Abstract
The omission of standards for renal length in infants younger than 1 year may result in a statistically significant increase in the frequency of “spurious” nephromegaly. Nonetheless, there are only a few reports specifically dealing with normal kidney dimensions in infants. Based on sonographic assessments performed on a sample of 992 healthy infants, between January 2002 and December 2004, this paper sets up standards for normal kidney dimensions in children aged 0–3 months, 3–6 months, 6–9 months, and 9–12 months and establishes correlations between kidney dimensions (length, width, and volume) and body length and weight. Linear as well as non-linear nomograms, with percentiles for all the kidney variables examined, based on body length, are provided. Also, statistically significant differences in mean values (P = 0.000) for all the observed neonatal kidney parameters, depending on gestational age at birth, are demonstrated. Principal advantages of our nomograms are that they are based on a large number of examined healthy infants and that kidney dimensions are related to body length. In addition, subjects are divided into four sub-annual age groups demonstrating gender-related differences in renal growth dynamics. Our linear nomograms are easier to use for routine clinical practice, but the percentile-based non-linear nomograms we present cover a much wider range of variations in normal infant kidney dimensions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sonography is method that enables easy, safe, and relatively accurate non-invasive assessment of kidney dimensions. Several published reports have examined normal kidney length, width, and volumes in children up to 19 years old. However, only a few of them specifically deal with normal kidney dimensions in infants up to 12 months of age [1–6]. Furthermore, the omission of standards for renal length in infants younger than 1 year may result in a statistically significant increase in the frequency of “spurious” nephromegaly. In their report Zerin and Meyer demonstrated that the prevalence of nephromegaly is reduced from 17.3% to 1.6% if multiple sub-annual standards for renal length in infants less than 12 months of age are included [7].
It is well known that the pattern of renal growth in the first year of life is non-linear. Renal growth is fastest during the first few weeks of life, with up to a 20% increase by the end of the first month. The rate of increase of renal length gradually slows through the remainder of the first year of life and finally stabilizes at approximately 2–3 mm/year [7]. To overcome the problem of non-linear infant renal growth, some published sonographic standards for renal length in relation to age have included multiple sub-annual standards with separate means and standard deviations (SDs) [1, 7]. Other researchers calculated linear or non-linear polynomial regression equations for renal size during the first year of life [3, 8].
This report aims to establish correlations between kidney dimensions (length, width, and volume) and body length and weight. Another purpose of this prospective study is to establish multiple sub-annual standards based on normal infant kidney dimension measurements performed on four different subgroups aged: 0–3 months, 3–6 months, 6–9 months and 9–12 months. Finally, this paper examines the influence of gestational age on neonatal kidney dimensions.
Materials and methods
Nine hundred ninety-two randomly selected healthy children of both genders, aged 0–12 months, were enrolled in this study between January 2002 and December 2004. Only healthy full-term neonates with gestational ages of 37–40 weeks and appropriate birth weight, and healthy infants with normal physical examination results and normal kidney sonograms, were included in the study. Excluded were full-term neonates who were either too small or too large for gestational age, as well as neonates with severe perinatal asphyxia, infection or congenital anomalies. Also excluded from the study were subjects with any renal malformations, such as unilateral renal agenesis, renal hypoplasia or dysplasia, ectopia, hydronephrosis, polycystic kidney disease, or cortical scarring. Finally, also excluded were patients with lower urinary-tract abnormalities or vesico-ureteral reflux. All the subjects examined were white infants coming from the region surrounding the city of Kragujevac, Serbia. All the measurements were performed by a single pediatric nephrologist, with 10 years of experience in pediatric abdominal sonography.
There were 472 girls and 520 boys. All those examined were divided into four age groups: 0–3 months, 4–6 months, 6–9 months and 9–12 months. Within the group of 0–3 month-olds there were 168 boys and 123 girls; in the group of 3–6 month-olds there were 119 boys and 105 girls; in the group of 6–9 month-olds there were 123 boys and 125 girls; finally, in the group of 9–12 month-olds there were 110 boys and 119 girls.
Sonography was performed with a LOGIC 400, GE color Doppler echo machine, with a multi-frequent 4–6 MHz probe. For each child examined, kidney length and width were calculated as the average of three consecutive measurements. The intra-observer variation expressed as a standard deviation was estimated to be 0.12 cm, which means that 95% of the investigator’s measurements of the length of a particular kidney were within ±0.24 cm. The coefficient of variation for the volume measurements was 6.67%, which means that 95% of the investigator’s measurements of the volume of a particular kidney were within ±13.33%.
Renal measurements were performed with the children in the supine position, scanning in the para-coronal view with the transducer positioned to obtain the longest kidney dimension. The sonographic probe was placed on the back of the child only when the presence of abdominal gases precluded adequate scanning from the standard position [9]. Kidney volume was calculated using the echo machine software. Stepper volume (STVOL) is the method used to calculate kidney volume using the LOGIC 400 urology software. According to this method the total volume of the organ is calculated as: V = d [(5/6) A1+A2+A3+...+(5/6)AN], where d is the spacing between the slices, A1,2,3.... are volumes of the slices and N is the number of slices. The distance between slices was 2.5 mm, and the number of slices (N) was automatically determined by built-in echo machine software, depending on kidney length. Body weight was measured on an analog scale (Libela, Celje) to the nearest 0.005 kg. Body length was measured with the child lying supine on the measuring board (Hyssna AB, Sweden), to the nearest 0.1 cm.
Statistical analyses
In this paper, data are presented either as mean ± standard deviation (SD) with 95% confidence intervals or as medians and percentiles. Two-way analysis of variance (ANOVA) was used to examine the relationship between age and gender, on one hand, and the observed kidney parameters, on the other hand. Kruskal–Wallis test was used for non-parametric data analysis, when more than two groups of children were compared. One-way ANOVA was performed when parametric data were compared among three or more groups. Relationships between two parameters were tested using Pearson correlation coefficient and linear regression equations. The analyses were performed in SPSS 10.0 for Windows. Results were considered significant if P < 0.05.
Results
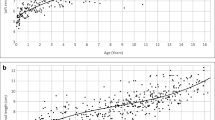
Statistically significant correlation was found between body length and all the examined kidney parameters. The strongest linear correlation coefficient was found between body length (height) and the kidney length (r = 0.728 for the right, r = 0.721 for the left and r = 0.724 for combined kidney length) and the combined kidney volume (r = 0.651), (Table 1). Because the established correlation coefficient (r) was statistically highly significant (P = 0.000), linear regression equations with 95% confidence interval (CI) limits for mean (CI) between body length and both kidney length and kidney volume were constructed, using a standard SPSS package (Fig. 1). The linear regression equation for the combined right and left kidney length is: kidney length (in centimeters) = 2.0425 + 0.0518 body length (in centimeters), and for the combined left and right kidney volume: kidney volume (in milliliters) = −11.081 + 0.4501 body length (in centimeters). The correlation coefficient between body length and combined kidney width was 0.565. Statistically significant correlations between body weight and the observed kidney parameters were also found, but they were not as strong as the ones found for the body height. The correlation coefficient between body weight and kidney length was r = 0.572. Correlation coefficient between body weight and kidney volume was r = 0.520. Finally, correlation coefficient between age and kidney length was r = 0.687.
Non-linear percentile-based growth charts between body length and kidney length and body length and kidney volume were also constructed (Fig. 2). Initially, percentile values for all the kidneys belonging to each of the body length group ranging from 48 cm to 88 cm were calculated (40 separate tables). The lines connecting all the points within the same percentile were then created and, finally, logarithmically transformed. Owing to small number of kidneys for body length below 48 cm and above 88 cm lines, the final lines were extrapolated.
No statistically significant difference in size between the right and the left kidneys was found. Data on kidney length and volume for all the infant age subgroups examined are presented in Table 2 and in Fig. 3. Statistically significant difference in mean values of kidney length and volume was found between boys and girls in the subgroups aged 0–3 months, 6–9 months and 9–12 months (Tables 3 and 4). In the 0–3 month-old subgroup, boys had significantly longer (P = 0.009) and larger in volume (P = 0.003) kidneys than girls had. Boys also had significantly longer (P = 0.000) and larger in volume (P = 0.000) kidneys than did girls in the 6–9 month-old subgroup of infants. In the 3–6 month-old subgroup, boys did not have kidneys either significantly longer (P = 0.929) or larger in volume (P = 0.064) than girls. If all the infants aged from 0–9 months are taken as a single group, boys had insignificantly longer (P = 0.178) but significantly larger in volume (P = 0.015) kidneys than girls had. In the subgroup aged 9–12 months, girls had significantly longer (P = 0.000) and significantly larger in volume (P = 0.006) kidneys than did boys (Fig. 4).
In neonates, one-way ANOVA was used to assess the relationship between gestational age at birth (37th, 38th, 39th, and 40th gestational week) and both kidneys’ lengths, widths, and volumes. Statistically significant difference in mean values for all the observed neonatal kidney parameters depending on gestational age at birth (P = 0.000) and body length (P < 0.005) was demonstrated. The influence of both gestational age and body length on observed kidney parameters was examined by two-way ANOVA. This analysis demonstrated that gestational age and body length are not independent from one another and had a combined statistically significant influence on kidney length (P = 0.000), width (P = 0.01), and volume (p = 0.001).
Discussion
Although renal length can be assessed sonographically with reasonable accuracy, the prevalence of false nephromegaly in infants is significantly increased if multiple sub-annual standards for normal kidney dimensions are not used during routine sonographic examination [7]. The major purpose of this prospective study was to establish accurate growth charts for sub-annual age groups and linear as well as percentile-based non-linear nomograms for normal infant kidney dimensions. We achieved this by performing kidney measurements on a large number of healthy infants. Because of a non-linear pattern of infant renal growth, our linear nomograms are probably less precise than non-linear ones [3, 10]. On the other hand, the advantage of having linear nomograms is that they are much easier to use in routine clinical practice. Moreover, our 5–95% confidence interval limits are narrower and, thus, more accurate than some published non-linear nomograms [3] and wide enough to overcome the problem of spurious nephromegaly [11].
A major limitation of our linear nomograms is that, due to a wide variation in normal values throughout the first year of life, a significant number of normal kidneys are above the 95% confidence interval limits. This is especially pronounced in the 9–12 month-old subgroup of infants and particularly applies for kidney volume. Our data demonstrate that gestational age affected only the first subgroup of infants but had no influence on the overall first-year kidney dimensions.
Comparison of linear nomograms demonstrates that the observer error is probably greater for kidney volume estimation than for length. This is not a surprise, because it is well known that volume estimation is technically more demanding than estimation of kidney length. On the other hand, it is worth mentioning that, when dealing with kidney volumes, in the first three age subgroups (0–3 months, 3–6 months and 6–9 months) with a total of 1,524 kidneys, we had only six points above the 99% CI. In the 9–12 month-old subgroup of infants there were 32/460 kidneys above the 99% CI, which is almost 8%. This difference is too big to be explained solely by a technical error. Even more, 14/21 of the largest kidneys (volume > 40 ml) were from girls, and this partly explains the gender-related differences in normal kidney growth dynamics that we found. To overcome this problem we constructed non-linear nomograms ranging from the third (P3) to the ninety-seventh (P97) percentile. Such nomograms are more precise than are linear ones, and they cover a much wider range of variations in normal kidney dimensions throughout the whole period of the first year of life.
The mean kidney length in our sample of healthy children is consistent with the data reported in the literature. For example, Rosenbaum et al. found that mean neonatal normal kidney length was 4.48 cm (SD = 0.31) [1]. Our respective values for the same subgroup of patients were 4.58 cm (SD = 0.55) for the right kidney and 4.53 cm (SD = 0.50) for the left kidney and 4.56 (SD = 0.52) for the combined kidney length. Data from the literature also demonstrate that there are no statistically significant differences in kidney length between different ethnic groups, such as Chinese and Western children [12].
In an attempt to create accurate and clinically useful growth charts, different authors have correlated the kidney parameters examined to age, body weight, height, and body surface area. Although age is often used for correlation [1, 7], in most of the published reports correlation to body length was found to be the best single predictor of renal length [3, 8, 13]. This is in agreement with our findings. Among body weight, length and age, the highest correlation was found between the observed kidney parameters and body length.
Similar values presented in different papers for kidney dimensions of either healthy neonates or healthy 12-month-old infants reflect the methodological accuracy of sonographic examination [1–4, 7, 8]. However, very few of those reports include sub-annual infant kidney dimensions, and, in most of them, the number of examined subjects is not large enough for appropriate statistical evaluation (Table 5) [1–3, 7, 8]. In their study, for example, Rosenbaum et al. included only 20 infants between 4 months and 8 months of age and only eight infants between 8 months and 12 months of age. Even more, a significant proportion of their examined infants suffered from nephro-urological or some other disease [1]. Zerin and Meyer pointed out that in such patients kidneys tend to be slightly shorter, in relation to age, than expected [7]. Similarly to our approach, Konus et al. related kidney length to both body length and age. Their findings of the mean right and left kidney length for each subgroup of infants examined are similar to ours, but the 5–95% confidence interval limits for the means, very narrow in our report, were not presented in their paper [3]. We believe that the narrow 5–95% confidence interval limits for means, presented in our report, are the consequence of the much larger number of subjects we examined [11].
Conflicting data exist regarding the difference in size of the right and the left kidney. Although, in some reports, both kidneys have been found to be of equal size [8, 14, 15], in most of the published papers the left kidney was longer and slimmer than the right one [3, 10, 16]. Schmidt et al. state that the left kidney is longer than the right one at all ages and in both genders. However, in their research, neonatal right and left kidney length in girls was identical and, in boys, the mean difference was only 1 mm [10]. Scott et al., who also found the left kidney to be longer than the right one, correctly pointed out that confidence intervals showed the magnitude of the differences between kidneys to be small and not of clinical importance [16]. In our study we found that the left kidney was slightly, but not significantly, longer than the right one in all the subgroups of infants examined. Also, there was no statistically significant difference in right and left kidney volumes. It is worth mentioning that the other major study on normal infant kidney dimensions also failed to demonstrate a statistically significant difference in size between right and left kidneys [14]. Because we found no statistically significant difference either in kidney length or in kidney volume between right and left kidneys, we decided to combine the values of both kidneys and to create a single growth chart for each of the observed parameter (Figs. 1 and 2). With such an approach, based on the measurements of 1,984 normal infant kidneys, we were able to create more accurate nomograms for both kidney length and volume. Also, a better estimate of gender differences was achieved.
In a well-designed study Fritz et al. demonstrated that three-dimensional (3D) sonography is comparable to CT or MRI in assessing renal volume in children (mean difference of −2.6 ± 4.4%). In the same study the value of two-dimensional (2D) sonography in assessing renal volume in children was also examined. It was concluded that, although less accurate than those determined by 3D sonography, renal volumes determined by 2D sonography are acceptably comparable to the ones obtained by CT or MRI (mean difference −3.8 ± 14.7%) [17]. We did not perform 3D sonography, or CT, or MRI on our group of examined infants and were not in a position to compare renal volumes obtained by 2D sonography. Our data demonstrate that further 3D studies on kidney volume, especially in 6–12 month old infants, are necessary.
Most of the published reports found no gender difference in renal size in infants and children beyond the neonatal period [3, 8, 14]. Schmidt et al., who found a small but statistically significant gender difference in kidney size, commented that, to be able to reach gender-related significant difference in kidney volume/length, one would have to have at least 85/150 subjects of each gender in each of the subgroups of infants examined [10]. In one of the only two published reports that fulfill this criterion, significant gender-related difference in kidney size was indeed found [16]. However, the other report failed to confirm this finding [14]. In our study, when right and left kidneys were evaluated separately, we did find that boys had slightly, but not significantly, larger kidney volume in both the right and the left kidney in the first 9 months of life. On the other hand, girls had kidneys both longer and larger in volume than had boys in the subgroup of infants aged 9–12 months. When all the four subgroups were taken together, no gender-related difference in kidney size was found. When we combined right and left kidneys, renal volume in 0–9 month-old boys compared to girls became significantly larger (P = 0.015), confirming the observation that one would need to have a large sample of subjects to be able to reach statistically significant gender-related difference in kidney size [10]. Our results confirm the findings from previous reports [10] that, in infants up to 9 months of age, boys have kidneys that are larger in volume than those of girls, but they also seem to confirm the observation that this difference is more of statistical than of clinical importance [11, 16, 18].
A very interesting finding was that in the 9–12 month-old subgroup of infants both the right and the left kidney in girls were longer and larger in volume than in boys. This finding, initially, was of borderline statistical significance, but when we combined right and left kidneys it became highly statistically significant (P = 0.000 for kidney length and P = 0.000 for kidney volume). To the best of our knowledge, this observation has not been reported thus far. One of the possible explanations might be that, in all the published reports, this subgroup of infants was either the smallest one examined or was not included at all [1–3, 8, 10, 12].
A limitation of this study is the lack of inter-observer variability; given that one person did all the measurements. Another limitation is ethnic homogeneity of the sample, although data presented by Loftus et al. demonstrated that this is not of much relevance [12]. Finally, because of non-linear infant renal growth, our linear regression equations do suffer from some lack of precision, although standard errors and 5–95% confidence interval limits for the means presented in this report are narrower than most of the intervals reported in the literature [3, 11]. Non-linear percentile-based growth charts that we present in the paper largely overcome this limitation.
Conclusion
Sonographic assessment of kidney dimensions and growth during the first year of life enables early recognition of either pathological growth or hypoplasia of these organs. Statistically significant correlation between physiological body growth during the first year of life and kidney dimensions was established. Positive correlation was found between both kidney length and volume and body length and weight. During the first year of an infant’s life the strongest correlation was established between kidney length and body length (height). A relationship between kidney dimensions and gestational age in full-term neonates was also found. There was no statistically significant difference in size between the right and the left kidney in any of the groups of infants examined. In infants up to 9 months of age boys had kidneys that were insignificantly longer, but significantly larger in volume, than those of girls. Within the 9–12 month subgroup girls had significantly longer and larger kidneys than boys had. Interestingly, this finding was not observed in any of the previously published reports and sheds a new light on gender differences in renal growth dynamics in healthy infants. Equal size of kidneys in 18-month-old male and female children demonstrated by Schmidt et al. [10] suggests that non-linear renal growth expands from infancy to, at least, the first half of the second year of life. Finally, in this report, we established body length-based both linear and non-linear nomograms for kidney length and volume in children up to 12 months of age. These nomograms allow accurate prediction of sonographically assessed kidney dimensions in any full-term neonate and infant up to 12 months of age.
References
Rosenbaum DM, Korngold E, Teele RL (1984) Sonographic assessment of renal length in normal children. AJR Am J Roentgenol 142:467–469
Blane CE, Bookstein FL, DiPietro MA, Kelsch RC (1985) Sonographic standards for normal infant kidney length. AJR Am J Roentgenol 145:1289–1291
Konus OL, Ozdemir A, Akkaya A, Erbas G, Celik H, Isik S (1998) Normal liver, spleen, and kidney dimensions in neonates, infants, and children: evaluation with sonography. AJR Am J Roentgenol 171:1693–1698
Weisenbach J, Horvath M, Jeges S, Adamovich K, Huszar T (2001) Normal percentiles of kidney size in children as measured by ultrasonography. Orv Hetil 142:71–74
Sargent MA, Long G, Karmali M, Cheng SM (1997) Interobserver variation in sonographic estimation of renal volume in children. Pediatr Radiol 27:663–666
Dixit PK, Sahai SB, Rath B, Garg A, Chowdhury V (1994) Norms for renal parenchymal volume in Indian children. Indian Pediatr 31:1059–1064
Zerin JM, Meyer RD (2000) Sonographic assessment of renal length in the first year of life: the problem of “spurious nephromegaly”. Pediatr Radiol 30:52–57
Han BK, Babcock DS (1985) Sonographic measurements and appearance of normal kidneys in children. AJR Am J Roentgenol 145:611–616
De-Sanctis JT, Connolly SA, Bramson RT (1998) Effect of patient position on sonographically measured renal length in neonates, infants and children. AJR Am J Roentgenol 170:1381–1383
Schmidt I, Main K, Damqaard I, Mau C, Haavisto AM, Chellakooty M, Kirsten AB, Petersen JH, Scheike T, Olgaard K (2004) Kidney growth in 717 healthy children aged 0–18 months: a longitudinal cohort study. Pediatr Nephrol 19:992–1003
Cockburn DM (2006) How to make clinical decisions from statistics. Clin Exp Optom 89:176–183
Loftus WK, Gent RJ, LeQuesne GW, Metreweli C (1998) Renal length in Chinese children: sonographic measurement and comparison with western data. J Clin Ultrasound 26:349–352
Dinkel E, Ertel M, Dittrich M, Peters H, Berres M, Schulte-Wissermann H (1985) Kidney size in childhood. Sonographical growth charts for kidney length and volume. Pediatr Radiol 15:38–43
Jelen Z (1993) The value of ultrasonography as a screening procedure of the neonatal urinary tract: a survey of 1021 infants. Int Urol Nephrol 25:3–10
Holloway H, Jones TB, Robinson AE, Harpen MD, Wiseman HJ (1983) Sonographic determination of renal volumes in normal neonates. Pediatr Radiol 13:212–214
Scott JES, Hunter EW, Lee REJ, Matthews JNS (1990) Ultrasound measurement of renal size in newborn infants. Arch Dis Child 65:361–364
Fritz GA, Riccabona M, Bohdal G, Quehenberger F (2003) Accuracy of renal volume assessment in children by three-dimensional sonography. Rofo 175:540–546
Chan KBY, Man-Son-Hing M, Molnar FJ, Laupacis A (2001) How well is the clinical importance of study results reported? An assessment of randomized controlled trials. CMAJ 165:1197–1202
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vujic, A., Kosutic, J., Bogdanovic, R. et al. Sonographic assessment of normal kidney dimensions in the first year of life—a study of 992 healthy infants. Pediatr Nephrol 22, 1143–1150 (2007). https://doi.org/10.1007/s00467-007-0478-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-007-0478-2