Abstract
Mortality from end-stage renal disease (ESRD) is often due to cardiac causes. Although cardiovascular complications of ESRD have long been recognized, only recently has the presence of traditional cardiovascular risk factors been associated with late cardiovascular complications. This review presents a history of cardiac involvement in ESRD, the pathophysiology of accelerated atherosclerosis and left ventricular hypertrophy, and a summary of the literature on cardiovascular risk assessment in children. Techniques for non-invasive assessment of cardiac end-organ injury are also discussed. Recommendations for monitoring of risk factors and treatment in the pediatric ESRD population are presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac complications of end-stage renal disease (ESRD) have assumed increasing importance, as cardiac disease now accounts for the majority of deaths in adults with ESRD, and about a quarter of pediatric ESRD deaths [1, 2, 3] (Fig. 1). The current literature describes a wide array of cardiovascular complications of ESRD, but there is little information on the natural history or efficacy of interventions to prevent cardiovascular complications. In particular, increasing attention has been paid to coronary artery disease and left ventricular (LV) dysfunction secondary to the presence of major cardiovascular risk factors after the onset of renal insufficiency. This manuscript will review the natural history of cardiac involvement with ESRD, with an emphasis on acquisition of morbidity secondary to sustained exposure to cardiovascular risk factors. Recommendations for evaluation and management to minimize life-long risk in pediatric patients will also be presented.
Cardiovascular mortality in pediatric end-stage renal disease (ESRD) according to dialysis modality and race (USRDS 1990–1996). Adapted from Ref. [1]
Interactions of ESRD with cardiac disease
Historically, cardiovascular complications were approached as either acute events requiring management or sequelae of ESRD itself where treatment of the underlying disease was the most prudent course. For example, arrhythmias were considered secondary to electrolyte imbalance from ESRD and congestive heart failure secondary to severe fluid retention. LV dilation and hypertrophy were also considered inevitable complications of hypertension, and management of hypertension was not focused on preventing complications. Over the last 2 decades, innovations in clinical management and associated improvements in outcome have suggested the need to revise this older paradigm. For example, introduction of erythropoietin prevented chronic severe anemia, and consequently prevented compensatory LV dilation [4] and reduced the prevalence of LV hypertrophy. Thus, anticipatory management could prevent known long-term cardiovascular complications.
Success with renal replacement therapy has lengthened life expectancy. Currently, mortality in patients with ESRD is not only related to renal replacement therapy but also to chronic diseases in other organ systems as a result of prolonged exposure to risk factors, particularly with regard to cardiovascular disease. Paradoxically, renal replacement therapy by either dialysis or transplantation may potentiate cardiovascular risk at the same time as it corrects underlying abnormalities of renal function. Management of renal failure alone is no longer the only determinant of long-term survival, and it is now critical to focus on co-morbid conditions to improve survival.
The cardiac abnormalities associated with ESRD are diverse. These include pericardial disease, arrhythmias, abnormalities of LV function, and coronary artery disease [1, 2]. Pericardial disease is most likely secondary either to the underlying cause of the renal disease or pro-inflammatory aspects of uremia [5]. Arrhythmias may be secondary to electrolyte imbalance, cardiomyopathy, and effects of medications or dialysis on myocardial repolarization. LV dysfunction is secondary to chronic anemia, hypertension, intravascular volume stresses (including fistulae for dialysis), and uremia [6, 7]. Coronary artery disease is secondary to the clustering of traditional cardiovascular risk factors (hypertension, dyslipidemia for example), as well as the presence of a pro-inflammatory state and endothelial dysfunction [8, 9, 10, 11]. In addition, novel risk factors such as C-reactive protein (CRP), lipoprotein (a) [Lp(a)], thrombotic factors, and homocysteine are impacted adversely by ESRD [10, 11, 12]. Of hospitalizations in pediatric patients with ESRD, 20% are reported to be due to arrhythmias, 10% to cardiomyopathy, and 3% to a cardiac arrest [13]. The incidence of cardiomyopathy has also doubled over the 6 years from 1991 to 1996 (Fig. 2) [13].
Annual cardiac events per 1,000 patient years in pediatric ESRD adjusted for age, sex, race, and primary ESRD diagnosis (USRDS 1991–1996). Adapted from Ref. [13]
Vascular injury
Vascular endothelium is the initial target for the proliferation of the atherosclerotic process [14]. Damage to the endothelium initiates a cycle of vascular smooth muscle proliferation and deposition in the intimal region of the vessel leading to fatty streak and plaque formation [14] (Fig. 3). This process of atherosclerosis results in “atheromas” in the intima of the vessel wall. There is reported subclinical evidence of atherosclerosis with intimal plaques in pediatric ESRD. In a series of children with iliac artery biopsy at the time of transplant, atherosclerosis in the uropathy group was also associated with increased serum calcium [15]. In otherwise healthy individuals, it is unusual for calcium to be incorporated into atherosclerotic plaques before the 4th or 5th decade of life.
Atherosclerosis is the most common form of arteriosclerosis but is only one form of arteriosclerosis. Arteriosclerosis is a group of diseases characterized by thickening and loss of elasticity of the arterial wall [16]. This is an important distinction especially in ESRD, as both forms are reported to occur in ESRD, and may have differing pathogenesis. Medial vessel calcification and arteriosclerosis or Monckeburg arteriosclerosis have also been shown in the pediatric ESRD population by vascular calcification in the coronaries, aorta, peripheral vessels, and aortic valves. Autopsy series of subjects with ESRD revealed soft tissue calcification in 60% of pediatric patients; 50% were on dialysis at the time of death [17]. Arteriosclerosis has also been described in a small series of patients, with four of eight patients having evidence of arteriosclerosis and diffuse vascular calcification and calcified valves [18].
Disruption of the endothelium integrity during arteriosclerosis may establish the inflammatory cascade for atherosclerotic plaque formation. Conversely, the atherosclerotic plaque may develop early in ESRD, and calcium deposition in the atherosclerotic plaque may be accelerated [19, 20]. There is also evidence of biomarkers of bone formation in the vasculature. This may promote progressive arterial wall calcification and stiffness, and worsening of both intimal and medial wall calcification [21, 22]. Increased parathyroid hormone (PTH) levels have been associated with increased coronary calcium [20] but not consistently [19], and the contribution of PTH metabolism to premature arterial calcification needs to be further elucidated.
Ventricular hypertrophy
The two most important factors contributing to the development of ventricular hypertrophy are hypertension and chronic volume overload, which are associated with chronic anemia and fluid retention. Hypertension increases ventricular afterload and causes left atrial dilation and LV hypertrophy as a compensatory mechanism (Fig. 3). Volume loading is an even more potent stimulus to the development of atrial dilation and ventricular hypertrophy. Arteriosclerosis results in stiffening of the aorta and large capacity arteries, and is a major determinant of LV pressure overload [16]. Arterial stiffening from vascular calcification has been shown to increase systemic pulse wave velocity, and afterload, which in turn impacts LV function.
There is evidence of increasing LV hypertrophy in children with chronic kidney disease (CKD) and ESRD [23]. LV hypertrophy occurs in 40%–75% of the pediatric ESRD population depending on the classification of LV hypertrophy [24, 25, 26, 27, 28]. At initiation of dialysis, 69% of subjects aged 4–18 years had evidence of LV hypertrophy [24]. Post-mortem studies have shown over 50% of children with ESRD have evidence of LV hypertrophy [18]. Chronic erythropoietin therapy has contributed significantly to the amelioration of this complication.
Cardiovascular risk factors in ESRD
Most risk factors for the development of chronic cardiovascular disease are present in a significant number of patients with ESRD. Not only are traditional cardiovascular risk factors such as hypertension and dyslipidemias present, but novel risk factors such as homocysteine and CRP are highly prevalent in the ESRD population as well.
Hypertension is seen in 49% of children with CKD [29] and 50%–60% [30] of patients on dialysis. Hypertension is more common in the transplant population, with 65%–80% of patients being treated [30]. In the young adult population, aged 18–35 years, systolic hypertension occurs in 51% and diastolic hypertension occurs in 35% of the dialysis population [31].
Lipoprotein abnormalities are increasingly recognized as complicating factors in ESRD. Approximately 29%–87% of pediatric peritoneal dialysis patients had low-density lipoprotein (LDL) >100 mg/dl (>2.29 mmol/l) [32]. Similarly, 72%–84% of pediatric kidney transplant recipients had LDL>100 mg/dl (>2.29 mmol/l) [32]. In ESRD, triglycerides are consistently elevated, with average triglyceride levels greater than 150 mg/dl, and HDL-cholesterol levels, generally thought to be protective against coronary artery disease are diminished. Lp(a), a lipoprotein associated with a mild increase in risk in the general population, is significantly elevated in ESRD, although the importance of this is unclear since it is genetically determined, and also levels are related to worsening renal function.
Two additional risk factors are much more common in ESRD than in the general population; these are homocysteine and CRP. Homocysteine has procoagulant activity and may cause direct injury to the endothelium. Homocysteine levels also increase with worsening renal function, as metabolism of homocysteine may require intrarenal metabolism [33]. Homocysteine is elevated in >65% of children with CKD [34]. Interestingly, the level only increases after 7 years of age, and this appears to be independent of renal function [34, 35]. The higher the homocysteine levels in children with CKD, the lower the vitamin B12 and folate levels. This suggests a role for careful assessment of nutritional deficiencies in the pediatric ESRD population [34, 35].
CRP is strongly associated with future cardiovascular events, although the magnitude of its association with risk prediction is under debate. The main reason for controversy is its strong association with conventional risk factors. Thus, it is unclear whether elevated levels represent vascular inflammation associated with a high-risk environment or are independent predictors in themselves. It is also unclear whether CRP may be most useful as a marker of acute vascular instability or a marker of ongoing chronic vascular damage. Cross-sectional measurements of CRP reveal elevated levels that are three times higher in pediatric ESRD patients on dialysis and two times higher in transplant recipients compared with healthy controls [20]. Furthermore, CRP is highly correlated with coronary calcium, especially in patients who also have an elevated PTH level. An elevated CRP level may reflect chronic inflammation from many sources, including overt or occult infectious processes, co-morbid conditions such as access complications, and factors associated with the dialysis procedure per se, including bioincompatible membrane and possibly dialysate leak in the membrane [36]. The high CRP levels in ESRD [37] are consistent with a milieu that promotes vascular injury.
Additional risk factors such as malnutrition, oxidative stress, proteinuria, anemia, infection, medications, and activation of the renin-angiotensin system have increased prevalence in CKD. In addition, in the dialysis population, calcium phosphorus metabolism with an elevated phosphorus has been associated with increased mortality [38, 39] and vascular calcification [19, 20]. In the adult CKD population, low-calcium dialysate and non-calcium-containing phosphate binders are advocated. The role of limiting calcium in growing children with ESRD needs to be addressed.
A significant difference between pediatric and adult ESRD is the frequency of diabetes mellitus as a primary etiology. Since diabetes mellitus is a major cause of ESRD in adults, the link between diabetes and long-term cardiovascular outcome in older individuals is self evident. Pediatric ESRD patients, however, may be at high risk for insulin resistance through several mechanisms: treatment with medications that worsen insulin sensitivity (e.g., steroids, growth hormone), sedentary life style, and obesity. Future studies are needed to address this question. With the current obesity epidemic, it is possible that early renal dysfunction may emerge as a significant co-morbidity in some individuals.
There is little information on the relationship between tobacco use and the presence of ESRD. In adult studies, tobacco use is well known to be associated with increased risk for mortality and cardiovascular complications.
Non-invasive assessment of cardiac end organ injury
A major technological advance in recent years is the ability to non-invasively assess the presence of cardiovascular target end organ injury in the absence of manifest cardiac disease [40]. Abnormalities have been detected in youth with extremes of traditional cardiovascular risk factors, such as hypercholesterolemia, hypertension, and obesity. These include LV hypertrophy, left atrial enlargement, presence of coronary arterial calcium, endothelial dysfunction assessed by measurement of brachial artery reactivity, and the presence of increased carotid arterial wall thickness. These markers of target organ injury have been associated with cardiovascular events in adults. The discussion above suggests that children with ESRD are at increased cardiovascular risk; studies of these non-invasive measures of end organ injury confirm this suspicion.
The most important and well-studied non-invasive diagnostic tool is echocardiography. Cardiovascular function and the presence of pericardial disease are routinely assessed and LV mass can be measured. LV hypertrophy is secondary to the chronic volume loading associated with anemia and uremia as well as hypertension. The LV mass index in the dialysis population is almost twice that of the healthy controls [23]. Frequent monitoring of the pediatric dialysis population is warranted, with a 40%–75% prevalence of LV hypertrophy despite treated hypertension [24, 25, 26, 27, 28]. LV hypertrophy, an LV mass >51 kg/m2.7, can be treated by maintaining higher levels of hemoglobin with the use of erythropoietin [41], and by effectively treating hypertension.
One of the most striking atherosclerotic precursors in ESRD is the presence of coronary calcium on coronary computed tomography (CT) by either helical or electron beam CT. There is increased coronary calcium in young adults with a history of pediatric ESRD [19, 20]. It is unknown whether this represents a dramatic acceleration of atherosclerosis in ESRD or an increased propensity for calcium to accumulate in the medial wall of the coronary vessel due to altered calcium metabolism in ESRD. Although coronary calcium develops in the 3rd decade in patients with ESRD, recent observations in young adults that risk factors assessed years before the measurement of non-invasive target organ injury are better predictors than contemporary risk factors. This suggests that the pediatric ESRD patient with many cardiovascular risk factors is highly likely to have coronary calcium as a young adult [42].
Endothelial dysfunction assessed by brachial artery reactivity has been demonstrated in CKD. These findings are independent of lipid levels and hypertension but are correlated with LV mass index [35, 43]. This technique remains a research tool.
Risk factor management
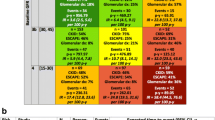
Current guidelines for cardiovascular risk factor management in ESRD are incomplete. The presence of malignant forms of myocardial adaptation to stress such as LV hypertrophy, cardiomyopathy, and/or atherosclerosis suggests the need for aggressive treatment (Table 1).
Treatment of hypertension is well established, and includes pharmacological therapy and control of intravascular fluid management. A blood pressure less than the 90th percentile for the child’s age, gender, and height, as recommended by the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents, is an appropriate goal (http://www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm). An unresolved question in children is the level for optimal blood pressure control; should the target be lowered to the 50th percentile for appropriate age, gender, and height (analogous to the adult goal of <120/80 mmHg)?
Regression of LV hypertrophy is possible in patients on dialysis [44]. Close monitoring of blood pressure and also yearly echocardiograms to monitor cardiac size are critical to prevent LV hypertrophy. Specific medications have been recommended for preserving severe LV dysfunction; these include angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β1-selective blockers such as carvedilol and metoprolol. Pediatric trials are underway to support these recommendations based mostly on clinical experience and adult data [45]. Other supportive measures include fluid management with diuretics and/or dialysis. Digoxin, formerly a mainstay of congestive heart failure treatment, has more limited use in contemporary management, and may not be necessary if regulation of therapeutic levels is complicated by renal failure.
The most recent guidelines for lipid management have been developed for adults (National Cholesterol Panel-Adult Treatment Panel III). These recommendations recognize the importance of aggressive lipid-lowering therapy in patients with documented coronary artery disease or the presence of coronary artery disease equivalents such as diabetes mellitus. Current pediatric guidelines do not address the issue of accelerated cardiovascular disease caused by diabetes or CKD [46]. A recent statement from the American Diabetes Association has attempted to update the 1992 Pediatric NCEP guidelines to reflect both increased awareness of accelerated cardiovascular disease in diabetes mellitus and new clinical experience with the HMG Co-A reductase inhibitors (statins) [47]. As all children with chronic kidney disease are at high risk, similar to children with diabetes, a recommended diagnostic and treatment algorithm would include screening and monitoring children with a fasting lipid profile. Fasting lipoprotein levels could be obtained yearly, and dietary modification initiated when appropriate in children with CKD. If children are prepubertal or less than 10 years of age, recommendations for treatment should follow the guidelines proposed by the expert panel in children [46]. Children >10 years of age or postpubertal could be considered for lipid-lowering therapy with a statin for LDL-cholesterol ≥160 mg/dl, a non-HDL-cholesterol of ≥190 mg/dl, or an LDL-cholesterol of ≥130 mg/dl if extreme risk is thought to be present. The current NKF K/DOQI guidelines on treatment of dyslipidemia should be used for children and adolescents with advanced CKD and ESRD [48, 49]. There are currently no specific treatments for elevations of Lp(a).
For other risk factors, treatment is less certain. In 25 children with CKD, a double-blind placebo-controlled randomized crossover trial of folic acid for 8 weeks showed statistically significant improvement in endothelial-dependent dilatation with lowering of homocysteine levels [50]. However, long-term effects of homocysteine lowering need to be studied to determine if improved endothelial function is sustained despite worsening kidney function. Lowering homocysteine has not yet been proven to improve cardiovascular survival in the general population. Currently, in the transplant population, a nationwide, multicenter clinical trial randomized controlled trial, The Folic Acid for Vascular Outcome Reduction in Transplantation (FAVORIT), is underway to determine whether total homocysteine-lowering treatment with a high-dose combination of folic acid, vitamin B12, and vitamin B6 reduces the rate of cardiovascular disease among 4,000 stable renal transplant recipients with mild to moderately elevated total homocysteine levels [51].
Tobacco use should be monitored, and smoking cessation programs initiated where necessary. It is probably useful to also monitor insulin resistance in high-risk individuals.
Summary
In CKD, the origins of cardiovascular mortality and morbidity are in childhood when the cardiovascular risk milieu is established. Natural history studies are underway to better document the presence of cardiovascular risk factors in CKD, and their association with cardiovascular subclinical disease. In the interim, clinicians need to consider reducing the risk of cardiovascular disease by modifying traditional cardiovascular risk factors, and monitoring for end organ injury through the use of echocardiography, and, in young adults, CT studies for coronary calcium. Chronic cardiovascular risk factor reduction, begun early in the course of CKD, is now an essential part of clinical management.
References
Parekh RS, Carroll CE, Wolfe RA, Port FK (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:191–197
Mitsnefes MM (2002) Pediatric end-stage renal disease: heart as a target. J Pediatr 141:162–164
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW (2003) Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108:2154–2169
Levin A, Thompson CR, Ethier J, Carlisle EJ, Tobe S, Mendelssohn D, Burgess E, Jindal K, Barrett B, Singer J, Djurdjev O (1999) Left ventricular mass index increase in early renal disease: impact of decline in hemoglobin. Am J Kidney Dis 34:125–134
Alpert MA, Ravenscraft MD (2003) Pericardial involvement in end-stage renal disease. Am J Med Sci 325:228–236
Scharer K, Schmidt KG, Soergel M (1999) Cardiac function and structure in patients with chronic renal failure. Pediatr Nephrol 13:951–965
Mitsnefes MM, Daniels SR, Schwartz SM, Khoury P, Strife CF (2001) Changes in left ventricular mass in children and adolescents during chronic dialysis. Pediatr Nephrol 16:318–323
Silverstein DM, Palmer J, Polinsky MS, Braas C, Conley SB, Baluarte HJ (2000) Risk factors for hyperlipidemia in long-term pediatric renal transplant recipients. Pediatr Nephrol 14:105–110
Kari JA, Vallance DT, Bruckdorfer KR, Leone A, Mullen MJ, Bunce T, Dorado B, Deanfield JE, Rees L (1997) Physiology and biochemistry of endothelial function in children with chronic renal failure. Kidney Int 52:468–472
Fine A (2002) Relevance of C-reactive protein levels in peritoneal dialysis patients. Kidney Int 61:615–620
Arici M, Walls J (2001) End-stage renal disease, atherosclerosis, and cardiovascular mortality: is C-reactive protein the missing link? Kidney Int 59:407–414
Querfeld U, Lang M, Friedrich JB, Kohl B, Fiehn W, Scharer K (1993) Lipoprotein(a) serum levels and apolipoprotein(a) phenotypes in children with chronic renal disease. Pediatr Res 34:772–776
Chavers BM, Li S, Collins AJ, Herzog CA (2002) Cardiovascular disease in pediatric chronic dialysis patients. Kidney Int 62:648–653
Ross R (1999) Atherosclerosis—an inflammatory disease. N Engl J Med 340:115–126
Nayir A, Bilge I, Kilicaslan I, Ander H, Emre S, Sirin A (2001) Arterial changes in paediatric haemodialysis patients undergoing renal transplantation. Nephrol Dial Transplant 16:2041–2047
London G (2003) Cardiovascular calcifications in uremic patients: clinical impact on cardiovascular function. J Am Soc Nephrol 14 [Suppl 4]:S305–S309
Milliner DS, Morgenstern BZ, Murphy M, Gonyea J, Sterioff S (1994) Lipid levels following renal transplantation in pediatric recipients. Transplant Proc 26:112–114
Litwin M, Grenda R, Prokurat S, Abuauba M, Latoszynska J, Jobs K, Boguszewska-Baczkowska A, Wawer ZT (2001) Patient survival and causes of death on hemodialysis and peritoneal dialysis—single-center study. Pediatr Nephrol 16:996–1001
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Moe SM, O’Neill KD, Duan D, Ahmed S, Chen NX, Leapman SB, Fineberg N, Kopecky K (2002) Medial artery calcification in ESRD patients is associated with deposition of bone matrix proteins. Kidney Int 61:638–647
Moe SM, Duan D, Doehle BP, O’Neill KD, Chen NX (2003) Uremia induces the osteoblast differentiation factor Cbfa1 in human blood vessels. Kidney Int 63:1003–1011
Mitsnefes MM, Kimball TR, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2003) Left ventricular mass and systolic performance in pediatric patients with chronic renal failure. Circulation 107:864–868
Mitsnefes MM, Daniels SR, Schwartz SM, Meyer RA, Khoury P, Strife CF (2000) Severe left ventricular hypertrophy in pediatric dialysis: prevalence and predictors. Pediatr Nephrol 14:898–902
Ulmer H (1978) Cardiovascular impairment and physical working capacity in children with chronic renal failure. Acta Paediatr Scand 67:43–48
Morris KP, Skinner JR, Wren C, Hunter S, Coulthard MG (1993) Cardiac abnormalities in end stage renal failure and anaemia. Arch Dis Child 68:637–643
Litwin M, Kawalec W, Latoszynska J, Grenda R, Smirska E (1994) Cardiac systolic and diastolic function in children on hemodialysis and continuous ambulatory peritoneal dialysis. Contrib Nephrol 106:114–118
Johnstone LM, Jones CL, Grigg LE, Wilkinson JL, Walker RG, Powell HR (1996) Left ventricular abnormalities in children, adolescents and young adults with renal disease. Kidney Int 50:998–1006
Mitsnefes M, Ho PL, McEnery PT (2003) Hypertension and progression of chronic renal insufficiency in children: A Report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). J Am Soc Nephrol 14:2618–2622
Neu AM, Ho PL, McDonald RA, Warady BA (2002) Chronic dialysis in children and adults. The 2001NAPRTCS Annual Report. Pediatr Nephrol 17:656–663
Parekh RS, Ni W, Fivush BA, Klag MJ (2001) Prevalence of traditional cardiovascular risk factors in the Dialysis Mortality and Morbidity Special Study (DMMS) among different age groups: a nationally representative sample of the US ESRD population. J Am Soc Nephrol 12:236A
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for managing dyslipidemias in chronic kidney disease. Am J Kidney Dis 41 [Suppl 3]:S1–S92
Bostom AG, Kronenberg F, Jacques PF, Kuen E, Ritz E, Konig P, Kraatz G, Lhotta K, Mann JF, Muller GA, Neyer U, Riegel W, Schwenger V, Riegler P, Selhub J (2001) Proteinuria and plasma total homocysteine levels in chronic renal disease patients with a normal range serum creatinine: critical impact of true glomerular filtration rate. Atherosclerosis 159:219–223
Merouani A, Lambert M, Delvin EE, Genest J Jr, Robitaille P, Rozen R (2001) Plasma homocysteine concentration in children with chronic renal failure. Pediatr Nephrol 16:805–811
Lilien M, Duran M, Van Hoeck K, Poll-The BT, Schroder C (1999) Hyperhomocyst(e)inaemia in children with chronic renal failure. Nephrol Dial Transplant 14:366–368
Stenvinkel P, Pecoits-Filho R, Lindholm B (2003) Coronary artery disease in end-stage renal disease: no longer a simple plumbing problem. J Am Soc Nephrol 14:1927–1939
Goldstein SL, Currier H, Watters L, Hempe JM, Sheth RD, Silverstein D (2003) Acute and chronic inflammation in pediatric patients receiving hemodialysis. J Pediatr 143:653–657
Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998) Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 31:607–617
Ganesh SK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK (2001) Association of elevated serum PO(4), Ca x PO(4) product, and parathyroid hormone with cardiac mortality risk in chronic hemodialysis patients. J Am Soc Nephrol 12:2131–2138
Gidding SS (2002) The aging of the cardiovascular system: when should children be treated like adults? J Pediatr 141:159–161
Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE (1996) The impact of anemia on cardiomyopathy, morbidity, and mortality in end-stage renal disease. Am J Kidney Dis 28:53–61
McGill HC Jr, McMahan CA (2003) Starting earlier to prevent heart disease. JAMA 290:2320–2322
Aggoun Y, Niaudet P, Laffont A, Sidi D, Kachaner J, Bonnet D (2000) Cardiovascular impact of end-stage renal insufficiency in children undergoing hemodialysis. Arch Mal Coeur Vaiss 93:1009–1013
Hampl H, Sternberg C, Berweck S, Lange D, Lorenz F, Pohle C, Riedel E, Gogoll L, Hennig L (2002) Regression of left ventricular hypertrophy in hemodialysis patients is possible. Clin Nephrol 58 [Suppl 1]:S73–S96
Shaddy RE, Tani LY, Gidding SS, Pahl E, Orsmond GS, Gilbert EM, Lemes V (1999) Beta-blocker treatment of dilated cardiomyopathy with congestive heart failure in children: a multi-institutional experience. J Heart Lung Transplant 18:269–274
National Cholesterol Education Program (1992) Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics 89:525–584
American Diabetes Association (2003) Management of dyslipidemia in children and adolescents with diabetes. Diabetes Care 26:2194–2197
Group KDOQIKD (2003), K/DOQI clinical practice guidelines for management of dyslipidemias in patients with kidney disease. Am J Kidney Dis 41 [Suppl 3]:S1–S91
Kasiske B, Cosio FG, Beto J, Bolton K, Chavers BM, Grimm R Jr, Levin A, Masri B, Parekh R, Wanner C, Wheeler DC, Wilson PW (2004) Clinical practice guidelines for managing dyslipidemias in kidney transplant patients: a report from the Managing Dyslipidemias in Chronic Kidney Disease Work Group of the National Kidney Foundation Kidney Disease Outcomes Quality Initiative. Am J Transplant 4 [Suppl 7]:13–53
Bennett-Richards K, Kattenhorn M, Donald A, Oakley G, Varghese Z, Rees L, Deanfield JE (2002) Does oral folic acid lower total homocysteine levels and improve endothelial function in children with chronic renal failure? Circulation 105:1810–1815
Bostom AG, Kronenberg F, Gohh RY, Schwenger V, Kuen E, Konig P, Kraatz G, Lhotta K, Mann JF, Muller GA, Neyer U, Riegel W, Riegler P, Ritz E, Selhub J (2001) Chronic renal transplantation: a model for the hyperhomocysteinemia of renal insufficiency. Atherosclerosis 156:227–230
Acknowledgements
Portions of this paper were presented at the Annual Dialysis Conference: 14th Annual Symposium on Pediatric Dialysis, Seattle, Washington, 3 March entitled “Cardiac disease in pediatric dialysis patients: the scope of the problem.” Supported in part by grants from the American Society of Nephrology Carl W. Gottschalk Research Scholar Grant and National Institute of Diabetes and Digestive and Kidney Diseases (K23 DK02872), National Institutes of Health. We would like to thank Dr. B.A. Fivush for her careful review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parekh, R.S., Gidding, S.S. Cardiovascular complications in pediatric end-stage renal disease. Pediatr Nephrol 20, 125–131 (2005). https://doi.org/10.1007/s00467-004-1664-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-004-1664-0