest that very early treatment with rhGH in patients with early-onset CRF may improve growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impairment of longitudinal growth is a severe complication of chronic renal failure (CRF) in childhood [1, 2]. The etiology of growth failure in this population is multifactorial, reflecting both abnormalities in the growth hormone/insulin-like growth factor-1 (GH/IGF-1) axis, decreased nutrition intake and metabolic disturbances [3]. To grow, these children require an aggressive medical treatment that includes a maximization of nutrition, prompt correction of metabolic acidosis, prevention of renal osteodystrophy and hyperparathyroidism, correction of anemia and salt supplementation as needed [3]. Despite all these efforts, a substantial number of children remain significantly growth-retarded [4, 5].
Several studies have documented that recombinant human growth hormone (rhGH) therapy promotes catch-up growth [1, 6–9]. Infants suffering from CRF from their first months of life are at an especially high risk of growth failure and long-term growth retardation because the first years of life correspond to a period of maximal growth velocity [1, 10, 11]. Such children are often growth retarded by 2–3 standard deviation scores at the age of 1 year and do not experience a significant catch-up growth during subsequent years [4, 5, 12, 13]. As growth is not considered to be dependent on the GH/IGF-1 axis during the first 2 years of life, most efforts in infants are directed at optimizing the nutrition intake, while rhGH therapy is usually initiated later. This conservative management, if started quickly, can limit and sometimes prevent growth retardation [3]. In this retrospective study, we report our experience in initiating rhGH treatment during the first year of life in infants with early-onset of CRF.
Methods
Patient selection criteria and data collection
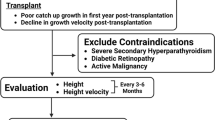
All infants with CRF or end stage renal disease (ESRD) who have been followed at the Bambino Gesù Children’s Hospital for at least 2.5 years of age and have began treatment with rhGH before their first birthday were included in this study. Patient characteristics are reported in Table 1.
Following parental consent, rhGH was started in seven patients with a height standard deviation score (HtSDS) lower than −2. Four patients had a HtSDS ranging between −1.2 and −2 when they began rhGH treatment, but three of these had lost more than 1 HtSDS and one had lost 0.6 HtSDS in less then 3 months, despite adequate caloric intake through a nasogastric tube. They were therefore rapidly falling below the third percentile for height. One patient with a severe form of oxalosis began rhGH treatment with a HtSDS of −0.5. Treatment was started in this patient in an attempt to maximize growth so that the child would rapidly achieve a suitable size for combined kidney and liver transplantation.
To generate a control group, we selected all children with a creatinine clearance < 50 ml/min per 1.73 m2 at 1 year of life who had been followed at our institution during the same time period but who had not received rhGH treatment.
Medical records were reviewed retrospectively. Data collection included growth parameters, nutrition, renal function, biochemical analyses, thyroid function, treatment and complications. Data were collected on the patient cohort up to the age of 5 years or up to the age of transplantation, if patients were transplanted before their fifth birthday.
Most patients have been followed on a monthly basis. Some patients, with a milder degree of CRF, were followed every 2 months.
Parents were instructed to bring a 24-h record of their child’s nutritional intake to each visit to the outpatient clinic to enable the clinician to calculate the caloric and protein intake. At each outpatient visit, energy and proteins intake were assessed by a dietitian. Data are expressed as percentage of the recommended dietary allowance (RDA) [14]. The diet was modified with the aim of achieving an optimal intake of 120% of the RDA.
rhGH was administered by daily subcutaneous injections and prescribed at a target dose of 0.35 mg/kg per week [2]. The dose was adjusted according to weight every 3 months. The rhGH is currently licensed in Italy for the use in growth-retarded patients with CRF, without age limitations.
Thyroid function was evaluated in all patients during the follow-up and at the beginning of rhGH therapy. When needed, thyroxine treatment was prescribed to maintain thyroid stimulating hormone (TSH) levels within the normal range.
Data elaboration and synchronization
Height, weight and weight for height data were expressed as standard deviation scores (SDS) using the age- and gender-specific reference values of the Center for Disease Control (CDC) [15]. Chronological age was corrected for gestational age for infants born prematurely. Bone age was estimated by a single radiologist using the Greulich and Pyle reference atlas [16]. All data were tabulated at 3-month intervals. A maximum gap of 3 weeks with the effective age of measurement was tolerated.
Growth data are reported up to 3 years of age, because after this age a significant number of patients had received transplants or had not completed a 5-year follow-up.
To further analyze the effects of rhGH on protein and caloric intake and on calcium–phosphate metabolism, we synchronized data at the beginning of rhGH treatment. The median age of initiation of rhGH (6 months) was used to compare synchronized data collected in the control group. Creatinine clearance was calculated with the Schwartz formula, using a k value of 0.48 [17]. For patients on dialysis, a value of 5 ml/min per 1.73 m2 was arbitrary assumed to account for possible residual renal function and dialysis clearance.
Statistical analysis
Statistical analysis was performed using SPSS for Windows ver. 8.0 software (SPSS, Chicago, IL) and Stata 9.0 software (StataCorp LP, College Station, TX). Categorical data were compared using the Fisher’s exact test. Data were tested for normality with the Kolmogorov–Smirnov and the Shapiro–Wilk tests. Data that passed the normality tests are represented in figures as the mean ± SD. Due to the small sample number, comparisons within groups were performed using the Wilcoxon signed-rank test, and comparisons between groups were performed with the Mann–Whitney U test. Repeated measurements between groups were compared with the two-sample Hotelling T-square test. All tests were two-sided, and results were considered significant at a p level < 0.05.
Results
Characteristics of the study populations
Patient characteristics are reported in Table 1. Between 1998 and 2005, 38 patients were treated for early-onset CRF, 12 of whom received rhGH before the age of 1 year. Of the remaining patients, 15 did not receive rhGH in the first 3 years of life, and these were selected as controls for our study. The two groups did not differ in terms of gender, gestational age, birth weight, duration of follow-up, and type of renal disease (Table 1).
The main diagnoses were bilateral renal (hypo)dysplasia, posterior urethral valves, bilateral reflux with renal dysplasia, and autosomal recessive polycystic kidney disease (ARPKD). Other diagnoses included cortical necrosis, focal segmental glomerular sclerosis, diffuse extracapillary proliferative glomerulonephritis, and type I oxalosis.
All patients with growth retardation were started on enteral feeding. As they began to catch up on growth, parents often discontinued this feeding modality. Enteral feeding through a nasogastric tube was used for more then 6 months during the first year of life more frequently in the rhGH group than the control group, but the differences between the two groups did not reach statistical significance. Three patients in the rhGH group continued nasogastric feeding for more then 18 months. No patient was fed with a gastrostomy tube.
Renal function was worse in the treatment group, as indicated by differences in creatinine clearances and in the proportion of patients on dialysis between the two groups (Table 1).
At the last follow-up, seven of the 12 patients in the rhGH group had been successfully transplanted. Two patients in the control group received a transplant at an older age.
Co-morbidity conditions, such as infections and surgical procedures, were recorded as these can significantly hamper growth in infants and small children with CRF. No statistical differences were found between the two groups, with the exception of the number of peritonitis episodes, which was higher in the rhGH group as this group included more patients treated with peritoneal dialysis (p < 0.001). The acid–base equilibrium was also assessed. With few exceptions, all patients were well equilibrated during the entire duration of the study, with serum bicarbonate levels ≥ 20 mEq/l (data not shown).
The actual dose of rhGH was 0.24 ± 0.07 mg/kg per week, indicating that the target dose of 0.35 mg/kg per week was not achieved in a significant number of patients. Closer analysis of this result indicates that adjustment of the rhGH dose on a 3-month basis was, in part, inadequate because growth velocity in this age range is elevated, and patients tended to become rapidly under-dosed as they gained weight. In addition, the dose was not increased regularly in several patients because they developed significant hyperparathyroidism (see below).
Growth data
As shown in Fig. 1, both groups of patients showed significant growth retardation in the first months of life. Overall, children treated with rhGH reached a slightly higher HtSDS at 3 years of age, despite more severe renal failure and lower HtSDS at 6 months of age (Fig. 1a). These differences did not reach statistical significance (non significant, n.s.). By 3 years of age, the mean HtSDS was lower by approximately 1 SDS in both groups.
Height and weight data. Recombinant human growth hormone (rhGH)-treated patients are shown in black lines and controls in gray lines. Vertical bars indicate the age at the beginning of rhGH therapy in individual patients. a Height standard deviation score (SDS), b growth velocity expressed as relative values to the −2 SDS channel for the normal population, c weight SDS, d weight for height SDS. Numbers indicate number of infants/children for which there were data at that time point
Between the age of 6 months, which corresponds to the median age of rhGH initiation, and the age of 2.5 years, HtSDS improved from – 2.0 ± 1.2 to −0.9 ± 0.9 in the rhGH group (p < 0.005) and from −1.6 ± 1.6 to −1.0 ± 1.9 in the control group (p=n.s.). The average gain in HtSDS was +1.1 ± 0.8 in the treated group and +0.6 ± 1.4 in the control group (p=n.s.).
As growth velocity decreases by more than sixfold during the first 3 years of life, velocity data were expressed as relative values, using the –2 SDS channel as a reference (Fig. 1b). Values < 1 indicate a loss of HtSDS while values > 1 indicate a gain in HtSDS (catch-up growth), in comparison to children who are growing along the lower limit of normal values. As shown in Fig. 1b, infants in the treatment group began their catch-up growth earlier (6.2 ± 2.1 months) than those in the control group (11.4 ± 3.0 months). These differences reached statistical significance (p < 0.03). It should be noted, however, that at 6 months of age only six of the 12 patients in the treatment group had started rhGH therapy and that several patients in both groups showed an irregular growth pattern during the first year of life, with periods of loss and periods of gain in HtSDS; both these factors limit the accuracy of this parameter when assessed in individual patients.
Children receiving rhGH treatment also gained more weight (Fig. 1c). As the gain in weight SDS (WtSDS) was higher than the gain in HtSDS, patients treated with rhGH were slightly overweight by the age of 3 years, while control patients were slightly underweight (Fig. 1d). From 6 months to 2.5 years of age, the WtSDS improved from −2.2 ± 0.9 to −0.6 ± 1.2 (p< 0.005) and from −1.9 ± 1.2 to −1.3 ± 1.2 (p = n.s.) in the treatment and control groups, respectively. The average weight gain was significantly higher in rhGH-treated patients (+1.52 ± 1.2) than in non-treated patients (+0.42 ± 1.3) (p < 0.02).
Nutrition
Overall, the caloric and protein intake were slightly higher in the rhGH group, but differences between the groups did not reach statistical significance (Fig. 2a, b).
Nutrition and calcium–phosphate metabolism. All data were synchronized at the beginning of rhGH therapy. a, b Caloric and protein intake expressed as a percentage of the recommended daily dose (RDA) (mean ± SD), c parathyroid hormone (PTH) levels. The mean (±SD) dose of vitamin D is indicated at the top of the panel (μg/kg per day). Filled circles rhGH-treated patients, open circles control patients, horizontal bars median PTH level d serum calcium and serum phosphate levels (mean ± SD)
Bone age
Bone age was measured between the ages of 1 and 3 years in eight patients treated with rhGH and in seven control patients. These measurements were repeated at 1-year intervals in five patients in the rhGH group and in three control children. Overall, bone age was marginally retarded by 2.0 ± 3.1 months at a mean chronological age of 1.8 ± 0.8 years in the rhGH group and by 3.5 ± 2.0 months at a mean chronological age of 2.0 ± 0.4 years in controls. In the five rhGH-treated patients in whom repeated measurements were available, we observed no trend towards an acceleration of bone age, however, the number of observations were too small to draw conclusions. No rickets lesions were observed.
Parathyroid hormone, vitamin D, calcium, phosphate
Parathyroid hormone (PTH) tended to increase after the initiation of rhGH therapy (Fig. 2c), although not significantly. During the first 24 months of treatment, four of the 12 treated patients had PTH levels > 500 pg/ml, as opposed to one patient in the control group. Physicians taking care of patients responded to increased PTH levels by increasing the dose of 1,25(OH)2vitamin D during the first 6 months of hormonal treatment (from 0.028 ± 0.011 to 0.041 ± 0.017 μg/kg per day, p < 0.05). After 1 year of treatment, the dose of vitamin D was not different from that in the pre-treatment period. Serum calcium and phosphate levels were well controlled in the majority of patients (Fig. 2d). Three patients in the treatment group had serum phosphate levels above the upper limit for the age at any one point during the follow-up.
Thyroid function
Four rhGH-treated patients and one control patient received L-thyroxine. These patients were all treated with peritoneal dialysis. In one rhGH-treated patient, TSH levels remained elevated (7.4–10.0 μIU/ml) until the age of 18 months. The other three patients had normal TSH levels (1.94 ± 0.36 μIU/ml) under thyroxine treatment. Free triiodothyronine (FT3; 4.51 ± 1.13 pg/ml) and free thyroxine (FT4; 1.49 ± 0.76 ng/dl) levels were within the normal range in all patients, and no patient experienced sustained hypothyroidism during the study period.
Serum glucose
Non-fasting serum glucose levels were measured at every outpatient visit and were similar before (96.3 mg/dl, range 76–115 mg/dl) and after (89.2 mg/dl, range 56–120 mg/dl) rhGH treatment (p=n.s.). Glycosylated hemoglobin and glucose tolerance tests were not routinely performed.
Discussion
This study is one of the first to report clinical experience with rhGH treatment of infants with early onset CRF during their first year of life. Although a small number of infants were treated during the first year of life in one other study, the data were included and analyzed with a larger cohort of older children [18].
While the data reported here are clearly limited by its retrospective nature of the study and the small number of patients, they do indicate that treated patients grew at least as well as the non-treated ones despite a higher incidence of more severe chronic renal failure and higher, although not statistically different, growth retardation in the first months of life. The lower HtSDS at the beginning of treatment, however, may have promoted a more sustained catch-up growth in the rhGH group.
Altogether, our patients were less growth retarded than those with the same degree of renal failure who participated in the European multicenter study for nutritional treatment of CRF in childhood, which was performed between 1970 and 1992 [12]. These differences most likely reflect improvements in nutritional and medical care during the past decades. We have therefore avoided using historical controls and have preferred to select a control group that was treated during the same time period, at the expenses of incomplete matching for growth retardation and renal impairment. Nutritional data, infection episodes, and surgical procedures, which are known to be associated with growth stunting, were reported in all patients and analyzed.
Fine et al. reported their experience with a group of children with a renal function similar to our control group, with most of the group being treated with rhGH after the first year of life [18]. The HtSDS improved with rhGH treatment from −3.0 ± 0.9 to −1.1 ± 1.0 over a 2-year period, while non-treated patients failed to demonstrate significant catch-up growth. Here again, differences with our study may be related to the period where their study was performed.
Kari et al. reviewed a group of infants with early-onset CRF between 1986 and 1998 [19]. None received early rhGH treatment. At 6 months of age their cohort had a mean renal function and HtSDS similar to our rhGH-treated group. However, data comparison between these two studies is difficult and of limited significance. In addition, patients in the study by Kari et al. were subdivided according to the stage of renal failure. With these limitations, our rhGH-treated infants seem to have grown somewhat better than the children on conservative management reported by Kari et al. and similarly to their children treated with dialysis and aggressive enteral feeding [19]. Specifically, 89% of their patients were enterally fed for a mean duration of 2 years, 44% had a gastrostomy and in 22% a Nissen fundoplication was performed [19]. In comparison, 58% of our patients received enteral feedings for more then 6 months, mostly during the first year of life. In this respect, one of the benefits of early rhGH therapy may have been to promote growth without the need of very aggressive dietary therapies. Most patients in our cohort had appropriate caloric and protein intake.
Our rhGH-treated patients gained more weight with respect to their linear growth and actually became moderately overweight. Several of these children were oligoanuric and treated with peritoneal dialysis, which may have been associated with fluid retention and increased weight. Conversely, a significant number of patients in the control children had polyuric congenital kidney diseases, which may have been associated with decreased total body water and lower weight. Thus, we are unable at this time to provide a clear interpretation of the weight gain under rhGH therapy.
Assuming that rhGH improves statural growth by 1 HtSDS in 3 years, we have estimated that our treated children have reached a suitable height for transplantation approximately 5 months earlier that they would have without treatment. In balancing the costs and benefits of early rhGH treatment, this point should be taken into account, including the complications and the costs of chronic peritoneal dialysis. In addition, the cost of rhGH in these patients is relatively low because of the lower body weight of this age group.
We did not record any malignancies, bone abnormalities, pseudotumor cerebri, or hyperglycemia after rhGH treatment [20], but we also did not investigate in depth the effects of rhGH on muscle strength, body composition, bone metabolism, and neurodevelopment. Our data do not suggest that rhGH accelerates the progression of renal failure or bone maturation. The number of children and their follow-up are clearly too limited and short, respectively to draw any definitive conclusion.
The most disturbing side effect is related to the development of overt hyperparathyroidism in a substantial number of patients. Here again, the numbers are too small to draw definitive conclusions, but hyperparathyroidism was the primary reason for not adjusting at regular intervals the rhGH dose to the target dose of 0.35 mg/kg per week (the mean dose over the entire study period was 0.24 ± 0.07 mg/kg per week).
Increased serum PTH levels after rhGH therapy has previously been reported, especially in fast-growing pubertal uremic patients [21–23]. Likewise, the first 2 years of life are characterized by high growth velocity, suggesting that similar mechanisms apply also to infants with CRF.
In the past, high PTH levels often prompted physicians to increase the dose of 1,25(OH)2vitamin D supplementation during the first 6 months of treatment as a means of controlling hyperparathyroidism. Recent studies, however, have drawn attention to the risk of vascular calcification in uremic and transplanted children. This risk has been related to high [calcium × phosphate] production, high PTH levels, and elevated 1,25(OH)2vitamin D dosages [24–26]. In our view, this risk constitutes the major factor in advocating the use of rhGH in infants with CRF. New drugs, such as calcimimetics, may represent new strategies for controlling hyperparathyroidism in these patients, as data in children are now becoming available [27, 28].
In conclusion, this is one of the first reports on the use of rhGH in infants with CRF from the first year of life onwards. Our data suggest that early hormonal treatment may accelerate catch-up growth, allowing transplantation at an earlier age. The only apparent side effect was a tendency to develop hyperparathyroidism, which required treatment with increased doses of 1,25(OH)2vitamin D. This study has a number of distinct limitations, including its retrospective nature, the small number of patients, a lack of randomization, and incomplete matching with the control group.
References
Haffner D, Schaefer F, Nissel R, Wühl E, Tönshoff B, Mehls O (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. German study group for growth hormone treatment in chronic renal failure. N Engl J Med 343:923–930
Mahan JD, Warady BA (2008) Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol 21:917–930
Mahesh S, Kaskel F (2008) Growth hormone axis in chronic kidney disease. Pediatr Nephrol 23:41–48
Kleinknecht C, Broyer M, Huot M, Marti-Henneberg C, Dartois AM (1983) Growth and development of nondialyzed children with chronic renal failure. Kidney Int 24[Suppl 15]:S40–S47
Rees L, Rigden SPA, Ward GM (1989) Chronic renal failure and growth. Arch Dis Child 64:573–577
Fine RN, Kohaut E, Brown D, Kuntze J, Attie KM (1996) Long-term treatment of growth retarded children with chronic renal insufficiency, with recombinant human growth hormone. Kidney Int 49:781–785
Vimalachandra D, Craig JC, Cowell CT, Knight JF (2001) Growth hormone treatment in children with chronic renal failure: a meta-analysis of randomized controlled trials. J Pediatr 139:560–567
Maxwell H, Rees L (1996) Recombinant human growth hormone treatment in infants with chronic renal failure. Arch Dis Child 74:40–43
Hokken-Koelega A, Mulder P, De Jong R, Lilien M, Donckerwolcke R, Groothof J (2000) Long-term effects of growth hormone treatment on growth and puberty in patients with chronic renal insufficiency. Pediatr Nephrol 14:701–706
Tonshoff B, Mehls O (1995) Growth retardation in children with chronic renal insufficiency: current aspects of pathophysiology and treatment. J Nephrol 8:133–142
Kaskel F (2003) Chronic renal disease: a growing problem. Kidney Int 64:1141–1151
Karlberg J, Schaefer F, Hennicke M, Wingen AM, Rigden S, Mehls O (1996) Early age-dependent growth impairment in chronic renal failure. European study group for nutritional treatment of chronic renal failure in childhood. Pediatr Nephrol 10:283–287
Van Dyck M, Sidler S, Proesmans W (1998) Chronic renal failure in infants: effect of strict conservative treatment on growth. Eur J Pediatr 157:759–762
Kopple JD, National Kidney Foundation K/DOQI Work Group (2001) The National Kidney Foundation K/DOQI clinical practice guidelines for dietary protein intake for chronic dialysis patients. Am J Kidney Dis 38[Suppl 1]:S68–S73
United States growth charts. National Center for Health Statistics, Center for Disease Control. Available at https://doi.org/www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm
Guerlich WW, Pyle SI (1959) Radiographic atlas of skeletal development of the hand and wrist. Stanford University Press, Stanford, California
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
Fine RN, Attie KM, Kuntze J, Brown DF, Kohaut EC (1995) Recombinant human growth hormone in infants and young children with chronic renal insufficiency: Genentech Collaborative Study Group. Pediatr Nephrol 9:451–457
Kari JA, Gonzalez C, Ledermann SE, Shaw V, Rees L (2000) Outcome and growth of infants with severe chronic renal failure. Kidney Int 57:1681–1687
Fine RN, Ho M, Tejani A, Blethen S (2003) Adverse events with rhGH treatment of patients with chronic renal insufficiency and end-stage renal disease. J Pediatr 142:539–545
Bérard E, Crosnier H, Six-Beneton A, Chevallier T, Cochat P, Broyer M (1998) Recombinant human growth hormone treatment of children on hemodialysis. French Society of Pediatric Nephrology. Pediatr Nephrol 12:304–310
Maxwell H, Rees L (1998) Randomised controlled trial of recombinant human growth hormone in prepubertal and pubertal renal transplant recipients. British association for pediatric nephrology. Arch Dis Child 79:481–487
Picca S, Cappa M, Martinez C, Moges SI, Osborn J, Perfumo F, Ardissino G, Bonaudo R, Montini G, Rizzoni G (2004) Parathyroid hormone levels in pubertal uremic adolescents treated with growth hormone. Pediatr Nephrol 19:71–76
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Civilibal M, Caliskan S, Adaletli I, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Kuruoglu S, Arisoy N (2006) Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol 10:1426–1433
Rees L (2008) What parathyroid hormone levels should we aim for in children with stage 5 chronic kidney disease; what is the evidence? Pediatr Nephrol 23:179–184
Silverstein DM, Kher KK, Moudgil A, Khurana M, Wilcox J, Moylan K (2008) Cinacalcet is efficacious in pediatric dialysis patients. Pediatr Nephrol 23:1817–1822
Muscheites J, Wigger M, Drueckler E, Fischer DC, Kundt G, Haffner D (2008) Cinacalcet for secondary hyperparathyroidism in children with end-stage renal disease. Pediatr Nephrol 23:1823–1829
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mencarelli, F., Kiepe, D., Leozappa, G. et al. Growth hormone treatment started in the first year of life in infants with chronic renal failure. Pediatr Nephrol 24, 1039–1046 (2009). https://doi.org/10.1007/s00467-008-1084-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-1084-7