Abstract
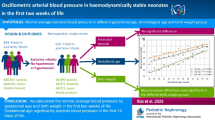
Blood pressure (BP) measurement in the premature neonate is an essential component of neonatal intensive care. Despite significant advances in neonatal care, the data available on BP in the premature neonate are limited. The aim of this study was to determine normative BP measurements for non-ventilated stable premature neonates of gestation age 28–36 weeks in the first month of life using an oscillometric method. Neonates born at 28–36 weeks gestation who did not require ventilation for >24 h or inotrope support for >24 h were enrolled into the study. Blood pressure measurements were taken on days 1, 2, 3, 4, 7, 14, 21 and 28 where possible prior to discharge. A total of 147 infants were included in the study, and 10th and 90th percentiles BPs were obtained for gestation as well as birthweight. Changes in BP over time for each gestational week were determined. A significant difference in BP from day 1 to day 7 and from day 7 to 14 was observed in those born at less than 31 weeks gestation, and from day 1 to 7 in those born at more than 31 weeks gestation, but not from day 14 to 21 and from day 21 to 28 for any gestation period. Data on BP for stable non-ventilated premature infants using an oscillometric method provide useful information for determining hypotension and hypertension in the premature neonate. Premature neonates stabilize their BP after 14 days of life, and at this time they have a BP similar to that of term infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Blood pressure (BP) measurement in the premature neonate is an essential component of neonatal intensive care. It is known to change with gestational age and birth weight and may be affected by a number of clinical situations, including ventilation and continuous positive airway pressure (CPAP). Despite significant advances in neonatal care, the data available on BP of the premature neonate are limited. Many of the studies have only looked at BP during the first hours or days of life [1–5], while in the study of Zubrow et al., the population of neonates was heterogeneous, consisting of those ventilated and on inotropes [6].
Many of the aforementioned studies date from the 1980s and early 1990s. Significant advances have been made in neonatal care since this time, including the administration of antenatal steroids, surfactant, CPAP and methods of BP measurement. Some of the earlier studies of BP in this group of neonates used Doppler ultrasound or intra-arterial assessment [3, 4, 7, 8]. Given these advances, normative BP data, using current oscillometric methods, are required to allow clinicians to appropriately monitor and manage BP in the premature neonate.
The aim of this study was to determine normative BP measurements for non-ventilated stable premature neonates born at 28–36 weeks of gestation during the first month of life.
Methods
Neonates born at more than 27 weeks of gestation who had been admitted to the neonatal intensive care unit were eligible for enrolment. Gestation was determined by the earliest available antenatal ultrasound or last menstrual period if early scans were unavailable. Neonates were excluded if they: (1) required ventilation for longer than 24 h; (2) required inotropes for longer than 24 h; (3) had a congenital or chromosomal anomaly; (4) had a maternal history of illicit substance use (i.e. methadone, heroin, cocaine). The study was approved of by the local Human Research Ethics Committee. Informed consent was obtained from one parent of the neonate.
The data collected included: maternal gravida, parity, smoking, ethnicity, weight at booking visit, BP at booking visit, BP at delivery, antenatal steroid exposure (Celestone 11.4 mg, two doses 24 h apart), type of delivery, Apgar score at 1 and 5 min, birth weight, length, days of CPAP requirement, days of oxygen and days of umbilical arterial catheter (UAC) placement (all UACs are placed between T8–T10 in this institution and are removed if they are not in the correct position).
Blood pressure measurements
Three BP recordings were taken on days 1, 2, 3, 4, 7, 14, 21 and 28 where possible prior to discharge. The BP measurements on day 1 were taken between 12 and 24 h of age to allow for the resolution of fetal circulation. Peripheral BP measurements were taken using an appropriately sized blood pressure cuff (the inflatable portion of the cuff encircling 75% or more of the limb circumference, and the length of the cuff at least two thirds of the length of the upper limb segment from the tip of the shoulder) on an upper limb of an infant in a resting state, awake or asleep. Measurements were taken after the first 12 h of life on the first day, and then between 0900 and 1200 hours for the remaining two measurements on the other days. The BP measurements were taken using the Hewlett Packard Merlin Multiparameter Monitor, neonatal module (Phillips Medical Systems Australasia, Sydney, Australia). BP measurements were taken by the neonatal intensive care unit nursing staff. Values were discarded if there was considerable movement of the infant. Averages of the three systolic, mean and diastolic readings were used for analysis.
Statistical analysis
Data were managed on an SPSS ver. 15.01 database (SPSS, Chicago, IL). Descriptive analyses were carried out to describe the distribution of mean BP readings over a 28-day period for gestation ages ranging from 28 to 36 weeks. General linear models using repeated measures and contrasts (repeated) were performed to determine differences in BP at different time points for gestational ages grouped 28–29 weeks, 30–31 weeks, 32–33 weeks and 34–36 weeks. Given the varying lengths of follow-up, the 28–29 week and 30–31 week groups were compared over 28 days and the 32–33 week and 34–36 week groups compared over 14 days. Graphs were produced using Microsoft Excel ver. 2003 (Microsoft, Seattle, WA).
Results
A total of 147 infants were included in the study, of whom 81 were male (55%) and 66 were female (45%). The majority of infants were Caucasian (97%). Fourteen infants were born at 28 weeks gestation (10%), 18 at 29 weeks (12%), nine at 30 weeks (6%), 24 at 31 weeks (16%), 15 at 32 weeks (10%), 26 at 33 weeks (18%), 20 at 34 weeks (14%), 11 at 35 weeks (8%) and ten at 36 weeks (7%). The demographics of the neonates enrolled are provided in Table 1. Ninety-five (65%) neonates had been exposed to a complete course of antenatal steroids. There were no significant differences in BP readings with and without exposure to antenatal steroids. The 10th, 50th and 90th percentiles of systolic, mean and diastolic BP for gestation on the second day of life are provided in Fig. 1a–c.
Blood pressure and birthweight
The diastolic, mean and systolic BP on day 2 of life and birthweight are provided in Fig. 2. Trends over time suggest that neonates 1500 g or less had a significant linear rise in systolic BP over the first 14 days (F = 36.2, df = 2.72, p < 0.0001), while mean and diastolic BPs tended to stay the same between day 1 and day 7 (F = 2.4, df = 1.36, p = 0.1, and F = 1.1, df = 1.35, p=0.3 respectively) and then significantly increase from day 7 to day 14 (F = 24.6, df = 1.36, p < 0.0001; F = 17.8, df = 1.36, p < 0.0001, respectively). In contrast, neonates weighing 1501–2500 g at birth showed a significant rise in their BP from day 1 to day 7 and then maintained similar BPs from day 7 to day 14. Neonates weighing more than 2500 g at birth experienced significant rises in systolic and mean BPs, but not for diastolic BP, from day 1 to day 7. Too few neonates larger than 2500 g stayed in the study after 7 days for this trend to be studied.
Blood pressure trends over the first 28 days of life
The 10th and 90th percentiles of diastolic, mean and systolic BPs on the 1st, 7th, 14th, 21st and 28th day of life were determined to examine the progressive increase in BP rise for each week of gestational age at birth from 28 to 36 weeks in 2- to 3-week increments (Fig. 3a–d).
a Blood pressure trend in the first 28 days for neonates born at 28–29 weeks gestation. Boxes delineate 10th and 90th percentiles, with black marks delineating range. Green Diastolic BP, red mean BP, blue systolic BP. Purple lines denote median values. b Blood pressure trend in the first 28 days for neonates born at 30–31 weeks gestation. Boxes delineate 10th and 90th percentiles, with black marks delineating range. Green Diastolic BP, red mean BP, blue systolic BP. Purple lines denote median values. c Blood pressure trend in the first 28 days for neonates born at 32–33 weeks gestation. Boxes delineate 10th and 90th percentiles, with black marks delineating range. Green Diastolic BP, red mean BP, blue systolic BP. Purple lines denote median values. d Blood pressure trend in the first 28 days for neonates born at 34–36 weeks gestation. Boxes delineate 10th and 90th percentiles, with black marks delineating range. Green Diastolic BP, red mean BP, blue systolic BP. Purple lines denote median values
Repeated measures general linear models for neonates born at 28–31 weeks gestation over a 28-day period revealed significant differences between the 28–29 week and 30–31 week groups in terms of systolic BP (F = 10.8, df = 1.35, p = 0.002), mean BP (F = 5.8, df = 1.35, p = 0.02) and diastolic BP (F = 4.4, df = 1.35, p = 0.04), with the younger gestation age group tending to have lower average BPs. In terms of trends over time, there were no significant differences between the 28–29 and 30–31 week groups. Based on repeated contrasts, from day 1 to day 7 there was a significant increase in systolic BP (F = 28.2, df = 1.35, p < 0.0001), and mean BP (F =13.5, df = 1.35, p = 0.001), and diastolic BP nearly reached significance (F = 3.6, df = 1.35, p =0.07). There was a significant increase in systolic BP from day 7 to day 14 (F = 13.2, df = 1.35, p = 0.001) and from day 14 to day 21 (F = 12.8, df = 1.35, p = 0.001), but not from day 21 to 28. For mean and diastolic BPs, there was a significant increase from day 7 to day 14 (F = 15.4, df = 1.35, p < 0.0001; F = 18.3, df = 1.35, p < 0.0001 respectively), but not from day 14 to day 28 (F = 1.1, df = 1.35, p = 0.3; F = 0.6, df = 1.35, p =0.4 respectively).
Repeated measures general linear models for neonates born at 32–36 weeks gestation over a 14-day period revealed no significant differences between the 32–33 week and 34–36 week groups in terms of systolic BP (F = 0.7, df = 1.32, p = 0.4), mean BP (F = 0.9, df = 1.31, p = 0.3) and diastolic BP (F = 0.03, df = 1.32, p = 0.9). In terms of trends over time, there were no significant differences between the 32–33 and 34–36 week groups. Based on repeated contrasts, from day 1 to day 7 there was a significant increase in systolic BP (F = 43.0, df = 1.32, p < 0.0001), mean BP (F = 30.7, df = 1.31, p < 0.0001) and diastolic BP (F = 18.7, df = 1.32, p < 0.0001). However, from day 7 to day 14 there were no significant difference in BP’s (F = 0.2, df =1.32, p = 0.6; F = 0.04, df = 1.31, p = 0.8; F = 0.09, df =1.32, p = 0.8 respectively).
Discussion
This paper provides normative mean BP data on non-ventilated premature infants born at more than 27 weeks gestation during the first month of life using an oscillometric method. The results indicate that the clinical practice of considering a mean BP of 1–2 mmHg above their gestation in the first days of life does fall within the 10th to 90th percentiles in the first few days of life. However, if an infant born at 28 weeks gestation who is 31 weeks corrected gestation becomes unwell, a mean BP of 32–34 mmHg may be hypotensive as the BP from 14 days onwards is similar to that of term infants in the first few days of life [9].
The number of neonates enrolled in this study is comparable to the numbers reported in many of the widely published studies on BP in the premature neonate. Tan [10] provided the BP of 45 stable infants born at less than 34 weeks gestation and weighing 1500 g during the first 2 weeks of life along with BPs for the first 10 weeks of life. This study together with the one reported here are two of the few published to date to provide systolic, mean and diastolic BPs in neonates for more than the first few days of life. Hegyi et al. provided a large dataset on BP in premature infants; however, the study period covered only in the first week of life and consisted of a heterogeneous group of infants, including those ventilated and on inotropes [1, 2]. Zubrow et al. provided information on 206 neonates born at less than 37 weeks gestation for the first 99 days of life. Again, Zubrow’s study included a heterogeneous sample, including infants ventilated and on inotropes, and the authors did not provide mean BPs [6]. The Northern Neonatal Nursing Initiative provided data on nearly 400 infants born less than 32 weeks gestation in the first 10 days of life, which again included ventilated infants and only provided systolic BP measured using a Doppler ultrasound method [7]. Our study of systolic, mean and diastolic BP in 147 infants represents one of the largest studies to date; in addition, our cohort of infants is homogeneous, being non-ventilated and not on inotropes. This study provides nomograms of 10th and 90th percentiles for systolic, mean and diastolic BPs for gestation at the time of birth as well as throughout the first month of life. We consider these to be clinically useful nomograms in comparison to other studies that have used regression analyses [4, 6].
There are a number of other studies providing BP data in premature infants, but these are limited to the first few days of life, include ventilated infants and use different methods of measurement, i.e. intra-arterial [3–5, 8, 11, 12]. Georgieff et al. provided data on 61 neonates from day 7 to 4 months of age using an oscillometric method. The results of our study are similar to those reported by Georgieff in that they reveal that premature infants have a rapid increase in their BP during the first 2 weeks of life [13]. In our study, the BPs after 14 days of life are similar to those of term infants in the first few days of life [9].
The oscillometric method was used in this study as it is commonly employed in clinical practice, and many neonates born at more than 28 weeks gestation do not require an arterial line. The Hewlett Packard Merlin Multiparameter Monitor, neonatal module has been validated by the manufacturer against intra-arterial measurements. Although there is some controversy regarding the accuracy of the oscillometric method, it has been shown to correlate more closely with intra-arterial measurements than the sphygmomanometer [14, 15]. As the oscillometric method is being used more commonly in clinical practice in this group of neonates, nomograms are required.
Conclusion
This study has obtained BP data on stable non-ventilated premature infants using an oscillometric method, thereby providing useful information for determining hypotension and hypertension in the premature neonate. Premature neonates stabilize their BP after 14 days of life and at this time have a BP similar to that of term infants [9]. This change has clinical implications for premature infants who become unwell after the 14th day of life and who may not be considered to be hypotensive if they are thought to have a BP similar to that of an infant in the first week of life at their current corrected gestational age.
References
Hegyi T, Carbone MT, Anwar M, Ostfeld B, Hiatt M, Koons A, Pinto-Martin J, Paneth N (1994) Blood pressure ranges in premature infants. I. The first hours of life. J Pediatr 124:627–633
Hegyi T, Anwar M, Carvone MT, Ostfeld B, Hiatt M, Koons A, Pinto-Martin J, Paneth N (1996) Blood pressure ranges in premature infants: II. The first week of life. Pediatrics 97:336–342
Shortland DB, Evans DH, Levene MI (1988) Blood pressure measurements in very low birth weight infants over the first week of life. J Perinat Med 16:93–97
Versmold HT, Kitterman JA, Phibbs RH, Gregory GA, Tooley WH (1981) Aortic blood pressure during the first 12 hours of life in infants with a birth weight 610 to 4220 grams. Pediatrics 67:607–613
Hulman S, Edwards R, Chen YQ, Polansky M, Falkner B (1991) Blood pressure patterns in the first three days of life. J Perinatol XI:231–234
Zubrow AB, Hulman S, Kushner H, Falkner B (1995) Determinants of blood pressure in infants admitted to neonatal intensive care units: A prospective multicenter study. J Perinatol 15:470–479
Northern Neonatal Nursing Initiative (1999) Systolic blood pressure in babies of less than 32 weeks gestation in the first year of life. Arch Dis Child Fetal Neonatal Ed 80:F38–F42
Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh N (1999) Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum Dev 56:151–165
Kent AL, Kecskes Z, Shadbolt B, Falk MC (2007) Normative blood pressure data in the early neonatal period. Pediatr Nephrol 22:1335–1341
Tan KL (1988) Blood pressure in very low birth weight infants in the first 70 days of life. J Pediatr 112:266–270
Spinazzola RM, Harper RG, de Soler M, Lesser M (1991) Blood pressure values in 500- to 750-gram birthweight infants in the first weeks of life. J Perinatol 11:147–151
Moscoso P, Goldberg RN, Jamieson J, Bancalari E (1983) Spontaneous elevation in arterial blood pressure during the first hours of life in the very-low-birth-weight infant. J Pediatr 103:114–117
Georgieff MK, Mills MM, Gomez-Martin O, Sinaiko AR (1996) Rate of change of blood pressure in premature and full term infants from birth to 4 months. Pediatr Nephrol 10:152–155
Park MK, Menard SW, Yuan C (2001) Comparison of auscultatory and oscillometric blood pressures. Arch Pediatr Adolesc Med 155:50–53
O’Brien E, Mee F, Atkins N, Thomas M (1996) Evaluation of three devices for self-measurement of blood pressure according to the revised British Hypertension Protocol: the Omron HEM-705CP, Phillips HP5332, and Nissei DS-175. Blood Press Monit 1:55–61
Acknowledgements
We would like to acknowledge the assistance of the Centre for Newborn Care nursing staff who assisted in performing BP measurements, and the parents of the neonates who enrolled into the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kent, A.L., Meskell, S., Falk, M.C. et al. Normative blood pressure data in non-ventilated premature neonates from 28–36 weeks gestation. Pediatr Nephrol 24, 141–146 (2009). https://doi.org/10.1007/s00467-008-0916-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0916-9