Abstract
Hypocalcaemic tetany is a known complication of plasmapheresis. It has two causes. Intravenously administered 4.5% human albumin solution (HAS) has no calcium or magnesium, so the replacement of plasma with this fluid depletes these ions. The citrate in fresh frozen plasma (FFP) chelates divalent cations, so the exchange with this at the end reduces the proportion of calcium and magnesium that is ionised. We studied the effect of supplementing HAS with 2 mmol/l calcium chloride and 0.8 mmol/l magnesium sulphate on the changes in ionised and total calcium and magnesium concentrations throughout plasmapheresis. The supplements prevented the falls in these concentrations that is otherwise seen during the HAS infusion, and, thus, the transient fall in ionised calcium concentration induced by the citrate in the FFP was not so profound, reaching 0.92 instead of 0.78 mmol/l (P = 0.002). Supplementation with calcium and magnesium during HAS maintains their balance and prevents tetany during the FFP infusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Plasmapheresis is used to treat some renal and autoimmune diseases in children and consists of the removal of the patient’s own plasma and its replacement with a substitute. The precise choice of replacement fluids varies between units, but, if plasmapheresis is repeated frequently or performed when there is a risk of bleeding (such as soon after a renal biopsy), it should include fresh frozen plasma (FFP) or similar products, at least at the end of the exchange.
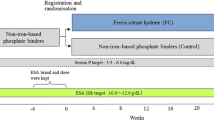
Life-threatening complications are rare during plasmapheresis, though up to a third of patients complain of chills, fever, allergic reactions, nausea or transient hypotension, and up to approximately 10% will develop hypocalcaemic tetany [1–4]. We observed several children developing tetany whilst receiving FFP and found that they had extremely low serum ionised calcium concentrations (Fig. 1a), which we assumed was due to the chelation of calcium by the citrate used for the anticoagulation of donor blood, and we treated them intravenously with calcium gluconate. Although this improved their symptoms, increasing their ionised calcium concentrations to nearly normal levels, it also caused a marked rise in the total calcium concentration (an example is shown in Fig. 1b). Because symptomatic hypocalcaemia on the one hand is unpleasant, and because causing hypercalcaemia by correcting it may be hazardous, we then investigated whether the supplementation of the 4.5% human albumin solution (HAS) with divalent cations would prevent the fall in ionised calcium during FFP infusion from reaching such a low trough and, thereby, prevent the troublesome symptoms of clinical tetany. We supplemented with both calcium and magnesium because we had observed falls in the concentrations of both cations.
Example of the changes in total (solid symbols) and ionised (open symbols) calcium concentrations in two children (round and square symbols) undergoing plasmapheresis with 80 ml/kg exchanges, the first 85% of the replacement being with HAS and the last 15% with FFP. a No calcium supplements were given; b calcium gluconate was run in parallel with the HAS and the FFP. By trial and error, we found that the ionised calcium concentration was best maintained by infusing 1.5 mmol of calcium with each litre of HAS, and 11 mmol with each litre of FFP
Patients and methods
Children undergoing plasmapheresis for glomerulonephritis had sessions in which the HAS replacement fluid was supplemented with calcium and magnesium, alternating with some when it was not. The plasmapheresis replacement volumes were 80 ml/kg, of which the first approximately 85% was with 45 g/l HAS, and the last 15% was with FFP. Exchanges were typically completed in about 2 h but were limited to a maximum rate of 2 l/h. Standard HAS contained no measurable calcium or magnesium. We supplemented HAS by adding 2 mmol/l calcium chloride and 0.8 mmol/l magnesium sulphate immediately before use, using careful sterile techniques. We measured the children’s serum albumin, ionised and total calcium, and total magnesium concentrations at the start and end of each HAS infusion and after 15 min of each FFP infusion, which had been the peak time for the development of clinical tetany. Ionised calcium concentration was measured by potentiometric sensing through a specific membrane, and the total divalent cations by bichromatic absorbance measurement, after complexing with arsenazo-III for calcium and with xylidyl blue for magnesium.
Each child was studied during at least one pair of plasmapheresis runs, with or without supplemented HAS. Statistical analysis was carried out on one set of values for each patient. For children that were studied on multiple occasions, we used the mean values for that child. Analysis was with paired t-tests, either comparing changes in concentration at different times within the same plasmapheresis session or comparing the concentrations at the same point between exchanges where HAS had or had not been supplemented. For ease of comparing data from several children, we expressed changes in chemical concentrations in percentage terms by defining each child’s initial concentrations as being 100%. The incidence of tetany symptoms was compared, using Fisher’s exact test.
Results
Eleven children (seven girls) underwent 91 sessions of plasmapheresis for rapidly progressing glomerulonephritis (two), focal segmental glomerulosclerosis (two), anti-glomerular basement membrane disease (two), transplant rejection (two), atypical haemolytic uraemic syndrome (one), Wegner’s granulomatosis (one), and recurrence of mesangiocapillary glomerulonephritis in a renal transplant (one). Thirty-one paired plasmapheresis runs were studied, with and without supplemented HAS. Six children were studied during just one pair of exchanges; one child was studied six times, three were studied five times, and one was studied four times.
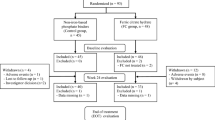
Infusion with HAS
During the first 85% of the plasmapheresis, when 45 g/l HAS was used as the exchange solution, the plasma albumin rose by 19.5% (CI 12.2–26.9, P < 0.000), from 34.9 g/l to 41.3 g/l, and this was the same whether standard or supplemented HAS was used. With standard HAS, the total and ionised calcium and the total magnesium concentrations fell, and did so by similar proportions (Fig. 2, blue lines). The ionised calcium fell from 1.22 mmol/l to 1.10 mmol/l (8.7%, CI 2.1–15.3, P = 0.015); the total calcium fell from 2.02 mmol/l to 1.70 mmol/l (15.1%, CI 9.9–20.3, P < 0.000), and the total magnesium fell from 0.71 mmol/l to 0.60 mmol/l (15.3%, CI 11.1–19.4, P < 0.000). By contrast, rather than falling, these concentrations all increased slightly during the supplemented HAS exchange (Fig. 2, red lines). The ionised calcium rose from 1.18 mmol/l to 1.36 mmol/l (15.7%, CI 7.8–23.6, P < 0.001); the total calcium rose from 2.01 mmol/l to 2.16 mmol/l (8.2%, CI 2.3–14.0, P < 0.01), and the magnesium rose from 0.71 mmol/l to 0.77 mmol/l (9.7%, CI 4.2–15.2, P < 0.003).
Total calcium (a), ionised calcium (b), and magnesium (c) concentrations during plasmapheresis using 80 ml/kg exchanges. Concentrations are shown before the start, after the first 85% of the plasma replacement using human albumin solution (HAS), and after 15 min of exchange with fresh frozen plasma (FFP). Blue symbols and lines indicate the use of standard HAS, and red indicates the use of calcium and magnesium supplemented HAS
Infusion with FFP
After 15 min of FFP exchange, the plasma albumin had fallen from 41.3 g/l to 38.5 g/l in both groups. In the group that had received standard HAS, the low total divalent cation concentrations had been partly corrected, the calcium increasing to 1.81 mmol/l (8.0% below the starting level, CI 2.4–13.7, P < 0.01, Fig. 2a), and the magnesium reaching 0.64 mmol/l (8.7% below the starting level, CI 3.9–13.6, P < 0.003, Fig. 2c). Similarly, the slight elevations in total calcium and magnesium concentrations that occurred during infusion with supplemented HAS fell towards their starting values, reaching 2.09 mmol/l and 0.75 mmol/l, respectively after 15 min of FFP infusion (Fig. 2a,c).
The concentrations of ionised calcium fell markedly and by similar proportions during FFP infusion, falling by 26% when preceded by standard HAS (CI 14.6–37.4, P < 0.000) and by 27.5% (CI 14.4–40.5, P < 0.001) after supplemented HAS (Fig. 2b). However, although the percentage falls were similar, the higher initial ionised calcium concentrations achieved by the use of supplemented HAS meant that the absolute values were higher, at 0.92 mmol/l compared to 0.78 mmol/l, after standard HAS (difference 0.14, CI 0.07–0.22, P = 0.002). Clinical symptoms of tetany were reported during 9/31 (29%) of the plasmapheresis sessions using standard HAS; none was reported during the 31 supplemented treatments (P < 0.002). Tetany was always associated with ionised calcium concentrations between 0.35 mmol/l and 0.67 mmol/l.
Discussion
Plasmapheresis is carried out fairly widely for various renal and immunological diseases to remove the presumed damaging plasma elements, such as anti-glomerular basement membrane antibody, or to replace deficient components, for example in atypical haemolytic uraemic syndrome. Previous authors that have used HAS as a replacement fluid have noted that the use of citrate as an anticoagulant may cause tetany, because it chelates divalent cations and reduces their free ionised concentrations, and have attempted to minimise this problem by infusing calcium prophylactically. Calcium gluconate has been given intravenously both in regular boluses [4, 5], and at a concentration of 2.2 mmol/l in the replacement fluid [5]. It is likely that in the process of correcting their patients’ ionised calcium levels, they will have raised their total calcium levels substantially, as we saw in out-patients treated that way (Fig. 1). We can speculate that individuals are likely to develop abnormally high ionised calcium concentrations once the citrate has been metabolised and the normal relationship between bound and free calcium restored.
Although we use heparin anticoagulation during plasmapheresis sessions, and, thereby, avoid the use of citrate throughout most of an exchange, we still encounter problems with hypocalcaemia, for two reasons. First, because HAS has no calcium or magnesium, exchange with this reduces the concentrations of ionised and total calcium, and of magnesium. In our children, who have relatively large volume exchanges (80 ml/kg, approximately equivalent to twice the plasma volume), the fall averages approximately 15%. Second, because we use FFP to reduce the depletion of various plasma components, including clotting factors, we necessarily infuse citrate during the last phase of the exchanges. This causes an approximately 25% fall in ionised calcium levels that may cause symptoms of tetany, which will last either until calcium is administered intravenously or until the citrate is metabolised. By adding calcium chloride and magnesium sulphate to HAS in concentrations similar to normal plasma levels, we avoid the early fall, and the balance of the divalent cation is maintained. Although the ionised calcium concentration (and presumably that of the free magnesium, which we did not measure) still fell during FFP infusion following the use of supplemented HAS, this did not cause any clinical symptoms of tetany. We have used supplemented HAS as a routine since completing this study and appear to have eliminated this symptom. We have also avoided the risk of inducing hypercalcaemia by infusing calcium during FFP exchange, which would correct the ionised calcium level transiently, but increased it substantially once the citrate was removed. We did not study the benefit that might have been seen with supplementing calcium alone, rather than supplementing both calcium and magnesium, but we speculate that it would be unlikely to have been so effective in maintaining the stability of the concentrations of both divalent cations.
In summary, we propose that, for small volume or single plasmapheresis sessions, the routine replacement fluid should be HAS, with additional calcium and magnesium supplements. This will maintain divalent cation balance. Furthermore, if FFP is required at the end to prevent the loss of plasma factors because of the volume or frequency of exchanges, this strategy will also make it unlikely that the patient will develop tetany due to citrate chelation.
References
Reimann PM, Mason PD (1990) Plasmapheresis: technique and complications. Intensive Care Med 16:3–10
Couriel D, Weinstein R (1994) Complications of therapeutic plasma exchange: a recent assessment. J Clin Apher 9:1–5
Mokrzycki MH, Kaplan AA (1994) Therapeutic plasma exchange: complications and management. Am J Kidney Dis 23:817–827
Basic-Jukic N, Kes P, Glavas-Boras S, Brunetta B, Bubic-Filipi L, Puretic Z (2005) Complications of therapeutic plasma exchange: experience with 4857 treatments. Ther Apher Dial 9:391–395
Weinstein R (1996) Prevention of citrate reactions during therapeutic plasma exchange by constant infusion of calcium gluconate with the return fluid. J Clin Apher 11:204–210
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnan, R.G., Coulthard, M.G. Minimising changes in plasma calcium and magnesium concentrations during plasmapheresis. Pediatr Nephrol 22, 1763–1766 (2007). https://doi.org/10.1007/s00467-007-0549-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-007-0549-4