Abstract
Kidney disease has not been considered a frequent complication in Down syndrome (DS) patients; a variety of urological abnormalities and glomerulopathies have been reported in this population, and some DS patients develop chronic renal failure (CRF).The aim of this study was to improve the understanding of renal disease in patients with DS, focusing on the incidence and range of kidney and urological abnormalities in a population of DS patients. A cross-sectional study was carried out in DS patients referred from a pediatric genetics unit of a tertiary care center. Medical records were reviewed. A 24-h urine specimen and a blood sample were obtained. Fractional excretion of sodium and potassium, tubular reabsorption of phosphate, urinary excretion of calcium, magnesium, uric acid, creatinine clearance and proteinuria were determined. Ultrasound was performed to evaluate the kidneys and the urinary tract. Laboratory data were reviewed for any possible renal disorder. Sixty-nine patients, aged 12 months to 24 years, were recruited. Pathological findings included three cases of voiding disturbances and a case of hypertension in a 7-year old girl. Eight patients (11.6%) had hyperuricemia without gout. Eighteen patients (24.2%) had hyperuricosuria. Urinalysis revealed three cases of mild proteinuria and two patients with microscopic hematuria. Minor radiological abnormalities were found in five patients (7.3%). Three patients (4.5%) had CRF. Renal disease in patients with DS is not as rare as previously thought, although the majority of findings are of minor relevance. According to the variety of pathologies, and in order to detect early irreversible renal injury, it seems quite reasonable to perform regular monitoring of renal function in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Down syndrome (DS) is the most common chromosomal abnormality, with a prevalence of 1–2 cases per 1,000 births. DS has many manifestations that can affect multiple organ systems, but kidney disease has not been typically considered a frequent complication. Reports of patients with renal diseases are increasing, partially due to increased survival [1]. A variety of urological abnormalities have been described such as ureteropelvic junction obstruction [2], vesicoureteral reflux [3], renal hypoplasia [4], obstructive uropathy or posterior urethral valves [5]. Glomerulopathies have also been reported, including membranoproliferative glomerulonephritis [6], immunoctactoid (amyloid-like glomerular deposits) glomerulopathy [7], focal and segmental sclerosis or hypercalcemia with medullary calcinosis [8]. A growing number of patients with DS who develop chronic renal failure (CRF) requiring renal transplantation or replacement therapy has been reported [9].
The aim of this study was to study the incidence of renal disease in a series of patients with DS followed up at a pediatric genetics department of a tertiary pediatric care center and to describe the main pathological findings.
Patients and methods
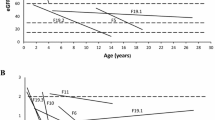
A cross-sectional study was carried out in patients with DS followed-up in a pediatric genetics unit of a tertiary hospital. All families were properly informed and gave their consent for participation. Children were referred to the division of pediatric nephrology for evaluation. Medical records were reviewed for age, gender, perinatal events and associated malformations. Families were instructed to collect a 24-h urine specimen. A blood sample was obtained at the completion of the urine collection; height, weight and blood pressure were measured. Hypertension was defined if systolic or diastolic blood pressure values exceeded the p95 of the reference values for each patient’s age, length and sex [10]. Kidney and urinary tract structures were evaluated by ultrasonography. Glomerular filtration rate (GFR) was estimated by the Schwartz formula [11] in girls and children younger than 14 years and by the Cockroft method in the adult patients [12]. CRF was defined as creatinine clearance below 70 ml/min/1.73 m2. Fractional excretion of sodium and potassium, tubular reabsortion of phosphate, urinary excretion of calcium, magnesium, uric acid and proteinuria were also determined and compared with reference values for the general population [13]. Hypercalciuria was defined as urine calcium excretion higher than 4 mg/kg/day. Uric acid excretion higher than 800 mg/day/1.73 m2 was considered as hyperuricosuria. Pathological proteinuria was defined by values higher than 4 mg/m2/h. All statistical analyses were performed using SPSS Software Package (SPSS, Chicago, Ill.).
Results
Sixty nine patients (37 boys, 32 girls) aged 12 months to 24 years (median 9.7 years) were recruited. Eighteen patients (26%) had congenital heart defects, all of them acyanotic.
Clinical findings
Five patients (four boys and a girl) had enuresis, a 7.5-year-old boy had sporadic urinary incontinence and a girl had pollakiuria. One patient (1.8%), a 7-year-old girl with normal renal function and no obesity, presented with hypertension.
Analytical data
GFR was determined in 66 patients, and three patients (4.5%) had CRF (Table 1), with no clinical symptoms and normal ultrasound. Eight patients (11.6%) presented with asymptomatic hyperuricemia.
Urinalysis revealed microscopic hematuria in two boys and mild proteinuria in three patients (all of them with normal renal function), whose clinical findings are explained in Table 2. Eighteen patients were found to have hyperuricosuria (24.2%). Four patients had asymptomatic hypercalciuria (two of them also had high urate excretion). No abnormalities in the fractional excretion of sodium, potassium and phosphate were found.
Only minor radiological abnormalities were detected in five patients (7.3%): bladder hypertrophy in a male with microscopic hematuria, medullary hyperechogenicity as the only finding in a case of asymptomatic hypercalciuria, ectopic left kidney, small kidney associated with pollakiuria and right kidney pyelectasia in a 7-year-old boy with nocturnal enuresis (Table 2).
Discussion
Down syndrome can affect multiple organ systems, although renal disease has been thought to be quite rare. In 1960, Berg et al. [2] described the first cases of DS with renal and urological malformations. Since them, published data concerning this issue have generally been restricted to sporadic case reports; only a descriptive study of DS patients with congenital heart disease focusing on kidney disease [14] and a review of the literature [15] have been reported previously. The incidence of renal and urological anomalies has been estimated as 3.5–21.4% [2, 4]. A variety of urological abnormalities have been described, including ureteropelvic junction obstruction, vesicoureteral reflux [3], renal hypoplasia [15], obstructive uropathy [4] and posterior urethral valves [5]. We have found a single case of asymptomatic renal pelvic dilatation and a patient with left kidney ectopia and no other clinical findings. Benaccerraf et al. [16] suggested that fetal pyelectasis could be associated with DS, but results are controversial; the risk of DS in isolated pyelectasis in a low risk population has been estimated as less than 1 in 340 [17]. Some authors suggest that the incidence of renal and urological anomalies in DS is high enough to encourage systematic screening [5, 15]. Thus, ultrasound should be performed in these infants early in life and, if abnormal, a voiding cystourethrogram to rule out any urological abnormality should also be performed.
To our knowledge, our study includes the largest population of young DS patients specifically investigated for renal disease. Urinalysis revealed five cases of hematuria and mild proteinuria as the only possible hint of glomerulopathy, and all of them had normal GFR. Pathological proteinuria was defined by a value higher than 4 mg/m2/h in a 24-h urine sample, but a postural element could have been present. We think that no specific glomerulopathy is associated with DS. Some autopsy studies in DS patients have reported “typical” histological findings, including glomerular microcysts, tubular dilatation and immature glomeruli [4, 18]. Ariel et al. [4] found 30 patients with cysts in the autopsy of urinary systems in 97 DS patients. Lo et al. [19] reported that cystic dilatation of Bowman’s space was more frequent than in the general population, and these findings were more common after the 1st decade of life. Acquired glomerulopathies have also been reported in DS patients, including membranoproliferative glomerulonephritis [6], inmunoctactoid glomerulopathy [7], focal and segmental sclerosis [19], amyloidosis [20] and hemolytic-uremic syndrome [9]. In addition, it has been reported that DS patients with autoimmune diseases (celiac disease, alopecia or hypothyroidism) may also present with primary glomerulonephritis [21], including two cases of anti-neutrophil cytoplasmic antibody-associated glomerulonephritis [22, 23]. It remains unclear, however, whether the coexistence of DS, autoimmune disorders and renal disease is somehow associated or whether it is just a coincidence due to their relatively common respective prevalence.
Four patients with asymptomatic hypercalciuria were detected. All of them had normal ultrasonographic findings, with the exception of one case of medullary hyperechogenicity with normal GFR. We think that these findings are different from previous reports of several patients with DS, hypercalcemia, hypercalciuria and medullary nephrocalcinosis [8, 24, 25] who progressed to renal insufficiency. A possible genetic predisposition to excessive dietary calcium absorption or a tubular disorder has been postulated to explain these cases [24].
Hyperuricemia and hyperuricosuria were the most frequent findings in our population. Increased serum uric acid level [26, 27] and the eventual development of gout [28, 29] have been previously documented. This could be explained by a decreased urinary clearance of uric acid [27] added to a decreased fractional excretion in DS patients [26]. Despite the relatively high frequency of uric acid disturbances observed, none of our patients developed gout.
We did not find malignant degeneration. Renal tumors in DS are extremely uncommon, and only four cases have ever been published: one malignant renal cancer of unstated histology [30], two nephroblastomas [31, 32] and one case of nephroblastomatosis [33].
Some DS patients develop end-stage renal disease, and we have found a CRF prevalence of 4.5% in our study, with unclear etiology. Two of our three patients with CRF are in their late teens, as are the majority of cases previously reported [9]. Two of these patients had acyanotic congenital heart defects (a 22-year-old female with an endocardial fusion defect and a 2.5-year-old boy with a ventricular septal defect), but we think there is no higher risk of CRF in patients presenting with these cardiovascular problems. Subrahmanyam et al. [14] have previously reported the results of 54 patients (40 of whom had congenital heart disease) and concluded that children with DS do not have a higher incidence of clinically significant renal anomalies compared to the general population.
CRF was defined by estimated GFR, using the Cockroft or Schwartz criteria, depending on age. Although it could be suggested, that this method is inaccurate as a sole indicator of impaired renal function, we think it could be enough as a screening test and regular follow-up should be carried out. Our patients have a mild impairment with GFR, and thus, conservative treatment was carried out and no biopsy performed. Renal transplantation is found to be a reasonable option in end-stage renal failure treatment for DS patients [34], and it seems to be the preferred treatment modality, although a few pediatric cases of DS on dialysis have been reported [35]. Nonetheless, the absence of other serious medical problems, level of psychomotor development and family support also must be taken into account in order to choose the best treatment option when the patient develops end-stage renal disease [36].
It is well known that DS patients are at a risk for infections, but we did not find a higher incidence of urinary tract infections compared with the general population.
Our population had an incidence of clinical symptoms of about 11.5%, mostly related to voiding disturbances, as others authors have previously noted [3]. According to our data, the incidence of renal anomalies in DS patients does not appear to be different when compared to the general population. We found that there are several signs and symptoms, most of them minor pathologies (hematuria, proteinuria or hypertension) that would require no treatment but rather follow-up. We consider that systematic follow-up of DS patients should be recommended: we suggest including a first evaluation (including ultrasound examination) and periodical urinalysis and serum creatinine levels determinations, synchronized with other regular blood analysis in DS patients.
In conclusion, renal disease in patients with DS is not very common, yet not rare, and it presents with a wide spectrum of findings. According to the variety of pathological findings, and in order to detect early CRF, it seems reasonable to perform regular monitoring of renal function in these patients.
References
Baird PA, Sadovnick AD (1989) Life tables for Down syndrome. Hum Genet 82:291–294
Berg JM, Crome L, France NE (1960) Congenital cardiac malformations in mongolism. Br Heart J 22:331–346
Ahmed S (1990) Vesico-ureteric reflux in Down syndrome: poor prognosis. Aust NZ J Surg 60:113–116
Ariel I, Wells TR, Landing BH, Singer DB (1991) The urinary system in Down syndrome: a study of 124 autopsy cases. Pediatr Pathol 11:879–888
Kupferman JC, Stewart CL, Kaskel FJ, Fine RN (1996) Posterior urethral valves in patients with Down syndrome. Pediatr Nephrol 10:143–146
Gupta SK, Venkataseshan VS, Churg J (1991) Mesangiocapillary glomerulonephritis in Down syndrome. Am J Nephrol 11:112–117
Takemura T, Yoshioka K, Akano N, Michihata I, Okada M, Maki S (1993) Immunotactoid glomerulopathy in a child with Down syndrome. Pediatr Nephrol 7:86–88
Proesmans W (1996) Hypercalcaemia, hypercalciuria and nephrocalcinosis in Down syndrome. Pediatr Nephrol 10:543–544
Kupferman JC, Stewart CL, Kaskel FJ, Katz SP, Fine RN (1994) Chronic peritoneal dialysis in a child with Down syndrome. Pediatr Nephrol 8:644–645
National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents (1996) Update on the 1997 task force report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program
Schwartz GJ, Haycock GB, Edelmann CM, Jr., Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Cockroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Santos F, García Nieto V (2000) Exploración basal de la función renal. In: Santos F, Garcia Nieto V (eds) Nefrologia pediatrica. Grupo Aula Medica SA, Madrid, pp 3–14
Subrahmanyam AB, Mehta AV (1995) Renal anomalies in Down syndrome. Pediatr Nephrol 9:253–254
Mercer ES, Broecker B, Smith EA, Kirsch AJ, Scherz HC, Massad A (2004) Urological manifestations of Down syndrome. J Urol 171:1250–1253
Benacerraf BR, Mandell J, Estroff JA, Harlow BL, Frigoletto FD Jr (1990) Fetal pyelectasis: a possible association with Down syndrome. Obstet Gynecol 76:58–60
Seeds JW (1998) Borderline genitourinary tract abnormalities. Semin Ultrasound CT MR 19:347–354
Gilbert EF, Opitz JM (1988) Developmental and other pathologic changes in syndromes caused by chromosomal abnormalities. Perspect Pediatr Pathol 7:1–63
Lo A, Brown HG, Fivush BA, Neu AM, Racusen LC (1998) Renal disease in Down syndrome: autopsy study with emphasis on glomerular lesions. Am J Kidney Dis 31:329–335
Husby G, Sletten K (1986) Amiloid proteins. In: Marrink J, van Rijswijk MH (eds) Amyloidosis. Nijhoff, Dordrecht pp 23–24
Birk PE, Burke BA, Vernier RL (1996) Glomerulonephritis in children with Down syndrome. Pediatr Nephrol 10:549
Robson WL, Leung AK, Woodman RC, Trevenen CL (1995) Anti-neutrophil cytoplasmic antibody associated glomerulonephritis in a patient with Down’s syndrome. Pediatr Nephrol 9:204–205
Schwab M, Boswald M, Ludwig K, Wittekind C, Waldherr R, Ruder H (1996) A patient with Down’s syndrome and anti-neutrophilic cytoplasmic antibody-positive vasculitis. Pediatr Nephrol 10:249–250
Andreoli SP, Revkees S, Bull M (1995) Hypercalcemia, hypercalciuria, medullar nephrocalcinosis, and renal insufficiency in a toddler with Down syndrome. Pediatr Nephrol 9:673
Cobenas C, Spizzirri F, Zanetta D (1998) Another toddler with Down syndrome, nephrocalcinosis, hypercalcemia, and hypercalciuria. Pediatr Nephrol 12:432
Coburn SP, Seidenberg M, Mertz EF (1967) Clearance of uric acid, urea and creatinine in Down syndrome. J Appl Physiol 23:579–580
Nishida Y, Akaoka I, Kobayashi M, Maruki K, Oshima Y (1979) Renal impairment in urate excretion in patients with Down’s syndrome. J Rheumatol 6:103–107
Nishida Y, Akaoka I, Nishizawa T, Maruki M, Aikawa T, Mitamura T, Yokohari R, Horiuchi I (1976) A case of gouty arthritis associated with Down’s syndrome. J Ment Defic Res 20:277–283
Ciompi ML, Bazzichi LM, Bertolucci MR, Mazzoni MR, Barbieri P, Mencacci S, Machia D, Mariani G (1984) Uric acid metabolism in two patients with coexisten Down syndrome and gout. Clin Rheumatol 3:229–233
Windham GC, Bjerkedal T, Langmark F (1985) A population-based study of cancer incidence in twins and in children with congenital malformations or low birth weight, Norway 1967–1980. Am J Epidemiol 121:49–56
Fabia J, Drolette M (1970) Malformations and leukemia in children with Down’s syndrome. Pediatrics 45:60–70
Kusumakumary P, Ninan M, Chellam VG, Jacob R, Nair MK (1995) Wilm’s tumor in a child with Down syndrome. J Pediatr Hematol Oncol 17:276
Saleun JP, Balouet G, Castel Y (1975) A case with transient leukoblastosis and renal dysembrioplasia. Nouv Presse Med 18:191
Baqi N, Tejani A, Sullivan EK (1998) Renal transplantation in Down syndrome: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Transplant 2:211–215
Hausmann MJ, Landau D (2002) A Down syndrome patient treated by peritoneal dialysis. Nephron 92:484–486
Riano I, Malaga S, Callis L, Loris C, Martin-Govante JM, Navarro M, Vallo A (2000) Towards guidelines for dialysis in children with end-stage renal disease. Pediatr Nephrol 15:157–162
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Málaga, S., Pardo, R., Málaga, I. et al. Renal involvement in Down syndrome. Pediatr Nephrol 20, 614–617 (2005). https://doi.org/10.1007/s00467-005-1825-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-005-1825-9