Abstract
Recent studies indicate that adding the mineralocorticoid receptor antagonist spironolactone (SP) to angiotensin converting enzyme inhibitors (ACEI) or ACEI and angiotensin receptor blocker (ARB), which is known as a triple blockade, enhances the more beneficial effects on urinary protein excretion of patients with chronic kidney diseases. In this study, we explored the effects of SP on urinary protein excretion in patients with Alport syndrome featuring persistent proteinuria in spite of the long-term use of ACEI (lisinopril) or both ACEI and ARB (candesartan). Five patients with Alport syndrome were enrolled and SP treatment (25 mg/day) was started. At the start of SP administration, all patients showed good renal function and none of them suffered from hypertension. We decided to assess the effect of SP by determining the morning urinary protein/creatinine ratio (U-P/C) and estimated glomerular filtration rate (EGFR). After SP treatment was started, U-P/C was significantly reduced at 3, 6, 12 and 18 months, while EGFR did not change. The drop in systolic and diastolic blood pressure was statistically significant and serum potassium level was slightly elevated. None of the patients showed signs of severe hyperkalemia (>5.0 mEq/l). These results suggest that aldosterone receptor blockade combined with ACEI and ARB therapy offers a valuable adjuvant treatment for the reduction of proteinuria in patients with Alport syndrome as in those with other chronic kidney diseases. SP can thus be expected to constitute a good renoprotective agent for Alport syndrome. These preliminary data indicate that large-scale trials of this therapy should be done.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alport syndrome, a progressive and hereditary form of glomerular nephritis, is a primary basement membrane disorder arising from mutations in genes encoding several members of the type IV collagen protein family [1]. It is a genetically heterogeneous disease with X-linked, autosomal recessive, and autosomal dominant variants. No specific curative therapy exists yet for this disorder, and most treatments are aimed at slowing the progression of the disease. Recently, using cyclosporine has been reported to show beneficial effects for human Alport patients and in animal models [2–4]. In addition, other studies have indicated that angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) show antiproteinuric effects for patients with Alport syndrome and in animal models [5–10]. However, these agents are only temporally effective for reducing urinary protein excretion.
Aldosterone is the principal physiological mineralocorticoid and acts to promote unidirectional sodium and water transport. Evidence has been recently increasing that aldosterone-induced vasculopathy may underlie progressive renal diseases [11, 12]. In fact, some studies show that adding spironolactone (SP), a mineralocorticoid receptor antagonist, to ACEIs enhances the beneficial effects on urinary protein excretion in patients with chronic nephritis including diabetic nephropathy [13–16].
In this study, we explored the effect of SP on urinary protein excretion and the glomerular filtration rate (GFR) in patients with Alport syndrome featuring persistent proteinuria despite the use of ACEI or a combination of ACEI and ARB.
Patients and methods
Patients
Table 1 summarizes the patients’ characteristics at the start of SP therapy. Five patients with Alport syndrome were enrolled, three of whom had the X-linked inherited form and two the autosomal dominant form. All patients satisfied the following modified Kashtan criteria [17]: (1) continuous microhematuria and proteinuria; (2) family history of one or several family members affected by well-documented Alport syndrome; (3) electron microscopic findings of renal biopsy showing pathognomonic lesions of the glomerular basement membrane (GBM), i.e., thickening of the GBM accompanied by splitting and splintering of the lamina densa [1, 18–20]. Although Patient 5 was diagnosed as having thin basement membrane disease, the electron microscopic GBM findings showed regional thickening and splintering abnormalities and both the patient and her father had persistent proteinuria. We therefore assumed that she had Alport syndrome in the early stage. When the SP treatment started, the patients were between 11 and 19 years of age (median 18.0 years) and all had persistent proteinuria, with a morning urinary protein/creatinine ratio (U-P/C) of more than 0.2 g/g (median 0.61 g/g) in spite of treatment with ACEI (lisinopril) or ACEI and ARB (candesartan) combined for more than 19 months. Four patients were treated with both ACEI and ARB and the other with ACEI only because of acute renal failure 2 months after the start of ARB treatment, when the serum creatinine level had increased from 0.96 to 4.24 mg/dl. All patients were normotensive and estimated glomerular filtration rates (EGFRs) were above 90 ml/min. One patient was treated with pravastatin for hyperlipidemina, and another patient with allopurinol for hyperuricemia. Final average doses of lisinopril and candesartan were 0.20±0.05 mg/kg/day (11.0±2.45 mg/day) and 0.11±0.03 mg/kg/day (5.5±0.96 mg/day), respectively.
Methods
The patients visited the outpatient clinic in Kobe University Hospital at least once every 3 months. At each visit, blood pressure was measured with an automatic sphygmomanometer and morning urine was examined. We decided to assess the effectiveness of SP in terms of U-P/C and EGFR [21–25]. Blood samples were taken for serum creatinine, albumin and potassium measurements with standard laboratory techniques. During treatment, no patients were instructed on special dietary therapy, such as potassium restriction. EGFR was calculated with Schwartz’s formula: EGFR=k×height (cm) /serum creatinine (mg/dl) (k: 0.55 for boys of 2–12 years and also girls of 2–21 years, and 0.70 for males of 13–21 years) [24, 25].
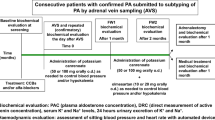
Study design
Patients with proven Alport syndrome and with persistent proteinuria in spite of ACEI or combined ACEI and ARB treatment were invited to participate in this clinical study after information had been given about the natural history of the disease, and the possibility of reducing urinary protein excretion as well as slowing down disease progression with SP treatment. Parents of the patients gave their informed consent. The dosage of SP was fixed at 25 mg/day, which was based on the previous studies [14, 15]. U-P/C just before the start of SP administration was compared with U-P/C at 3, 6, 12, and 18 months after the start of the treatment and baseline EGFR was compared with that at 18 months. Blood pressure and serum potassium levels before the treatment were compared with those three months after the start of treatment.
Statistical analysis
Data are expressed as mean±SE. Statview-J5.0 software was used for statistical calculations. Changes in parameters before and after treatment were compared by using two-group paired t-tests, and P values of <0.05 were considered significant.
Results
Proteinuria
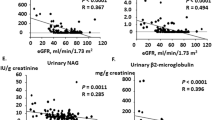
Figure 1 shows the time-course changes in U-P/C. Before the start of SP administration, U-P/C was 0.61±0.10 g/g and showed no significant reduction, that is, the maximal antiproteinuric effects obtained with ACEI or both ACEI and ARB were no longer observed. After the start of the treatment with SP, U-P/C was significantly reduced at every time point (P<0.05) and gradually dropped to a minimum (0.13±0.06 g/g) at 18 months.
Proteinuria in patients treated with SP for 18 months. Proteinuria expressed as morning urinary protein/creatinine ratio (U-P/C). Before the start of spironolactone (SP) therapy, U-P/C showed no significant reduction, but was significantly reduced 3, 6, 12 and 18 months after the start of treatment with SP. *P<0.05
Estimated GFR
EGFR remained virtually unchanged throughout SP therapy (before SP treatment: 129.2±21.4 ml/min; 18 months later: 110.1±30.1 ml/min; P=0.115) (Fig. 2).
Blood pressure
Before SP was initiated, the systolic and diastolic blood pressure values were 110.8±5.0 mmHg and 58.2±2.7 mmHg. Three months after SP administration, they had dropped to 91.2±6.6 mmHg and 51.0±3.0 mmHg, respectively (Table 2). In spite of this significant reduction (P<0.05), none of the patients complained of dizziness or orthostatic hypotension.
Serum potassium
Although serum potassium level 3 months after SP treatment was significantly higher than that before the start of treatment (P<0.05), none of the patients developed serious hyperkalemia (>5.0 mEq/l) as result of the SP therapy (Table 2).
Adverse events
There were no adverse events, including liver dysfunction, allergic manifestations, hyponatremia, arrhythmia, muscle weakness, or gynecomastia. No patients dropped out of this study.
Discussion
In this study, we demonstrated that treating Alport patients with SP in addition to ACEI or ACEI and ARB is helpful for reducing urinary protein excretion.
Alport syndrome is bound to progress to end-stage renal disease and there is no treatment except dialysis and transplantation [1, 17–19]. Callis et al. [3, 4] reported that cyclosporine may halt progression in human Alport syndrome with severe proteinuria, and this was followed by a demonstration that cyclosporine had beneficial effects in terms of improving renal function and delaying the onset of renal failure in canine X-linked Alport syndrome [2]. This study concluded that cyclosporine may be able to alter glomerular hemodynamics, resulting in a delayed deterioration of glomerular basement membrane. On the other hand, another study found that cyclosporine therapy for Alport syndrome not only suppressed urinary protein excretion but also accelerated renal fibrosis and resulted in reduced GFR [26]. It is thus very difficult to determine how long cyclosporine therapy should be continued and how many doses of cyclosporine are appropriate for Alport syndrome. Grodecki et al. [5] used ACEI to treat Samoyed dogs with X-linked hereditary nephritis and found the treatment beneficial with respect to renal function, renal structure, and survival. The affected treated dogs showed a significant transient reduction in glomerular basement membrane splitting. As for the effectiveness of ARB for Alport syndrome, Inoue et al. [10] demonstrated in a mouse model that ARB contains more renoprotective properties than calcium antagonists, thus inhibiting the progression of glomerulopathy and interstitial fibrosis. Some studies have described the effect of ACEI on patients with Alport syndrome [8, 9] and now it is believed that it is more effective to treat them with a combination of ACEI and ARB than with either agent alone. We also used treatment with ACEI and ARB, but found it to be temporarily effective and not effective enough to keep urinary protein excretion levels reduced in the long term.
Chrysostomou et al. [13] reported that SP was effective in long-term ACEI therapy for chronic kidney disease with persistent proteinuria. This was followed by some reports which confirmed the effectiveness of aldosterone receptor blockade for reducing urinary protein excretion [14–16]. A recent, double-blind, placebo-controlled study indicated that SP combined with ACEI had an antiproteinuric effect on chronic kidney diseases including diabetes nephropathy and IgA nephropathy [27].
Aldosterone is a major regulator of extracellular fluid volume and the major determinant of potassium metabolism. In recent years, evidence has been accumulating that aldosterone can affect vascular remodeling and collagen formation, and exerts a non-genomic action to modify endothelial function. It can also produce deleterious effects in both the cardiovascular system and the kidneys [11, 12]. Indeed, there has been considerable experimental and clinical evidence that aldosterone can contribute to the development of nephrosclerosis and renal fibrosis in models of diabetes and hypertension [28, 29]. In addition, a number of studies using human and animal models have indicated that aldosterone blockade protects against progression of end-organ damage through both hemodynamic and direct cellular actions. Nishiyama et al. [30] demonstrated in rats that aldosterone caused mesangial cell proliferation and urine protein excretion while activating the mitogen-activated protein kinase (MAPK) pathway, and this deterioration improved with the administration of eplerenone, a selective aldosterone receptor antagonist. Aldosterone has been shown to stimulate type IV collagen production, the principal component of glomerular basement membrane and mesangial matrix in cultured rat mesangial cells, and treatment with a combination of ACEI and SP to reduce urinary type IV collagen excretion in patients with diabetic nephropathy [31]. SP may thus be able to attenuate inflammatory changes in renal parenchyma of Alport patients with continuous urine protein excretion.
Hyperkalemia is potentially one of the most serious complications resulting from combining SP with ACEI and ARB. Since the randomized aldosterone evaluation study (RALES) was published, hyperkalemia-associated morbidity and mortality as well as the rate of prescriptions for SP have increased [32]. The patients in our study were carefully screened for risk of developing hyperkalemia as a result of the combined treatment. While the serum potassium level after treatment with SP was significantly higher than before, it was in no way a serious clinical problem. Normal estimated GFRs of all patients may prevent serum potassium levels from being much more higher, and this means that SP treatment in our study could exert a renoprotective effect without severe adverse events. Moreover, the suppression of aldosterone activity with ACEI, ARB and SP was quite successful, and resulted in only mild hyperkalemia.
We have demonstrated that the addition of SP to ACEI only or to ACEI and ARB resulted in a reduction of U-P/C after 3 months in patients with Alport syndrome, and that this reduction was maintained for as long as 18 months. The systolic and diastolic blood pressure dropped significantly after treatment with SP. Although maintenance of adequate blood pressure will often cause a reduction in urinary protein excretion, all the patients in our study maintained normotension and good renal function even before SP treatment, so it can be concluded that a reduction in the blood pressure is not a direct factor in the reduction of urinary protein excretion.
Our study has certain limitations. The first is that this is an uncontrolled and small-scale study with only five patients enrolled. Moreover, it is quite unusual two out of five patients to be genetically autosomal dominant variants, for most forms of the disease are generally of the X-linked variety and the autosomal dominant form accounts for only a small percentage [1, 18]. In addition, electron microscopic examination resulted in one of the patients being diagnosed as thin basement membrane disease with partial abnormalities of the glomerular basement membrane. However, it is very difficult to discriminate between the initial stage of Alport syndrome and thin basement membrane disease, and since both the patient and her father have continuous proteinuria as well as microhematuria, we have now evaluated her renal biopsy findings as the initial stage of Alport syndrome. This indicates that the Alport-related gene should be analyzed in these patients [1, 19]. The second shortcoming is that this is a rather short-term study. Although it is generally accepted that lowering protein excretion is a desirable treatment goal for chronic proteinuric kidney disease, it could not be determined in this study whether treatment with SP can suppress urinary protein excretion for a long time. In this connection, we previously found that urinary protein excretion increased again during long-term ACEI therapy.
In summary, we were able to demonstrate that adding SP to ACEI and ARB may be effective for lowering proteinuria in Alport syndrome. However, a larger-scale study with longer follow-up is required to demonstrate whether the results shown in our study translate to improved renal survival for patients with Alport syndrome.
References
Kashtan CE (2000) Alport syndromes: phenotypic heterogeneity of progressive hereditary nephritis. Pediatr Nephrol 14:502–512
Chen D, Jefferson B, Harvey SJ, Zheng K, Gartley CJ, Jacobs RM, Thorner PS (2003) Cyclosporine A slows the progressive renal disease of Alport syndrome (X-linked hereditary nephritis): results from a canine model. J Am Soc Nephrol 14:690–698
Callis L, Vila A, Nieto J, Fortuny G (1992) Effect of cyclosporine A on proteinuria in patients with Alport’s syndrome. Pediatr Nephrol 6:140–144
Callis L, Vila A, Carrera M, Nieto J (1999) Long-term effects of cyclosporine A in Alport’s syndrome. Kidney Int 55:1051–1056
Grodecki KM, Gains MJ, Baumal R, Osmond DH, Cotter B, Valli VE, Jacobs RM (1997) Treatment of X-linked hereditary nephritis in Samoyed dogs with angiotensin converting enzyme (ACE) inhibitor. J Comp Pathol 117:209–225
Cohen EP, Lemann J Jr (1996) In hereditary nephritis angiotensin-converting enzyme inhibition decreases proteinuria and may slow the rate of progression. Am J Kidney Dis 27:199–203
Gross O, Beirowski B, Koepke ML, Kuck J, Reiner M, Addicks K, Smyth N, Schulze-Lohoff E, Weber M (2003) Preemptive ramipril therapy delays renal failure and reduces renal fibrosis in COL4A3-knockout mice with Alport syndrome. Kidney Int 63:438–446
Proesmans W, Dyck MV (2004) Enarapril in children with Alport syndrome. Pediatr Nephrol 19:271–275
Proesmans W, Knockaert H, Trouet D (2000) Enarapril in paediatric patients with Alport syndrome: 2 years’ experience. Eur J Pediatr 159:430–433
Inoue M, Nomura S, Naito I, Ishikawa E, Katayama K, Oosugi K, Nakano T (2005) Renoprotection of angiotensin II receptor blocking agent for Alport’s mice. Abstract from American Society of Nephrology Renal Week 2005, 8–13 November 2005, Philadelphia
Epstein M (2001) Aldosterone as a mediator of progressive renal disease: pathogenetic and clinical implications. Am J Kidney Dis 37:677–688
Epstein M (2003) Aldosterone receptor blockade and the role of eplerenone: evolving perspectives (2003) Nephrol Dial Transplant 18:1984–1992
Chrysostomou A, Becker G (2001) Spironolactone in addition to ACE inhibition to reduce proteinuria in patients with chronic renal disease. N Engl J Med 345:925–926
Sato A, Hayashi K, Naruse M, Saruta T (2003) Effectiveness of aldosterone blockade in patients with diabetic nephropathy. Hypertension 41:64–68
Sato A, Hayashi K, Saruta T (2005) Antiproteinuric effects of mineralocorticoid receptor blockade in patients with chronic renal disease. Am J Hypertens 18:44–49
Williams GH, Burgess E, Kolloch RE, Ruilope LM, Niegowska J, Kipnes MS, Roniker B, Patrick JL, Krause SL (2004) Efficacy of eplerenone versus enalapril as monotherapy in systemic hypertension. Am J Cardiol 93:990–996
Kashtan CE, Michael AF (1996) Alport syndrome. Kidney Int 50:1445–1463
Gregory MC, Terreros DA, Barker DF, Fain PN, Denison JC, Atkin CL (1996) Alport syndrome - clinical phenotypes, incidence, and pathology. Contrib Nephrol 117:1–28
Pescucci C, Mari F, Longo I, Vogiatzi P, Caselli R, Scala E, Abaterusso C, Gusmano MS, Miglietti N, Bresin E, Renieri A (2004) Autosomal-dominant Alport syndrome: natural history of a disease due to COL4A3 or COL4A4 gene. Kidney Int 65:1598–1603
Yoshikawa N, Cameron AH, White RH (1981) The glomerular basal lamina in hereditary nephritis. J Pathol 135:199–209
Ginsberg JM, Chang BS, Matarese RA, Garella S (1983) Use of single voided urine samples to estimate quantitative proteinuria. N Engl J Med 309:1543–1546
Abitbol C, Zilleruelo G, Freundlich M, Strauss J (1990) Quantitation of proteinuria with urinary protein/creatinine ratios and random testing with dipsticks in nephrotic children. J Pediatr 116:243–247
Eknoyan G, Hostetter T, Bakris GL, Hebert L, Levey AS, Parving HH, Steffes MW, Toto R (2003) Proteinuria and other markers of chronic kidney disease: a position statement of the national kidney foundation (NKF) and the national institute if diabetes and digestive and kidney diseases (NIDDK). Am J Kidney Dis 42:617–622
Schwartz GJ, Haycock MB, Edelmann CM Jr., Spizer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Schwartz GJ, Gauthier B (1985) A simple estimate of glomerular filtration rate in adolescent boys. J Pediatr 106:522–526
Charbit M, Dechaux M, Gagnadoux MF (2003) Cyclosporine A therapy in Alport syndrome. J Am Soc Nephrol 14:111A
Chrysostomou A, Pedagogos E, MacGregor L, Becker GJ (2006) Double-blind, placebo-controlled study on the effect of the aldosterone receptor antagonist spironolactone in patients who have persistent proteinuria and are on long-term angiotensin-converting enzyme inhibitor therapy, with or without an angiotensin II receptor blocker. Clin J Am Soc Nephrol 1:256–262
Sun Y, Zhang J, Zhang JQ, Ramires FJ (2000) Local angiotensin II and transforming growth factor beta 1 renal fibrosis of rats. Hypertension 35:1078–1084
Blasi ER, Rocha R, Rudolph AE, Blomme EAG, Polly ML, McMahon EG (2003) Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int 63:1791–1800
Nishiyama A, Yao L, Nagai Y, Miyata K, Yoshizumi M, Kagami S, Kondo S, Kiomoto H, Shokoji T, Kimura S, Kohno M, Abe Y (2004) Possible contributions of reactive oxygen species and mitogen-activated protein kinase to renal injury in aldosterone/salt induced hypertensive rats. Hypertension 43:841–884
Wakisaka M, Spiro MJ, Spiro RG (1994) Synthesis of type IV collagen by cultured glomerular cells and comparison of its regulation by glucose and other factors with that of type IV collagen. Diabetes 43:95–103
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA (2004) Rates of hyperkalemia after publication of the randomized Aldosterone Evaluation Study. N Engl J Med 351:543–551
Acknowledgement
This work was supported by grants from Fund of Kidney Disease Research from Hyogo Prefecture Health Promotion Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaito, H., Nozu, K., Iijima, K. et al. The effect of aldosterone blockade in patients with Alport syndrome. Pediatr Nephrol 21, 1824–1829 (2006). https://doi.org/10.1007/s00467-006-0270-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0270-8