Abstract
This pilot study was designed to evaluate the efficacy and acceptability of sevelamer hydrochloride as a phosphate binder in pediatric patients treated with dialysis. A 6-month open-label trial of sevelamer hydrochloride (Renagel) was initiated in 17 patients, aged 11.8±3.7 years, undergoing hemodialysis (n=3) or peritoneal dialysis (n=14). Following a 2-week washout period of the phosphate binders, serum phosphorus increased from 5.2±1.3 mg/dl to 7.5±2.2 mg/dl (P<0.0002). After initiation of therapy with sevelamer hydrochloride, serum phosphorus levels decreased to 6.2±1.2 mg/dl (P<0.01) during the first 8 weeks and final values were 6.3±1.5 mg/dl. Serum calcium concentration decreased during the washout period from 9.4±0.9 mg/dl to 8.9±1.5 mg/dl (P<0.01); values remained unchanged thereafter. The serum calcium-phosphorus ion product decreased during the first 8 weeks and values did not change subsequently. Serum bicarbonate, parathyroid hormone, total cholesterol, low-density lipoprotein and high-density lipoprotein cholesterol, and triglyceride levels did not change. The initial prescribed dose of sevelamer hydrochloride was 121±50 mg/kg (4.5±5 g/day) and the final prescribed dose was 163±46 mg/kg (6.7±2.4 g/day). Sevelamer hydrochloride was well tolerated and without adverse effects related to the drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The control of hyperphosphatemia is a clinical challenge in the care of children with end-stage renal disease (ESRD) treated with dialysis. Moreover, phosphate retention and hyperphosphatemia play a pivotal role in the development of secondary hyperparathyroidism [1, 2]. In addition, hyperphosphatemia and hypercalcemia are major contributors to the pathogenesis of extraskeletal and vascular calcifications [3, 4, 5, 6, 7, 8].
The control of serum phosphorus levels is, therefore, essential in these patients and the available options include: (1) dietary phosphate restriction, but long-term compliance is difficult, as such diets are associated with protein restriction that may have important negative effects on the growing skeleton; (2) enhance phosphate removal by dialysis delivery, but with the current dialysis prescription, the removal rates are inadequate when compared with the daily net phosphorus absorption; and (3) block intestinal phosphate absorption with the use of phosphate-binding agents.
The most commonly used phosphate binders contain either aluminum or calcium. With the recognition that long-term ingestion of aluminum-containing phosphate-binding agents can result in aluminum retention and intoxication [9], the use of aluminum-free phosphate-binding agents has been recommended [10, 11, 12]. Indeed, calcium-based phosphate binders are currently widely used in children treated with dialysis. However, hypercalcemia and hyperphosphatemia occurred in 25%–50% of patients receiving large doses of calcium carbonate. Furthermore, the widespread use of calcium-containing phosphate binders may play a role in the development of the aplastic or adynamic lesion of renal osteodystrophy, as well as vascular calcifications [7, 13].
Sevelamer hydrochloride, derived from cholesterol-binding resins, is a non-aluminum, non-calcium-containing phosphate binder hydrogel of cross-linked poly (allylamine hydrochloride) that is resistant to digestive degradation and is not absorbed from the gastrointestinal tract. Its mechanism of action relates to the presence of partially protonated amines spaced one carbon from the polymer backbone, which interact with the phosphate ions by ionic and hydrogen binding. Several studies have demonstrated adequate control of serum phosphorus levels with sevelamer hydrochloride in adult patients treated with hemodialysis [14, 15, 16, 17, 18, 19]. This agent, however, has not been utilized in children. Thus, the current pilot study was designed to determine the efficacy and acceptability of sevelamer hydrochloride as a phosphate binder agent in pediatric patients treated with dialysis.
Materials and methods
All patients between the ages of 2 and 18 years undergoing maintenance dialysis at the UCLA/Davita Pediatric Dialysis Unit were considered as potential candidates for the study. In total, 17 patients were entered into the study: 9 males and 8 females. The mean age of all patients was 11.8±3.7 years; 7 patients were aged between 2 and 11 years and 10 patients were aged 12–18 years. Patients were treated with dialysis for 37.3±35.5 months at the outset of the study. Three patients were undergoing treatment with maintenance hemodialysis and 14 patients were receiving peritoneal dialysis. The ethnic distribution was as follows: Hispanic (65%); Caucasian 17%; and African-American 12%.
The patients entered into the study were receiving a stable dosage of calcium-containing phosphate binders 4.0±3.0 g/day with or without concurrent therapy with active vitamin D sterol for at least 3 months prior to the initiation of the study protocol. Patients younger than 2 years were excluded because they were considered unable to swallow the capsules of sevelamer hydrochloride. The dialysate calcium concentration was 1.5 mmol/l in 41% and 2.25 mmol/l in 59% of the patients.
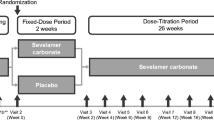
Prior to initiation of therapy with sevelamer hydrochloride, patients underwent a 2-week washout period without the use of phosphate-binding agents and were then entered into a 6-month open-label clinical trial. The tablets of sevelamer hydrochloride were supplied as odorless, tasteless, hard gelatin, single-strength capsules (403 mg). During the course of the study, 7 patients were switched to 800-mg tablets because they became available. The initial dose of sevelamer hydrochloride was two capsules with each meal because serum phosphorus levels were less than 7.5 mg/dl after the washout period [17]. The dose was increased by one tablet per meal (three times three tablets per day) every month as necessary to achieve serum phosphate levels below 6.5 mg/dl.
In total, 12 patients completed the study: 3 patients were withdrawn from the study because of documented non-compliance and persistent hyperphosphatemia, and 2 patients were withdrawn because of cadaveric kidney transplantation.
At monthly intervals starting from the end of the washout period, serum phosphorus, calcium, calcium-phosphorus ion product, parathyroid hormone (PTH), and total bicarbonate concentrations were measured. Total cholesterol, high-density lipoprotein (HDL) and triglyceride levels were determined at the end of the washout period and after 6 months. Baseline values before the washout period represent the average of single determinations in each of the patients. All blood samples were analyzed at the UCLA Clinical Laboratories using standard methods. Serum PTH levels were measured using an immunoradiometric assay (Nichols Institute, San Juan Capistrano, Calif., USA) that detects PTH (1–84) and has cross-reactivity with amino terminally truncated PTH fragments, probably 7–84 [20, 21]. The study was approved by the UCLA Human Subjects Protection Committee and informed consent form was obtained from all the patients and/or their parents.
Intent-to-treat analysis was utilized for the interpretation of the results. Descriptive statistics (mean, standard deviation, median) were used to summarize the laboratory data at each time point. Due to the small sample size, signed rank test was used to compare the change in biochemical determinations between two time points. A mixed-effect regression model with first-order splines was employed to characterize the change of the biochemical parameters during the study period. The values represent the estimated rates of change at different time intervals. The slope that significantly differs from zero indicates a change in the biochemical value during the time interval. Statistical software package, SAS, was used to carry out the analysis and a significance level of 0.05 was applied for all statistical tests.
Results
During the washout period, the mean serum phosphorus levels increased from 5.2±1.3 mg/dl to 7.5±2.2 mg/dl (P<0.0002). After initiation of therapy with sevelamer hydrochloride, serum phosphorus levels decreased to 6.2.±1.3 mg/dl during the first 8 weeks of the study (P<0.01) and values remained stable thereafter. Serum phosphorus concentrations were 6.3±1.5 mg/dl at the end of the period of observation (NS) (Fig. 1). The mean serum calcium concentration decreased during the washout period from 9.4±0.9 mg/dl to 8.9±1.5 mg/dl (P<0.01) 2 weeks after discontinuation of the calcium-containing phosphate-binding agents. Serum calcium levels did not change substantially during therapy with sevelamer hydrochloride. Furthermore, the mean serum calcium-phosphorus ion product rose from 50±17 mg2/dl2 to 66±21 mg2/dl2 (P<0.0001) during the washout period and decreased to 57±14 mg2/dl2 during the first 8 weeks (P<0.05). Values remained unchanged subsequently (Fig. 2).
Serum PTH levels during the washout period ranged from 451±60 pg/ml to 604±123 pg/dl (NS) and PTH concentrations remained within baseline values throughout the period of the study. Final values were 667±247 pg/ml (NS). Serum total bicarbonate levels were 25.9±3.4 mEq/l and 25.4±3.9 mEq/l at the beginning and end of the washout period. Values remained unchanged during the course of the study. The initial prescribed dose of sevelamer hydrochloride was 121±50 mg/kg (4.5±5 g/day) and the final prescribed dose was 163±46 mg/kg (6.7±2.4 g/day).
Baseline total serum cholesterol and triglyceride levels were 176±92 mg/dl and 274±329 mg/dl, respectively and values at the end of the study were 153±50 mg/dl and 272±218 mg/dl (NS). Initial and final mean serum HDL levels were 40.3±9.3 and 40.4±8.5 mg/dl, respectively (NS). Six patients were treated with calcitriol therapy (daily or intermittent) at a mean dose of 104±22 ng/kg per day during the course of the study. Therapy with intravenous calcitriol was discontinued in 2 patients because of persistent hyperphosphatemia, 2 patients continued to be given the same dose of calcitriol (0.5 μg/day), and the dosage of calcitriol was doubled from 1 μg/day to 2 μg/day in 2 patients during the course of the study.
Sevelamer hydrochloride was well tolerated and there were no adverse effects related to the study drug. Overall, the tablets were well accepted by the patients.
Discussion
The primary objective of this pilot study was to assess the efficacy and tolerance of sevelamer hydrochloride as a phosphate binder in pediatric patients treated with maintenance dialysis. Sevelamer hydrochloride has been found to effectively reduce serum phosphorus levels and values remained within target levels in the vast majority of patients during the 6 months of the study. However, serum calcium levels diminished during the first 2 weeks after discontinuation of the calcium-containing-phosphate binding agents, while values remained unchanged for the duration of the study. The serum calcium-phosphorus ion product diminished during therapy with sevelamer hydrochloride due mainly to the changes in serum phosphorus concentrations. Baseline serum PTH levels were consistent with a mild degree of secondary hyperparathyroidism and values did not change despite therapy with calcitriol. Serum bicarbonate levels, as well as serum cholesterol and low-density lipoprotein (LDL)-cholesterol, did not change during therapy with sevelamer hydrochloride. The initial prescribed dose of sevelamer hydrochloride was two/three tablets three times a day with meals. Initially, patients were given 403-mg tablets and, subsequently, when the 800-mg tablets became available, some patients were switched requiring fewer tablets per day.
Sevelamer hydrochloride has been shown to be an effective phosphate-binding agent in short and long-term studies in adult patients treated with maintenance hemodialysis [14, 15, 16, 17, 18, 19]. Goldberg et al. [15] demonstrated that the use of sevelamer hydrochloride led to reductions in serum phosphorus in hyperphosphatemic patients compared with an increase in placebo-treated patients over a period of 2 weeks. In a subsequent study, Chertow et al. [22] assessed the effect of sevelamer hydrochloride on serum phosphorus and the calcium-phosphorus ion product over 1 year in adult patients undergoing maintenance hemodialysis. The results demonstrated adequate control of serum phosphorus levels without changes in serum PTH levels, as documented in the current study. In addition, the pattern of serum lipids changed during therapy with sevelamer hydrochloride. The serum level of LDL-cholesterol decreased while HDL increased [14]. More recently, similar control of serum phosphorus levels was obtained when sevelamar hydrochloride and calcium-containing salts were compared in adult patients treated with hemodialysis [19]. Overall, the results of the current study in pediatric patients are consistent with those previous observations, except for the lack of change in the lipid pattern. Although there was a trend in the same direction, the smaller sample size and the shorter period of observation may explain the differences. Further studies are needed to assess the effects of therapy with sevelamer hydrochloride on lipid metabolism in children treated with dialysis.
Changes in serum bicarbonate levels have been described during therapy with sevelamer hydrochloride. In the initial studies by Chertow et al. [22], values were found to increase. However, bicarbonate levels were lower in those patients treated with sevelamer hydrochloride compared with calcium-containing binders [19]. Overall, serum bicarbonate levels did not change in the current study, as previously shown in adult patients undergoing hemodialysis [17]. It is interesting to note that serum calcium levels decreased by 0.5 mg/dl from initial values during the washout period after discontinuation of the calcium-containing phosphate-binding agents. Similar effects have been reported in previous studies and, thus, provide further evidence for the role of such agents in the development of an exogenous calcium load [15, 16, 17]. Such findings were further supported when the use of calcium-containing phosphate-binding agents was compared with aluminum hydroxide in pediatric patients treated with dialysis [23]. Serum calcium levels were higher and episodes of hypercalcemia occurred more often with the use of the calcium-containing phosphate-binding agents [23].
The reduction of the serum calcium-phosphorus ion product may prove to be an important factor in the prevention of long-term calcifications related to abnormalities of mineral metabolism in renal failure. Goodman et al. [7] demonstrated that the calcium-phosphorus ion product was higher in those patients with a positive coronary artery calcification score than in those with a negative score. Furthermore, when vascular calcifications were evaluated in autopsy material from 120 children with ESRD, Milliner et al. [3] demonstrated that soft tissue calcifications were present in 60% of the patients and systemic calcinosis in 36%. The major factors implicated were the use of active vitamin D sterols, the peak calcium-phosphorus ion product, the age at onset of renal failure, and gender (male) [3]. In addition, Block et al. [24] demonstrated that there was a steady increase in the relative risk of death with hyperphosphatemia and an elevated calcium-phosphorus ion product in a cross-sectional study of a large number of adult patients treated with dialysis. Thus, reduction of the serum calcium-phosphorus ion product that is observed during therapy with sevelamer hydrochloride might prove to be a very important factor in the prevention of long-term cardiovascular complications related to abnormalities of mineral metabolism in children with renal failure.
Over the last few years, it has been shown that the widespread use of calcium-containing phosphate binders may play a role in the development of vascular calcifications. Goodman et al. [7] demonstrated coronary artery calcification measured by electron beam computed tomography in young adult dialysis patients who developed ESRD in childhood. Moreover, the amount of calcium ingested daily from the calcium salts used as phosphate binders was nearly double in those patients with coronary artery calcification compared with those without calcification [7]. Using ultrasonography of the carotid artery, aorta, and femoral arteries, Guerin et al. [25] also demonstrated vascular calcifications in a large number of adult patients undergoing maintenance hemodialysis. The extent of arterial calcification increased with the use of calcium-containing phosphate binders. The mortality rate was higher in those patients with higher baseline vascular calcification scores [26]. Finally, calcium-containing phosphate-binding agents have been implicated in the pathogenesis of adynamic osteodystrophy, which is characterized by over-suppression of PTH levels and frequent episodes of hypercalcemia [13].
Hence, there is growing evidence that treatment with calcium and active vitamin D sterols may promote vascular calcification. Thus, the current therapeutic approach for the management of hyperphosphatemia with the use of calcium-containing phosphate binders should be reconsidered because patients are in a net positive calcium balance mainly due to the use of large doses of calcium-containing salts. The dialysate calcium concentration and therapy with active vitamin D sterols play an additional role in the development of a positive calcium flux [27]. It may be prudent, therefore, to modify the current large doses of calcium for the management of hyperphosphatemia. Indeed, it has been demonstrated by Chertow et al. [19] that coronary and aortic calcification scores diminished or did not change when adult patients undergoing hemodialysis were treated with sevelamer hydrochloride compared with those receiving calcium carbonate or acetate as the main phosphate-binding agents. Whether such an effect would affect morbidity and mortality in patients undergoing maintenance dialysis remains to be studied [19]. In addition, the effect of the current dialysis prescription on the control of serum phosphorus levels should be considered, because hyperphosphatemia is present in 60% of a large cohort of patients treated with hemodialysis [25]. It has been shown that a greater delivery of dialysis by daily nocturnal hemodialysis can prevent hyperphosphatemia without the use of phosphate-binding agents and some patients require phosphate supplementation [28, 29]. This technique has not yet been applied in pediatric patients with ESRD.
In summary, sevelamer hydrochloride, a non-absorbed aluminum- and calcium-free phosphate binder, effectively reduced serum phosphorus levels and the calcium-phosphorus ion product in children treated with maintenance dialysis. This new binder may play an important role in the prevention of soft tissue and vascular calcification in pediatric patients with ESRD. As overall survival rates in these patients have improved over the last 2 decades, it is important that major efforts are made to prevent the long-term consequences of vascular calcifications [30].
References
Almaden Y, Canalejo A, Hernandez A, Ballesteros E, Garcia-Navarro S, Torres A, Rodriguez M (1996) Direct effect of phosphorus on parathyroid hormone secretion from whole parathyroid glands in vitro. J Bone Miner Res 11:970–976
Slatopolsky E, Finch J, Denda M, Ritter C, Zhong M, Dusso A, MacDonald PN, Brown AJ (1996) Phosphorus restriction prevents parathyroid gland growth. High phosphorus directly stimulates PTH secretion in vitro. J Clin Invest 97:2534–2540
Milliner DS, Zinsmeister AR, Lieberman E, Landing B (1990) Soft tissue calcification in pediatric patients with end-stage renal disease. Kidney Int 38:931–936
Blacher J, Demuth K, Guerin AP, Safar ME, Moatti N, London GM (1998) Influence of biochemical alterations on arterial stiffness in patients with end-stage renal disease. Arterioscler Thromb Vasc Biol 18:535–541
Braun J, Oldendorf M, Moshage W, Heidler R, Zeitler E, Luft FC (1996) Electron beam computed tomography in the evaluation of cardiac calcifications in chronic dialysis patients. Am J Kidney Dis 27:394–401
Kimura K, Saika Y, Otani H, Fujii R, Mune M, Yukawa S (1999) Factors associated with calcification of the abdominal aorta in hemodialysis patients. Kidney Int [Suppl 71]:S238–S241
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Goodman WG (2001) Vascular calcification in chronic renal failure. Lancet 358:1115–1116
Coburn JW, Norris KC, Nebeker HG (1986) Osteomalacia and bone disease arising from aluminum. Semin Nephrol 6:68–89
Salusky IB, Coburn JW, Foley J, Nelson P, Fine RN (1986) Effects of oral calcium carbonate on control of serum phosphorus and changes in plasma aluminum levels after discontinuation of aluminum-containing gels in children receiving dialysis. J Pediatr 108:767–770
Slatopolsky E, Weerts C, Lopez-Hilker S, Norwood K, Zink M, Windus M, Delmez J (1986) Calcium carbonate is an effective phosphate binder in patients with chronic renal failure undergoing dialysis. N Engl J Med 315:157–161
Andreoli SP, Dunson JW, Bergstein JM (1987) Calcium carbonate is an effective phosphorus binder in children with chronic renal failure. Am J Kidney Dis 9:206–210
Salusky IB, Goodman WG (2001) Adynamic renal osteodystrophy: is there a problem? J Am Soc Nephrol 12:1978–1985
Chertow GM, Burke SK, Lazarus JM, Stenzel K, Wombolt D, Goldberg DI, Bonventre JV, Slatopolsky E (1997) Poly[allylamine hydrochloride] (RenaGel): a noncalcemic phosphate binder for the treatment of hyperphosphatemia in chronic renal failure. Am J Kidney Dis 29:66–71
Goldberg DI, Dillon MA, Slatopolsky EA, Garrett B, Gray JR, Marbury T, Weinberg M, Wombolt D, Burke SK (1998) Effect of RenaGel, a non-absorbed, calcium- and aluminum-free phosphate binder, on serum phosphorus, calcium, and intact parathyroid hormone in end-stage renal disease patients. Nephrol Dial Transplant 13:2303–2310
Wilkes BM, Reiner D, Kern M, Burke S (1998) Simultaneous lowering of serum phosphate and LDL-cholesterol by sevelamer hydrochloride (RenaGel) in dialysis patients. Clin Nephrol 50:381–386
Slatopolsky EA, Burke SK, Dillon MA (1999) RenaGel, a nonabsorbed calcium- and aluminum-free phosphate binder, lowers serum phosphorus and parathyroid hormone. The RenaGel Study Group. Kidney Int 55:299–307
Chertow GM, Dillon M, Burke SK, Steg M, Bleyer AJ, Garrett BN, Domoto DT, Wilkes BM, Wombolt DG, Slatopolsky EA (1999) A randomized trial of sevelamer hydrochloride (RenaGel) with and without supplemental calcium. Strategies for the control of hyperphosphatemia and hyperparathyroidism in hemodialysis patients. Clin Nephrol 51:18–26
Chertow GM, Burke SK, Raggi P (2002) Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int 62:245–252
John MR, Goodman WG, Gao P, Cantor TL, Salusky IB, Jüppner H (1999) A novel immunoradiometric assay detects full-length human PTH but not amino-terminally truncated fragments: implications for PTH measurements in renal failure. J Clin Endocrinol Metab 84:4287–4290
Gao P, Scheibel S, D’Amour P, John MR, Rao DS, Schmidt-Gayk H, Cantor TL (2001) Development of a novel immunoradiometric assay exclusively for biologically active whole parathyroid hormone 1–84: Implications for improvement of accurate assessment of parathyroid function. J Bone Miner Res 16:605–614
Chertow GM, Burke SK, Dillon MA, Slatopolsky E (1999) Long-term effects of sevelamer hydrochloride on the calcium x phosphate product and lipid profile of haemodialysis patients. Nephrol Dial Transplant 14:2709–2714
Salusky IB, Foley J, Nelson P, Goodman WG (1991) Aluminum accumulation during treatment with aluminum hydroxide and dialysis in children and young adults with chronic renal disease. N Engl J Med 324:527–531
Block GA, Hulbert-Shearon TE, Levin NW, Port FK (1998) Association of serum phosphorus and calcium x phosphorus product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis 31:607–617
Guerin AP, London GM, Marchais SJ, Metivier F (2000) Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant 15:1014–1021
Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM (2001) Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension 38:938–942
Kurz P, Monier-Faugere MC, Bognar B, Werner E, Roth P, Vlachojannis J, Malluche HH (1994) Evidence for abnormal calcium homeostasis in patients with adynamic bone disease. Kidney Int 46:855–861
Pierratos A, Ouwendyk M, Francoeur R, Vas S, Raj DSC, Eccestone A, Uldall PR (1998) Nocturnal hemodialysis: three-year experience. J Am Soc Nephrol 9:859–868
Mucsi I, Hercz G, Uldall R, Ouwendyk M, Francoeur R, Pierratos A (1998) Control of serum phosphorus without any phosphate binders in patients treated with nocturnal hemodialysis. Kidney Int 53:1399–1404
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Acknowledgements
This study was supported in part by USPHS grants DK-35423, by GeltTex Pharmaceuticals, and by funds from the Casey Lee Ball Foundation. The results of the study were presented in part at the 2001 American Society of Nephrology Meeting in San Francisco. Dr. Salusky is a consultant for Genzyme Pharmaceutical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mahdavi, H., Kuizon, B.D., Gales, B. et al. Sevelamer hydrochloride: an effective phosphate binder in dialyzed children. Pediatr Nephrol 18, 1260–1264 (2003). https://doi.org/10.1007/s00467-003-1298-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1298-7