Abstract
Although immunosuppressive regimens of corticosteroids combined with high-dose intravenous cyclophosphamide (IVCY) have been reported to suppress the activity of lupus nephritis, there is controversy regarding its application for children and adolescents, because of its potential toxicity including gonadal dysfunction. On the basis of the recent finding that a low-dose IVCY regimen for induction therapy in adult lupus nephritis effectively achieves renal remission comparable with that achieved with a conventional high-dose IVCY regimen, we treated two children with severe lupus nephritis by low-dose (fixed dose of 500 mg m−2, cumulative dose 3 g m−2, approximately one-fourth of the conventional high-dose IVCY regimen) IVCY and oral mizoribine (5 mg kg−1 day−1) and steroids (3 methylprednisolone pulse followed by oral prednisolone). They responded well to this regimen, showing remarkable improvement in both histological and clinical manifestations in a short period of time. From these findings we suggest that the new low-dose IVCY regimen may be as effective as the conventional high-dose IVCY regimen, without significant adverse effect, for induction therapy in children with severe lupus nephritis (class III or IV).
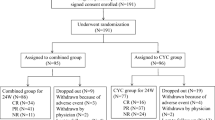
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical symptoms of systemic lupus erythematosus (SLE) are often more severe in children than in adults. Renal involvement develops in 30–70% of children with SLE [1] and the risk of progression to end-stage renal disease in childhood LN is 18 to 50% [2]. The optimum treatment is, however, unclear, because of the low prevalence of the condition.
Although an extended course of high-dose intravenous cyclophosphamide (IVCY) in combination with glucocorticoids has substantially improved renal survival, its substantial toxic effects, for example myelotoxicity, severe infection, and gonadal toxicity, have been a matter of concern.
Mizoribine (MZB), which was developed in Japan about 20 years ago, has been applied without serious adverse effects in the treatment of renal transplantation [3], nephrotic syndrome [4], IgA nephropathy [5, 6], and lupus nephritis [7, 8]. Its clinical efficacy has, however, been reported to be limited in patients with mild cases of lupus nephritis (non-class IV) [8] and thus monotherapy might be inadequate for more severe cases.
We report on two children with severe lupus nephritis (LN) treated with low-dose IVCY, oral MZB, and steroids who achieved complete remission with renal histological improvements in a short period of time and without significant adverse effects.
Case 1
A 12-year-old girl with a history of facial butterfly rash and fever for 2 weeks was initially admitted to a local hospital because of generalized edema, and was diagnosed as having SLE with renal involvement. She was referred to our hospital for renal biopsy 2 weeks later.
Her past medical history revealed she had been found to have microscopic hematuria at the age of 11 years, by a mass screening program for renal disease, without receiving further evaluation. There was no family history of autoimmune or renal disease.
On admission to our hospital, physical examination revealed a high blood pressure of 150/90 mmHg and temperature of 37.5°C. Her weight was 45 kg, which had increased by 3 kg compared with 1 month before admission. The butterfly rash over her cheeks and nose was noted. There was pitting edema of both lower extremities. Other physical examinations revealed nothing remarkable.
Laboratory investigations showed pancytopenia (white blood cell count 4,000 μL−1; hemoglobin 9.9 g dL−1; hematocrit 29.9%; platelets 45,000 μL−1), hypoproteinemia (serum total protein 4.9 g dL−1; serum albumin 2.0 g dL−1), slightly disturbed renal function (blood urea nitrogen (BUN) 31 mg dL−1; serum creatinine 0.84 mg dL−1), hypocomplementemia (C3 31 mg dL−1, normal >84; C4 <5 mg dL−1, normal >14). Serum titers of liver enzyme and electrolytes were within normal limits. Immunological investigations were positive for antinuclear antibody (1:640, homogeneous pattern) and anti-double-stranded DNA antibody (>400 IU mL−1, normal <10) whereas anticardiolipin antibody, anti-Sm antibody, anti-SS-A antibody, anti SS-B antibody, anti-RNP antibody, and rheumatoid factor were not detected.
Urinalysis showed 3+ for hematuria, 3+ for proteinuria, and a few granular, hyaline, and erythrocyte casts.
Diagnosis of severe LN with nephrotic syndrome was made on the basis of these clinical and laboratory findings and a first renal biopsy was performed in February 2004 (Fig. 1A). The renal pathology showed class IV-G(A) lesion, by the International Society of Nephrology/ Renal pathology Society (ISN/RPS) classification [9], as diffuse global proliferative lupus nephritis with diffuse wire-loop deposits. There were also hyaline thrombi in 3 (15.8%) and cellular crescents in 5 (26.3%) of 19 glomeruli, although no significant interstitial lesions were seen. Immunofluorescence study (IF) showed diffuse granular mesangial and peripheral capillary loop staining for IgG, IgA, IgM, C1q, and C3. Furthermore, mesangial and subendothelial electron-dense deposits were found by electron microscopy.
A Renal histology before induction therapy in Case 1. The glomerulus displays global intracapillary cellular proliferation with hyaline intracapillary thrombi (PAM×200). B Renal histology after induction therapy in Case 1. The glomerulus shows segmental areas of sclerosis without changes of active lesions (PAM×100)
The patient was treated with daily intravenous methylprednisolone (20 mg kg−1) for 3 days followed by oral prednisolone (PSL, initially 40 mg day−1 and then tapered at 2.5 mg every 2 to 4 weeks). After intravenous methylprednisolone administration the patient received, with informed parental consent, combined therapy of 6-monthly IVCY (500 mg m−2, cumulative dose 3 g m−2) and oral MZB (5 mg kg−1 day−1) to prevent the adverse effects of long-term high-dose IVCY regimen.
After the third dose of IVCY she achieved remission both clinically and serologically. There were no clinical signs of lupus; the anti-ds DNA antibody turned to negative; serum levels of complements and protein and renal function normalized; and urinalysis showed no proteinurea or hematuria.
The dose of PSL was tapered to 10 mg day−1 during the 6 months of low-dose IVCY therapy.
Serious complications such as amenorrhea, severe bacterial infection, and hemorrhagic cystitis did not develop.
A second renal biopsy was performed in August 2004 for evaluation of the efficacy of the treatment (Fig. 1B). Renal pathology showed significant improvement as focal sclerosing glomerulonephritis (class III-C).
Case 2
A 12-year-old boy was referred to our hospital from a local hospital for further evaluation of persistent fever and pancytopenia.
He had been previously healthy until this referral. His family history was remarkable for SLE in his maternal aunt and idiopathic thrombocytopenic purpura in his grandmother.
On admission, physical examination revealed a blood pressure of 130/70 mmHg and a high temperature of 40.5°C. Cervical lymph nodes were enlarged in size (diameter 3 cm) and hepatosplenomegaly was noted. Other physical examinations revealed nothing remarkable
Laboratory investigations showed pancytopenia (white blood cell count 1,000 μL−1; hemoglobin 9.2 g dL−1; hematocrit 29.9%; platelets 64,000 μL−1), hypoproteinemia (serum total protein 5.8 g dL−1; serum albumin 3.2 g dL−1), slightly disturbed renal function (BUN 25 mg dL−1, serum creatinine 0.93 mg dL−1), liver dysfunction (aspartate aminotransferase 292 IU L−1, alanine aminotransferase 197 IU L−1), and hypocomplementemia (C3 22 mg dL−1, C4<5 mg dL−1). Serum electrolytes were within normal limits. Immunological investigations revealed a positive antinuclear antibody (1:320) with a homogeneous pattern and an elevated anti-double-stranded DNA antibody level of 34.6 IU mL−1 (normal <10). Anticardiolipin antibody, anti-Sm antibody, anti-SS-A antibody, anti SS-B antibody, anti-RNP antibody, and rheumatoid factor were negative. Urinalysis showed 2+ of hematuria and 1+ of proteinuria.
Diagnosis of LN was made on the basis of on these findings and a first renal biopsy was performed in April 2004 (Fig. 2A). The renal pathology showed class III-A lesion by ISN/RPS classification as focal proliferative LN with focal subendothelial deposits and diffuse mesangial proliferation. No crescent, hyaline thrombi, or interstitial lesions were seen. IF showed diffuse granular mesangial and peripheral capillary loop staining for IgG, IgA, IgM, C1q, and C3. Mesangial and subendothelial electron-dense deposits were seen by electron microscopy. The patient was treated with the same regimen as case 1 and achieved remission after the second dose of IVCY. Six months later the PSL dosage was reduced to 10 mg day−1 because no clinical signs of lupus were evident and all results from blood examinations were within normal levels.
A Renal histology before induction therapy in Case 2. The glomerulus displays segmental endocapillary proliferative lesions with subendothelial deposits (AFOG×200). B Renal histology after induction therapy in Case 2. The glomerulus shows segmental mesangial hypercellularity without obsolescence of the glomerular capillary lumina. (PAM×200)
During this combined therapy, no serious complications developed.
A second renal biopsy was performed in October 2004 (Fig. 2B) and its pathology showed significant improvement—mesangial proliferative LN without endothelial deposits (class II).
Discussion
Since prospective trials performed by the National Institutes of Health (NIH) that demonstrated the superiority of a long-term high-dose IVCY regimen, in combination with glucocorticoids, over oral or IV glucocorticoids therapy alone [10, 11, 12, 13], this NIH regimen has become the standard treatment of adults with proliferative LN and has been similarly applied to childhood LN with excellent prognosis [14, 15].
However, the high prevalence of serious adverse effects such as severe infection, avascular necrosis, or ovarian failure, could not be disregarded, particularly in children and adolescents.
Recently, Houussiau et al. postulated that low-dose IVCY (cumulative dose 3 g, so-called the Euro-Lupus Trial regimen) effectively induces remission in adults with proliferative LN demonstrating renal remission and renal flares comparable with the remission achieved with a conventional high-dose IVCY regimen [16]. They also stated that the frequency of severe infection in low-dose IVCY was less than half of that in high-dose IVCY. There is currently scarce information regarding the outcome of low-dose IVCY regimen in children with lupus nephritis, although many pediatric renal units use something very similar to the Euro-Lupus Trial regimen routinely.
MZB is less toxic than other immunosuppressants, especially with regard to both bone marrow and liver function [17]. Several papers have reported the use of MZB in the treatment of lupus nephritis in children [7, 8]. Our regimen is, however, different from those in these papers in both duration (our report, 6 months; Tanaka, 2 years; Yoshidome, 1 year) and timing (our report, induction therapy; Tanaka, maintenance therapy; Yoshidome, mean disease duration was 4.8 years at initiation of MZB) of MZB treatment.
With regard to mode of action, that of MZB, a selective inhibitor of inosine monophosphatase dehydrogenease in the de novo pathway, resulting in suppression of proliferation of T and B lymphocytes and antibodies [18], is very similar to that of mycophenolate mofetil (MMF) which has been reported to be effective in the treatment of lupus nephritis [19].
For the purpose of reducing cumulative dose of CY and steroids, we also added oral MZB to the low-dose IVCY regimen for the initial induction, because childhood-onset SLE is more acute and severe than adult SLE and younger patients are likely to require high-dose PSL [20]. As a result, significant improvement of histological and clinical manifestations was obtained in a short period of time. We therefore suggest MZB has an additive effect on low-dose IVCY and steroids, although this should be investigated with a larger number of patients.
For maintenance therapy after this induction therapy, our patients were given MMF and a tapering dose of PSL, because a recent prospective study demonstrated that short-term IVCY followed by maintenance therapy with MMF seemed more efficacious and safer than long-term IVCY [21]. Our 2 patients have remained in remission with low-dose PSL (case 1, 7.5 mg day−1; case 2, 6 mg day−1) and MMF (case 1, 1.5 g day−1; case 2, 1 g day−1) for more than 6 months after discontinuation of low-dose IVCY and oral MZB.
In summary, induction therapy of low-dose IVCY, oral MZB, and steroids may be an alternative means of achieving remission in children or adolescents with severe LN (class III or IV), for whom serious adverse effects such as gonadal toxicity are a concern. Further study is needed to confirm our preliminary findings.
References
Niaudet P (2000) Treatment of lupus nephritis in children. Pediatr Nephrol 14:158–166
Bartosh SM, Fine RN, Sullivan EK (2001) Outcome after transplantation of young patients with systemic lupus erythematosus: a report of the North America pediatric renal transplant cooperative study. Transplantation 72:973–978
Sonda K, Takahashi K, Fchinoue S, Hayasaka Y, Kawaguchi H, Teraoka S, Toma H, Oka K (1996) Clinical pharmacokinetic study of mizoribine in renal transplantation patients. Transplant Proc 28:3643–3648
Yoshioka K, Ohashi Y, Sakai T, Ito H, Yoshikawa N, Nakamura H, Tanizawa T, Wada H, Maki S (2000) A multicenter trial mizoribine compared with placebo in children with frequently relapsing nephrotic syndrome. Kidney Int 58:317–324
Kaneko K, Nagaoka R, Ohtomo Y, Yamashiro Y (1999) Mizoribine for childhood IgA nephropathy. Nephron 83:376–377
Nagaoka R, Kaneko K, Ohtomo Y, Yamashiro Y (2002) Mizoribine treatment for childhood nephropathy. Pediatr Int 44:217–223
Tanaka H, Tsugawa K, Tsuruga K, Nakahata T, Ito E, Waga S (2004) Mizoribine for the treatment of lupus nephritis in children and adolescents. Clin Nephrol 62:412–417
Yoshidome K, Takei S, Imanaka H, Maeno N, Ohkawa T, Kawano Y (2004) Efficacy of mizoribine in the treatment of systemic lupus erythematosus in children. Pediatr Int 46:444–449
Weening JJ, Agati DD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijin JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennete JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 65:521–530
Austin HA 3rd, Kipple JH, Balow JE, le Riche NG, Steinberg AD, Plotz PH (1986) Therapy of lupus nephritis: control trial of predonisone and cytotoxic drugs. N Eng J Med 314:614–619
Boumpas DT, Austin HA 3rd, Vaughan EM, Kipple JH, Steinberg AD, Yarboro CH (1992) Controlled trial of pulse methylpredonisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis. Lancet 340:741–745
Gourley MF, Austin HA 3rd, Scott D, Yarboro CH, Vaughan EM, Muir J (1996) Methylpredonisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. Ann Intern Med 125:549–557
Illei GG, Austin HA, Crane M, Collinins L, Gourley MF, Yarboro CH (2001) Combination therapy with pulse cyclophosphamide plus pulse methylpredonisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Ann Intern Med 135:248–257
Lehman TJ, Sherry DD, Wagner L, McCurdy DK, Emery H, Magilavy DB (1989) Intermittent intravenous cyclophosphamide therapy for lupus nephritis. J Pediatr 114:1055–1060
Lehman TJ, Onel K (2000) Intermittent intravenous cyclophosphamide arrests progression of the renal chronicity index in childhood systemic lupus erythematousus. J Pediatr 136:243–247
Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, Garrido ER, Danieli MG (2002) Immunosupressive therapy in lupus nephritis: the Euro-lupus nephritis trial. A randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 46:2121–2131
Kusaba R, Otubo O, Sugimoto H, Takahashi I, Yamada Y, Yamauchi J, Akiyama N, Inou T (1981) Immunosuppressive effect of bredinin in the management of patients with renal transplantation. Proc Eur Dial Transplant Assoc 18:420–425
Yokota S (2002) Mizoribine: mode of action and effects in clinical use. Pediatr Int 44:196–198
Chan TM, Li FK, Tang CSO, Wong RWS, Fang GX, Ji YL, Lau CS, Wong AKM, Tong MKL, Chan KW, Lai KN (2000) Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. N Eng J Med 343:1156–1162
Tucker LB, Menon S, Schaller JG, Isenberg DA (1995) Adult- and childhood-onset systemic lupus erytematosus: a comparison of onset, clinical features, serology, and outcome. Br J Rheumatol. 34:866–872
Contreras G, Pardo V, Leclercq B, Lenz O Tozman E, O’Nan P, Roth D (2004) Sequential therapy for proliferative lupus nephritis. N Eng J Med 350:971–980
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujinaga, S., Kaneko, K., Ohtomo, Y. et al. Induction therapy with low-dose intravenous cyclophosphamide, oral mizoribine, and steroids for severe lupus nephritis in children. Pediatr Nephrol 20, 1500–1503 (2005). https://doi.org/10.1007/s00467-005-1983-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-005-1983-9