Abstract
After failure of conservative treatment of neurogenic bladders (deterioration of the upper urinary tract/incontinence) continent cutaneous diversion has to be considered in those patients with irreparable urethral sphincter defects or those who are unable to perform trans-urethral self-catheterization. In this second part of the study we investigated the long-term safety of using the Mainz pouch I with regard to protecting the upper urinary tracts and to provide urine continence. Between 1985 and 2002, operations to form an ileocaecal pouch with umbilical stoma (Mainz pouch I) were performed on 70 children and adolescents of median age 15.3 years (range 5.7–20 years). During the follow-up period five patients died 2.4–14 years postoperatively of causes not related to urinary diversion. A follow-up period of 8.7 years (0.9–18) was achieved in 65 patients with 118 renal units (RUs). As compared to preoperatively, the upper urinary tracts had remained stable or improved in 113/118 RUs (95.8%) at the latest follow-up. Complete continence was achieved in 97% of patients with a continent cutaneous diversion. Surgical revisions were required for: incontinence of the outlet mechanism in 9%, stoma prolapse in 2%, stoma stenosis in 23%, pouch calculi in 15%, symptomatic reflux in 1%, ureter stenosis in 16% of the RUs with submucosal tunnel and in 3% of the RUs with an extramural tunnel. We conclude that, in patients with irreparable sphincter defect and those who are unable to perform urethral self-catheterization, continent cutaneous urinary diversion with the Mainz pouch I provides a high continence rate with preservation of the upper urinary tracts in the long run. In patients with dilated ureters, the extramural tunnel technique results in a lower complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with a neurogenic bladder, only after failure of all conservative treatment options should surgical intervention be considered. For patients with irreparable sphincter defects and those who are unable to perform trans-urethral self-catheterization our suggestion is continent cutaneous diversion. At our institution the options of urinary diversion are discussed during an interdisciplinary conference of neuro-paediatricians, neurosurgeons, paediatric nephrologists, orthopaedic surgeons and urologists, as well as with the patient and the parents (the options are listed in Part I).
In this second part of the study we investigated whether the use of the Mainz pouch I was safe in the long run and whether it could meet both the patient’s expectations and the physician’s concerns in this most difficult group of patients with neurogenic bladder.
Material and methods
Between 1985 and 2002, continent cutaneous diversion was performed in 70 children and adolescents under the age of 20 years. The aetiology of neurogenic bladder was meningomyelocele in 53 patients, caudal regression in two, anal atresia in eight, status post-(s.p.) urethral valve in two patients, s.p.-sacral dermoid in one and iatrogenic after multiple operations in the pelvis in three patients.
Twenty of the patients (28.6%) underwent conversion from another urinary diversion. Eight of these patients had a colonic conduit, six an ileal conduit, three had undergone an ileal bladder augmentation, two a Mitrofanoff procedure and one patient a ureterocutaneostomy, all of which, except for the colonic conduits, were performed in other institutions.
For the continence mechanism the appendix [1] was used in 32 patients (three died during the follow-up period), an intussuscepted ileal nipple in 26 patients (Fig. 2) [2], a seromuscularis bowel flap tube in three [3], a full-thickness bowel flap in one [4], a tapered ileum in three [5] and a Monti-procedure in one [6, 7]. In four patients from the initial series of Mainz pouch procedures [8] one had an alloplastic stoma, one a sutured ileal nipple and two a stapled and sutured ileal nipple (two of the four patients died during the follow-up period).
For the re-establishment of bowel continuity by “ileoascendostomy”, reconstruction of the ileocaecal valve was performed in 37 of the 65 patients (57%) operated on since 1992 [9].
The data from the follow-up studies were obtained from the charts in 41 of the 65 patients. All these patients were seen annually at our institutions. Follow-up visits included detailed history concerning complications of the urinary diversion, problems with clean intermittent self-catheterisation (CISC), urinary continence, and problems with bowel movements. Blood chemistry included serum creatinine, the electrolytes, vitamin B12 after the 5th year, and a capillary blood gas analysis. Ultrasonography of the urinary tract was performed. In the case of dilatation of the upper urinary tract, a MAG-III clearance was performed. In the remaining 14 patients, data were obtained by telephone interview with the patient or the parents and the outside urologist, who performs the ultrasonography and the laboratory investigations at least annually. Mostly, the patients were seen every 3–6 months.
The status of the upper urinary tract was investigated, using the last intravenous urography or renal ultrasound, and compared with the preoperative studies. The degree of dilatation of the upper urinary tract was classified into none, mild-to-moderate, or severe.
Continence was defined as being dry day and night without the need for a protective pad. Patients with a continent cutaneous stoma and wearing a protection pad to absorb mucous secretion were defined as continent, while those who required at least one pad to soak up urine were considered incontinent.
Renal function was assessed by serum creatinine level (normal concentration for adolescents: <120 μmol/l).
The acid–base balance was determined from capillary blood gas analysis. At base excess (BE) below −2.5 mmol/l, alkali substitution (e.g. sodium/potassium citrate) was recommended (normal range is between +2.5 and −2.5 mmol/l).
After the 10th year, annual pouchoscopy was performed to exclude secondary malignancy or was performed in cases of haematuria or suspicion of a tumour after sonographic examination.
Results
Of the 70 patients with a Mainz pouch I, five died after a mean of 8.4 years (range 2.4–14 years) from reasons unrelated to urinary diversion; 65 patients with 118 renal units (RUs) had a mean follow-up period of 8.7 years (range 0.9–18 years; median 8.9 years). The mean age of patients at the time of operation was 15.1 years (range 5.7–20 years; median 15.3 years). A total of 37 patients (57%) developed 66 complications requiring re-operation, which was a minimally invasive procedure in 37 of the 66 complications (56%).
Surgical complications
Postoperative adhesive ileus occurred in two of the 65 patients (3%) requiring re-operation.
Upper urinary tract
Ureteral implantation was accomplished by a submucosal tunnel technique in 45 patients with 81 RUs, including eight patients with 14 RUs converted from a colonic conduit without re-implantation, a serous-lined extramural tunnel technique in 15 patients with 29 RUs, and various techniques in the remaining five patients with eight RUs. Regardless of the operating technique for ureteral re-implantation, five of the 118 RUs (4.2%) in the continent cutaneous diversion group showed an increasing dilatation of the upper urinary tract in the long-term follow-up. The ureteral re-implantation rate of the continent cutaneous group (65 patients and 118 RUs), independent of the technique used, was 12.7% of the RUs (12 patients and 15 RUs (nine unilateral, three bilateral)).
At the latest follow-up, ten of the 81 (12%) submucosally implanted RUs had improved, 67 (83%) were normal or had remained stable and four (5%) had an increasing upper tract dilatation. Re-operation due to stenosis of the uretero-intestinal implantation was required in 13 of 81 RUs (16%) (ten patients: three with bilateral stenoses, seven with unilateral stenosis) after a mean of 38 months (4–137 months). Of these 13 RUs, eight had already been dilated preoperatively. All the 13 re-implanted RUs remained stable or improved during the follow-up period. In one of these patients a secondary ureteropelvic obstruction was successfully corrected by Anderson Hynes pyeloplasty 6 months before ureteral re-implantation was performed.
The technique of serous-lined extramural tunnel ureteral implantation [10] was initiated in 1994 for dilated ureters that revealed thickened walls intraoperatively. After a mean follow-up of 5.4 years (range 0.9–8 years), at the latest ultrasound examination, 12 RUs (41%) had improved following serous-lined extramural tunnel implantation, 16 RUs (55%) had remained stable and one RU showed an asymptomatic increase in dilatation. Re-operation was performed in three RUs, one for symptomatic stenosis at the uretero-intestinal anastomosis 22 months postoperatively. At the latest follow-up the dilatation was the same as before the Mainz pouch operation. Ureterolysis was performed successfully in another patient, 2 months postoperatively, with symptomatic increasing upper tract dilatation, and, in the same patient, the second RU was re-implanted because of symptomatic reflux 62 months later. The dilatation of both RUs had improved when compared with that at the preoperative ultrasound.
The remaining eight RUs in five patients that had undergone different implantation techniques remained stable during follow-up, and no surgical revision was required. In one case of ileal augmentation, partial ureter substitution by ileum end-to-side anastomosis without anti-reflux protection was carried out. In one further adolescent with an ileal conduit, borderline renal function (serum creatinine 150 μmmol/l) and the strong desire for continent diversion, conversion into continent cutaneous diversion was performed and the ileal conduit was incorporated into the reservoir without re-implantation of the dilated ureters. In another three patients with four severely dilated ureters, end-to-side implantation of ureters without anti-reflux protection was performed.
Continence
Twenty-eight of the 29 patients with an appendix stoma (Fig. 1) [1] were continent; in one patient re-operation (conversion to an intussuscepted ileal nipple) was performed 6 years later. Two of 26 patients (7.7%) with an intussuscepted ileal nipple (Fig. 2) [2] required re-operation for incontinence. One of these two underwent conversion back to the bladder with augmentation of the bladder by the pouch in another institution, after which she is continent for 3–4 hours. Two additional patients, one with an alloplastic stoma and one with a sutured ileal nipple, and one of three patients with a seromuscularis bowel flap tube [11] required operative revision of the continence mechanism. One continent patient with an intussuscepted ileal nipple underwent revision for nipple gliding.
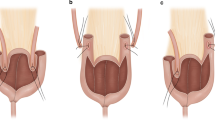
For the creation of an ileocaecal pouch with appendix stoma, two loops of ileum (2 cm×12 cm) and one loop of the colon ascendens, including the ileocaecal valve (12 cm), are isolated (a). The appendix is opened and dilation performed, followed by creation of a 6–7 cm long submucosal tunnel by incision of the seromuscular layer, leaving only the mucosa untouched. After insertion of a silicone catheter and creation of mesenteric windows without compromising the blood supply (b), the appendix is placed into the prepared bed and the sutures are positioned, grasping the seromuscularis through the windows (c)
After isolation of intestinal segments and anti-mesenteric opening of the bowel, a side-to-side anastomosis of the terminal and next ileal loop is done (a). For “nipple” construction the fatty tissue and the serosa are removed, leaving the vessels untouched (b) and by means of two Allis clamps the invagination of the ileum is performed. Fixation of the invagination is with two rows of staplers at the 3 o’clock and 9 o’clock positions. The completed invagination is pulled through the ileocaecal valve and the intussusception is subsequently fixed by a third row of staples at the 12 o’clock position (c)
Further pouch-related complications
Additional complications of continent cutaneous diversion compromise the development of stoma stenosis and pouch calculi. Stoma stenosis at the skin level developed in nine of 29 (31%) patients with an appendix stoma, requiring five endoscopic and ten open procedures. Four of the 26 patients (15.4%) with an intussuscepted ileal nipple developed stoma stenosis and required four endoscopic and two open treatments. One of the three patient with a seromuscularis bowel flap tube and one of the three patients with a tapered ileal segment stoma stenosis required surgical correction.
Four patients with an appendix stoma developed pouch calculi (13.8%). Six patients with an ileal outlet developed calculi in the pouch, mostly due to the metal staples (23.1%). The stones were removed endoscopically in five patients and required pouchotomy for stone extraction in the others.
Stool frequency: Of the 65 patients available for follow-up in whom the ileocaecal segment was excluded from bowel continuity, 37 underwent reconstruction of the ileocaecal valve in an attempt to prevent an increase in stool frequency. In this group no increase in stool frequency was seen in 29/37 patients (76%). Nine of the 37 patients (24%) took loperamide or cholestyramine for regulation of stool frequency. Eighteen of 28 patients (64%) without valve reconstruction had no increase in stool frequency, while four of 28 patients (14%) took loperamide or cholestyramine.
Renal function: Serum creatinine was elevated preoperatively in six of 65 patients. Renal function remained stable in five patients with elevated serum creatinine and deteriorated gradually in another requiring haemodialysis. This latter patient experienced renal transplantation followed by rejection and donor graft explantation. None of the patients with a preoperative normal serum creatinine level developed renal failure.
Acid–base balance: During the follow-up period the base excess dropped temporarily below −2.5 mmol/l in ten of the 65 patients followed-up. None of them developed clinical acidosis (fatigue, inappetence or nausea) or decrease in blood pH and significant serum electrolyte disturbances (hyperchloraemia, hyperkalaemia); 30/65 patients were using prophylactic alkali substitution at the latest follow-up.
Secondary malignancy: None of the 65 patients developed a bowel neoplasm.
Discussion
After failure of conservative treatment (pharmacotherapy, Botox injections, CISC and prophylactic antibiotics), operating options have to be discussed with the patient. From the patient’s view urinary incontinence is the main problem, and Börjeson et al. reported it to be the primary reason for social isolation of these patients [12]. Incontinence may be caused by irregular intervals of CISC due to decreased compliance of the patients or by technical problems secondary to obesity and handicap (wheelchair bound), or reduction or discontinuation of pharmacotherapy because of side effects.
Bladder augmentation or substitution with ureteral re-implantation is a commonly used surgical technique in neurogenic bladders [13, 14], but in patients with irreparable sphincter defects or those who are unable to perform CISC, continent cutaneous diversion is a reasonable alternative to bladder augmentation.
Calculi formation may occur in 18–52% of patients with bladder augmentation [15, 16, 17]. In our group of patients with an ileocaecal pouch, calculus formation was mostly related to metal staples used to create an ileal intussusception nipple. With generous irrigation of the pouch at regular intervals, the incidence of calculus formation can be decreased. Bladder perforation in augmented bladders is a rare but serious complication, which had a fatal outcome in three of 12 patients in one series [18]. Perforation occurs nearly always at the site of anastomosis of bowel and bladder and may be related to ischaemia. None of the patients with continent diversion had this complication.
A high continence rate is an advantage of continent cutaneous diversion over bladder augmentation. Of our patients with an embedded appendix or an ileal intussusception nipple as the continence mechanism, 97% were continent at the latest follow-up. Even though, in 24 patients, data were obtained by a detailed telephone interview, the continence status seemed to be accurate, because an incontinent patient will complain about it. CISC through an umbilical stoma, as compared with through the urethra, is an advantage for wheelchair-bound patients (50% of meningomyelocele patients in our series) and obese patients (Fig. 3). The high rate of stoma stenosis in patients with an appendix stoma is a disadvantage, even if the stenosis may be corrected by a minimally invasive procedure.
When the options of surgical intervention in this group of patients is discussed, future changes of neurological and orthopaedic status with increasing age should be considered. Hunt and Poulton reported on a cohort of 117 newborn infants with spina bifida. In a longitudinal survey, at a mean age of both 9 years and 18 years approximately 50% of patients were ambulatory. At a mean age of 25 years, however, only 20 of the 61 patients who were alive were still ambulatory. Especially in the group of patients with a lumbar lesion, mobility changes after puberty [19]. In our group of 70 patients with continent cutaneous diversion the neurological condition deteriorated in four of them. Two are now catheterised by their relatives, two died from neurological complications, in one a conversion to a conduit was performed 3 years prior to his death, and the other was treated by an indwelling catheter for 4 years as she was unable to perform clean intermittent catheterisation herself. Despite careful selection of our patients not all of them had a sustained benefit from continent cutaneous diversion in the long run.
Using the Kock pouch in 20 children and adolescents, Abd-el-Gawad et al. reported, in ten of 13 children (77%) and in three of seven adolescents (43%), pouch-related complications (calculus formation in six patients, stoma prolapse in three, angulation of the efferent segment in six, reflux in two, deterioration of renal function in eight, stoma stenosis in three) after a follow-up period of 6.5 years [20, 21].
Herschorn et al. have a re-operation rate of 36% in patients with bladder augmentation due to neurogenic bladder after 6 years, which is similar to that for our series [13]. Husmann and Cain reported a re-operation rate of 48% in 62 patients with ileocaecal bladder augmentation and a cutaneous stoma for CISC (Hemi-Indiana pouch) [22].
Ureteral implantation is a crucial point in urinary diversion, specifically with dilated ureters as a common indication for urinary diversion. In our group of patients with a submucosal tunnel implantation into the large bowel, 16% of the RUs required re-implantation due to obstruction of the uretero-intestinal anastomosis. The serous-lined extramural tunnel technique [10] has proven to be superior for dilated ureters: after a mean follow-up time of 5.4 years, one in 29 RUs (3%) required ureteral re-implantation. Recently, the necessity of anti-refluxive ureter implantation has been discussed [23, 24, 25, 26]. Clearly, there is a need for a prospective randomized study on the impact of reflux from a potentially contaminated reservoir. Until evidence is obtained that even low-pressure reflux does not harm the kidneys in the long run, young patients with a long life expectancy should be protected from developing renal scars by an appropriate anti-reflux technique.
During or after puberty some young adults with incontinent urinary diversion seek conversion to a continent diversion as the body image becomes more important. In the current series, 16% of patients with a colonic conduit underwent conversion to continent urinary diversion, and approximately one in three of all patients with continent diversion had had various previous types of incontinent diversion. Herschorn et al. reported a comparable series of 20 patients with myelodysplasia and incontinent diversion in whom un-diversion was carried out [27]. In a recent published series from our institution that comprised 39 patients (children and adults), we demonstrated the operating technique to avoid too much bowel resection and the feasibility of a conversion from a conduit diversion (ileum or colon) to a continent cutaneous diversion with an acceptable complication rate [28].
Exclusion of bowel segments and the ileocaecal valve can shorten the intestinal transit time and may result—especially in patients with neurogenic deficit—in faecal frequency and even faecal incontinence [22, 29, 30]. There are only a few reports in the literature concerning bowel dysfunction after urinary diversion. Increased faecal frequency was reported to develop after ileal or colonic conduit diversion in 11%–33% of patients, after bladder augmentation/substitution in 22%–27%, and after continent cutaneous diversion in 20%–23% [31, 32, 33, 34]. In the 65 patients of our series who underwent resection of the ileocaecal segment, the ileocaecal valve was reconstructed in 37 patients. Retrospectively, we did not find a statistically significant difference between patients with and without reconstruction of the ileocaecal valve. An alternative may be to construct a reservoir using solely the large bowel. However, even the use of the sigmoid colon for bladder augmentation may result in severe diarrhoea [31].
Hyperchloraemic metabolic acidosis, the most common electrolyte abnormality seen in intestinal urinary diversion [35], was not observed in our series of patients due to prophylactic correction of a negative base excess (e.g. BE <−2.5 mmol/l). A decrease in vitamin B12 levels, which was demonstrated in other series following ileal resection [36, 37], was not observed in children with an ileocaecal reservoir [38, 39].
Secondary malignancies represent a further important late complication of intestinal urinary diversion [40], for which screening of adult patients after more than 5 years of diversion and in children starting in the 10th year is recommended. None was found in our series of 65 patients after an average follow-up period of 8.7 years (range 0.9–18 years).
Conclusion
In patients with neurogenic bladders and failure of conservative treatment, urinary diversion is a viable compromise between the urologists’ concerns and the patients’ desire, as it can protect the upper urinary tracts in the long term and provides, at the same time, high continence rates. In patients who are unable to perform CISC through the urethra or in patients with an irreparable sphincter defect, a continent umbilical stoma offers a good alternative, especially in obese, immobile or wheelchair-bound patients. The serous-lined extramural tunnel technique has proven to be superior to submucosal implantation in patients with fibrotic and dilated ureters.
References
Bürger R, Riedmiller H, Müller SC, Hohenfellner R (1989) Kontinente Harnableitung—Mainz Pouch mit Appendix-Stoma. Akt Urol 20:I—IV
Thuroff JW, Alken P, Riedmiller H, Jacobi GH, Hohenfellner R (1988) 100 cases of Mainz pouch: continuing experience and evolution. J Urol 140:283–288
Lampel A, Hohenfellner M, Schultz-Lampel D, Thuroff JW (1995) In situ tunneled bowel flap tubes: 2 new techniques of a continent outlet for Mainz pouch cutaneous diversion. J Urol 153:308–315
Fichtner J, D’Elia G, Leissner J, Fisch M, Abol-Einein H, Hohenfellner R (1996) Kontinente Zökostomie. Akt Urol Operative Techniken 27:I—VI
Managaze L, Tschigogidze T (1993) Tiflis-Pouch. Akt Urol 24:I-VI
Monti PR, Lara RC, Dutra MA, De Carvalho JR (1997) New technique for construction of efferent conduits based on the Mitrofanoff principle. Urology 49:112–115
Yang WH (1993) Yang needle tunneling technique in creating antireflux and continent mechanism. J Urol 150:830–834
Thüroff JW, Alken P, Engelmann U, Riedmiller H, Jacobi GH, Hohenfellner R (1985) The Mainz pouch (mixed augmentation ileum and cecum) for bladder augmentation and continent urinary diversion. World J Urol 3:194–196
Fisch M, Wammack R, Spies F, Muller SC, Mokthar A, Ghoneim M, Hohenfellner R (1994) Ileocecal valve reconstruction during continent urinary diversion (comments). J Urol 151:861–865
Abol EH, Ghoneim MA (1994) A novel uretero-ileal reimplantation technique: the serous lined extramural tunnel. A preliminary report. J Urol 151:1193–1197
Lampel A, Hohenfellner M, Schultz-Lampel D, Wienold D, Thüroff JW (1993) Submucöser Seromuskularis-Konduit: Eine neue Technik des kontinenten Stomas beim Mainz-Pouch. Akt Urol 24:I-VIII
Börjeson M-C, Lagergren J (1990) Live conditions of adolescents with myelomeningocele. Dev Med Child Neurol 32:698–706
Herschorn S, Hewitt RJ (1998) Patients’ perspective of long-term outcome of augmentation cystoplasty for neurogenic bladders. Urology 52:672–678
Kaufman AM, Ritchey ML, Delbert AC, Rudy DC, McGuire EJ (1996) Decreased bladder compliance in patients with myelomeningocele treated with radiological observation. J Urol 156:2031–2033
Blyth B, Ewalt DH, Duckett JW, Snyder III HM (1992) Lithogenic properties of enterocystoplasty. J Urol 148:575–577
Hendren WH, Hendren RB (1990) Bladder augmentation: experience with 129 children and young adults. J Urol 144:445–453; discussion 460
Kronner KM, Casale AJ, Cain MP, Zerin MJ, Keating MA, Rink RC (1998) Bladder calculi in the pediatric augmented bladder. J Urol 160:1096–1098; discussion 1103
Bauer SB, Hendren WH, Kozakewich H, Maloney S, Colodny AH, Mandell J, Retik AB (1992) Perforation of the augmented bladder. J Urol 148:699–703
Hunt GM, Poulton A (1995) Open spina bifida: a complete cohort reviewed 25 years after closure. Dev Med Child Neurol 37:19–29
Abd-el-Gawad G, Abrahamsson K, Hanson E, Norlen L, Sillen U, Stokland E, Hjalmas K (1999) Kock urinary reservoir maturation in children and adolescents: consequences for kidney and upper urinary tract. Eur Urol 36:443–449
Abd-el-Gawad G, Abrahamsson K, Hanson E, Norlen L, Sillen U, Sixt R, Hjalmas K (1999) Evaluation of Kock urinary reservoir function in children and adolescents at 3–10 years’ follow-up. Scand J Urol Nephrol 33:149–155
Husmann OA, Cain MP (2001) Fecal and urinary continence after ileal cecal cystoplasty for the neurogenic bladder. J Urol 165:922–925
Abol-Enein H, Ghoneim MA (2001) Functional results of orthotopic ileal neobladder with serous-lined extramural ureteral reimplantation: experience with 450 patients. J Urol 165:1427–1432
Helal M, Pow-Sang J, Sanford E, Figueroa E, Lockhart J (1993) Direct (nontunneled) ureterocolonic reimplantation in association with continent reservoirs. J Urol 150:835–837
Pantuck AJ, Han KR, Perrotti M, Weiss RE, Cummings KB (2000) Ureteroenteric anastomosis in continent urinary diversion: long-term results and complications of direct versus nonrefluxing techniques. J Urol 163:450–455
Hohenfellner R, Black P, Leissner J, Allhoff EP (2002) Refluxing ureterointestinal anastomosis for continent cutaneous urinary diversion. J Urol 168:1013–1016; discussion 1016–1017
Herschorn S, Rangaswamy S, Radomski SB (1994) Urinary undiversion in adults with myelodysplasia: long-term follow-up. J Urol 152:329–333
Pahernik S, Stein R, Hohenfellner M, Thuroff JW (2004) Conversion from colonic or ileal conduit to continent cutaneous urinary diversion. J Urol 171:2293–2297
Gillitzer R, Fisch M, Jessel D, Schumacher S, Hohenfellner R, Thüroff JW (1998) Competence and function of the ileocecal valve reconstruction during urinary diversion (Mainz pouch I). J Urol 161:66A
Gonzales R, Cabral BHP (1983) Rectal incontinence after enterocystoplasty. Pediatr Dialogues 10:4–5
Singh G, Thomas DG (1997) Bowel problems after enterocystoplasty. Br J Urol 79:328–332
N’Dow J, Leung HY, Marshall C, Neal DE (1998) Bowel dysfunction after bladder reconstruction. J Urol 159:1470–1474; discussion 1474–1475
Roth S, Semjonow A, Waldner M, Hertle L (1995) Risk of bowel dysfunction with diarrhea after continent urinary diversion with ileal and ileocecal segments. J Urol 154:1696–1699
Henningsohn L, Wijkstrom H, Dickman PW, Bergmark K, Steineck G (2001) Distressful symptoms after radical cystectomy with urinary diversion for urinary bladder cancer: a Swedish population-based study. Eur Urol 40:151–162
McDougal WS (1992) Metabolic complications of urinary intestinal diversion. J Urol 147:1199–1208
Canning DA, Perman JA, Jeffs RD, Gerhart JP (1989) Nutritional consequences of bowel segments in the lower urinary tract. J Urol 142:509–511
Akerlund S, Delin K, Kock NG, Lycke G, Philipson BM, Volkmann R (1989) Renal function and upper urinary tract configuration following urinary diversion to a continent ileal reservoir (Kock pouch): a prospective 5 to 11-year follow-up after reservoir construction. J Urol 142:964–968
Stein R, Fisch M, Beetz R, Matani Y, Doi Y, Hohenfellner K, Burger RA, Abol-Enein H, Hohenfellner R (1997) Urinary diversion in children and young adults using the Mainz pouch I technique. Br J Urol 79:354–361
Stein R, Lotz J, Andreas J, Fisch M, Prellwitz W, Hohenfellner R, Thuroff JW (1998) Long-term metabolic effects in patients with urinary diversion. World J Urol 16:292–297
Kälble T, W. S, Berger MR, Waldherr R, Amelung F, Möhring K, Staehler G (1993) Karzinomrisiko in verschiedenen Formen der Harnableitung unter Verwendung von Darm. Akt Urol 24:1–7
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was presented at the AAP 2002 in Boston, Mass., USA
Part I of the article can be found at http://dx.doi.org/10.1007/s00467-005-1847-3 and Part III at http://dx.doi.org/10.1007/s00467-005-1849-1
Rights and permissions
About this article
Cite this article
Stein, R., Wiesner, C., Beetz, R. et al. Urinary diversion in children and adolescents with neurogenic bladder: the Mainz experience. Pediatr Nephrol 20, 926–931 (2005). https://doi.org/10.1007/s00467-005-1848-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-005-1848-2