Abstract
Background
Laparoscopic inguinal hernia repair is one of the procedures most commonly performed by paediatric surgeons. Current research on the learning curve for laparoscopic hernia repair in children is scarce. This study aims to evaluate the clinical outcome and learning curve of laparoscopic intra-corporeal inguinal hernia repair in children.
Methods
A retrospective single-centre analysis of all paediatric patients who underwent laparoscopic intra-corporeal inguinal hernia repair between 2010 and 2019 was performed. The clinical outcomes were analysed. The data on the achievement of the learning curve by surgical trainees were evaluated with the CUSUM technique, focusing on operative time.
Results
There were 719 patients with laparoscopic intra-corporeal inguinal hernia repair (comprising 1051 sides) performed during the study period. The overall ipsilateral recurrence rate was 1.8% without other complications detected. CUSUM analysis showed that there were 3 phases of training, for which the trainees underwent initial learning phase (Phase 1) for the first 7 cases. After mastering of the skills and extrapolating the skills to male patients with smaller body size (Phase 2), they then achieved performance comparable to that of the senior surgeons after 18 procedures (Phase 3).
Conclusions
18 procedures seem to be the number required to reach the learning curve plateau in terms of operative time by surgical trainees. The clinical outcomes show that laparoscopic intra-corporeal inguinal hernia repair is a safe and transferrable technique, even in the hands of trainees, with adequate supervision and careful case selection. It also provides skill acquisition for minimally invasive surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernias account for one of the most encountered inguinoscrotal pathologies in children, affecting 0.8–4.4% of the paediatric population [1, 2]. Repair of inguinal hernias is also the most commonly performed procedure by paediatric surgeons. In the years since it was first described, an open inguinal approach with high ligation and division of the hernia sac has remained the gold standard of inguinal hernia repair [3]. However, in this era of minimally invasive surgery, there has been a paradigm shift in the treatment of paediatric inguinal hernia to routine laparoscopic repair in many centres worldwide [4, 5]. Laparoscopic techniques can largely be categorised into intra-corporeal or extra-corporeal closure; both involve ligation of the patent processus vaginalis (PPV) with a purse-string non-absorbable suture [2]. The benefits of laparoscopic surgery include possible detection and repair of contralateral hernias in a single operative procedure, better cosmetic outcomes, less postoperative pain, recurrence and complication rates that are comparable to those of open surgery [6,7,8].
Although laparoscopic intra-corporeal closure of hernia rings is a simple and safe technique for experienced paediatric surgeons, residents have to surmount the learning curve related to intra-corporeal suturing before they can master this technique, even if they have experience in other types of laparoscopic surgery [6, 9, 10]. As known from many other laparoscopic procedures, such as appendicectomy and cholecystectomy, and as described in the literature, multiple procedures need to be done by residents before the technique can be performed safely and result in expert outcomes [11,12,13]. In general, learning curves reflect the stepwise improvement of outcomes (measured as the surgical process or patients’ outcomes) as the learner gains experience in the learning process and ultimately reaches an expert plateau [11, 14].
The use of learning curves in medical education, training and competency assessment has recently been gaining increasing research interest. To date, however, studies describing the learning curve of laparoscopic hernia repair in children are scarce in the literature. There have only been scattered reports on the learning curve of laparoscopic extra-corporeal closure and percutaneous internal ring suturing (PIRS) methods; little is known about the learning curve of laparoscopic intra-corporeal closure of hernia in children [9, 15,16,17]. The current study aimed to review the clinical outcomes and learning curve associated with laparoscopic intra-corporeal inguinal hernia repair in paediatric patients.
Materials and methods
Patients and study design
A total of 719 paediatric patients who underwent laparoscopic intra-corporeal repair of inguinal hernias in the period between January 2010 and December 2019 were included in the study. Medical records were reviewed with data retrieved from an electronic patient record (ePR) system for analysis. The data in our analysis included patient demographics, details of operation, operative outcomes and complications. In addition, the number of intra-corporeal repairs performed by surgical trainees and senior surgeons (specialist and trainer surgeons), with the respective operative times and recurrence rates, were noted to plot the learning curve.
Operative procedure
The operative technique that we used has been published previously [18] (Fig. 1). After induction of general endotracheal anaesthesia, a 5-mm reusable port was inserted through the umbilicus via the open method. A pneumoperitoneum pressure of 8–10 mmHg was created. The internal opening of the hernia was confirmed, and the opposite side was inspected. Two more 3-mm reusable ports were placed lateral to the rectus muscle under telescopic vision. A 4/0 or 3/0 monofilament, non-absorbable polypropylene suture (depending on the body size and surgeon’s preference) was introduced percutaneously into the peritoneal cavity at the groin. A purse-string suture was placed around the internal hernia opening and tied using intra-corporeal knotting. The ends of the stitches were then cut, and the needle was removed percutaneously. The procedure was repeated over the contralateral side if a contralateral patent deep ring was noted. After release of the pneumoperitoneum, the ports were removed. The wound was closed using skin strips, except for the umbilical wound, which was closed with absorbable stitches.
a A non-absorbable suture was introduced through the anterior abdominal wall for the placement of purse-string suture at deep ring. b Deep ring was encircled by placing the suture intra-corporeally. c Testicular vessels and vas were avoided during placement of suture. d Deep ring was closed after tying the suture
Trainees’ characteristics
During the study period, eight paediatric surgery trainees (surgeons 1–8) received clinical training for laparoscopic intra-corporeal hernia repair. They were all higher surgical trainees in paediatric surgery with at least 2 years of basic surgical training and clinical experience in surgery. Under the training program of The College of Surgeons of Hong Kong, all of them reached a minimal number of 100 major operations as part of their training requirement every half-yearly during the specialist training. They received structured teaching while assisting senior surgeons (specialists and/or trainers). They then began to assume the role of operating surgeon after being deemed capable under the assistance and supervision of trainer surgeons (who have more than 2 years of full-time service as specialist surgeons after obtaining fellowship in paediatric surgery, and accredited by The College of Surgeons of Hong Kong as eligible trainers). Trainees were supervised at their earlier stage of training until they were capable of performing the procedure independently.
Outcome measures
The overall outcome (recurrence, conversion, postoperative complications) of laparoscopic intra-corporeal repair of inguinal hernia of the institute was reviewed. The primary outcome of the study was to evaluate the learning curve of surgical trainees in terms of operation time and complications. The secondary outcome was to investigate the pattern of the learning curve and identify the factors influencing the learning curve. Operative times were examined as skin-to-skin time (defined as the time from skin incision to skin closure). Postoperative complications (including testicular atrophy, ascending testis, wound complications, and recurrence) were reviewed as documented in the patients’ medical records, clinical charts, and surgeons’ follow-up consultation notes.
The cumulative sum method and learning curve analysis
The cumulative sum (CUSUM) technique was originally a method of assessing technical proficiency in the industrial sector [19]. However, in the medical literature, it has recently gained popularity as a tool for evaluating technical performance in surgical practice. At the individual and local levels, it is a useful tool for personal audits. At the national level, it is also helpful for quantitative measure of technical proficiency for the purpose of credentialling [20]. CUSUM analysis enables investigators to visualise trends in the data through transformation of raw data into the running total of data deviation from the group mean [19]. A CUSUM chart plots the cumulative sums of the deviations of the sample values (e.g. mean operative time by surgical trainees) from a target value (e.g. expert level performance as the reference) and offers graphical representation of the trend in the outcomes of a series of consecutive procedures performed over time. Changes in performance can be detected quickly with the CUSUM chart. When the procedure is performed at an unacceptable level, the CUSUM curve slopes upwards and signifies the climbing of the learning curve. The curve will eventually be flattened, which signifies the reaching of the expert level—that is, the trainees’ mastering of the procedural skills.
In this study, we used the mean operative time (MOT) of consecutive repairs as an index of the proficiency of each surgical trainee. All the procedures performed by each trainee were ordered chronologically from the earliest to the latest date of surgery. The MOT of repairs was calculated by the average of the total operative time of the same chronological order by the trainees. For instance, the MOT of the nth case is calculated by the sum of all the operative time of the nth procedure divided by the total number of trainees:
The learning curves of an average trainee were plotted based on MOT against the number of consecutive repairs performed. The number of repairs performed by each trainee before the learning curve plateaued was evaluated and compared. A CUSUM chart was obtained with the use of R version 4.0.5 through the CUSUM analysis described previously in the literature [20]. The CUSUM of the first case was run using the difference between its operative time and the MOT of the entire series, the second case was calculated using the same method, and so on.
Statistical analysis
All data were statistically analysed and compared. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS; IBM, USA) version 26 and R version 4.0.5. Descriptive statistics were given as the number of units (n) and percentage (%). Data were expressed as mean and standard deviation (SD). Continuous variables were analysed using the Student’s t-test and analysis of variance (ANOVA) test as appropriate; ordinal variables were analysed using the Mann–Whitney U test, and categorical variables were analysed using the Chi-square test. A p value < 0.05 was considered statistically significant.
Results
Patients’ characteristics and overall outcomes
The patients’ characteristics and overall perioperative outcomes are listed in Table 1. From January 2010 to December 2019, 719 paediatric patients underwent laparoscopic intra-corporeal repair of inguinal hernia comprising 1051 sides of repair. The patients included 556 boys and 163 girls with a median age of 2 (0–16) years and median body weight of 11.5 (2.6–63.9) kg who received the procedure. Bilateral repair was performed in 332 patients (46%). Among the unilateral cases, right-side repair was performed in 212 patients (30%) and left-side repair was performed in 175 patients (24%). Incidental contralateral PPV was detected in 278 patients (38.6%); patients presenting with initial left-sided hernia were more likely to have incidental PPV. Among all the repairs, 233 patients who underwent repairs performed by the surgical trainees were included in the learning curve analysis. Most of the repairs (84.5%) were supervised by trainer surgeons. Regarding the remaining 485 cases, specialist surgeons performed repairs on 154 patients and trainer surgeons performed repairs on 332 cases.
The MOT was 41.9 ± 18.6 min with negligible blood loss. Regarding the repairs performed by senior surgeons (specialist and trainer surgeons), the MOT was 40.3 ± 12.4 min, whereas the MOT of repairs performed by trainees was 43.4 ± 15.2 min. The MOT of senior surgeons was set as a reference for subsequent CUSUM learning curve analysis. Senior surgeons performed repairs more quickly than trainees and male patients generally received longer operations than female patients did (42 ± 19 vs 39 ± 16 min), although the differences did not reach statistical significance (p = 0.26 and p = 0.07, respectively). Furthermore, patients with smaller body sizes had a significantly longer MOT (52.2 ± 34 min in < 5 kg vs 40.9 ± 16 min in ≥ 5 kg, p < 0.05). The overall recurrence rate was 1.8%. Most recurrence (70.6%) occurred within the first year, with a mean time to recurrence of 9.45 ± 11.5 months from the index operation. The recurrence rates of repairs performed by trainees, specialist surgeons and trainers were 2.4%, 0.9% and 1.84%, respectively, with no statistically significant difference from one another (p = 0.431) (Table 2). There were no significant complications, such as wound infection, testicular atrophy or ascending testis, reported during the study period. There were no conversions in this series. The mean follow-up period was 18 ± 22.4 months.
Learning curve
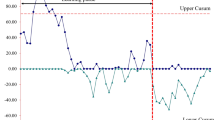
Figure 2 shows the average learning curve of the eight surgical trainees, plotted based on the MOT against the number of repairs performed. A shortening trend in the operative time with the accumulation of experience was observed based on this learning curve. For the sake of providing a measure of the quality of these repairs, a CUSUM analysis was conducted. Here, two cut-off points were identified at the 7th and 18th repairs, and thus three following phases were detected as expressing the learning curve: Phase 1, Case 1–7; Phase 2, Case 8–18; and Phase 3, Case 19–35 (Fig. 3). Patients’ characteristics and overall perioperative outcomes according to the phases of the learning curve are listed in Table 3. Trainees operated on a higher proportion of female patients in the initial phase than they did in subsequent phases, decreasing from 25 to 21% across the phases. In contrast, the body weight of patients operated on in the initial phase was heavier than it was in subsequent phases. The MOT significantly declined across the phases as experience accumulated, with statistically significant shorter operative durations in Phase 3 compared with Phase 1 (37.4 ± 5.7 vs 46 ± 9.2 min, p = 0.002). There was no recurrence in Phase 1, whereas the recurrence rate rose to 4% in Phase 2 and declined to 2% in Phase 3.
Discussion
With the advancement of laparoscopic surgeries in children, the standard of inguinal hernia repair in children has been shifting to a minimally invasive approach; this approach has been gaining popularity in many paediatric surgical centres worldwide [4, 5]. There are several types of procedures for laparoscopic inguinal surgery, including intra-corporeal and extra-corporeal closure, which both involve ligation of the PPV with a purse-string non-absorbable suture [2]. From our experience, laparoscopic intra-corporeal inguinal hernia repair is a safe procedure in children with no major complications detected during the study period. The recurrence rate was detected to be 1.8% in our study, which echoed the results of previously published data in the literature of 0.83–5.3% [21,22,23]. The recurrence rate of repairs performed by trainees was understandably higher than that of senior surgeons (specialist and trainer surgeon) because of learning curve issues and the need for accumulation of experience, yet not reaching statistical significance. Interestingly, trainer surgeons operated with a higher recurrence rate (1.84% vs 0.9%) than specialist surgeons did. This could be explained by the effect of case selection, with the more senior surgeons (trainers) operating on the more difficult patients with a smaller body size and with co-morbidities, leading to a higher recurrence rate (Table 2).
The MOT of laparoscopic intra-corporeal inguinal hernia repair for all levels of surgeons in our cohort was 41.9 ± 18.6 min. Indeed, a systematic review in 2021 by Maat et al. reported a longer duration of surgery in intra-corporeal repair compared with extra-corporeal repair, with the need for intra-corporeal suturing and knotting identified as the key time-limiting factor [24]. The intra-corporeal suturing and knotting approach places substantial demands on the requirement of hand–eye coordination, particularly in relation to the posterior and medial hemi-circumference of internal rings; major vessels, such as the iliac and inferior epigastric arteries; and the need to avoid important testicular vasculature—for example, the vas deferens and testicular vessels. With the accumulation of experience and various technical refinements, such as hydro-dissection and the “needle sign,” clinical outcomes improve and the operative time of the technique decreases [18].
Despite being proven to be safe, effective and non-inferior compared with traditional open repair, controversy still exists as to whether laparoscopic intra-corporeal inguinal hernia repair should be done by trainees with inadequate laparoscopic experience [8, 17]. Our results showed that laparoscopic intra-corporeal inguinal hernia repair is safe, feasible and reproducible; furthermore, it provides an adequate learning curve under the guidance of senior surgeons. It can be taught and performed by surgical trainees without jeopardising safety and outcomes. The role of the supervisor is crucial for careful case selection, skills demonstration and reducing the risk and morbidity related to the introduction and implementation of the new technique (intra-corporeal suturing and knotting) to the trainees. Intra-corporeal suturing and knotting play an important role in minimally invasive surgery in children. Many of the surgical procedures (e.g. fundoplication, pyeloplasty, ureteric reimplantation, intra-corporeal bowel anastomosis in hepatico-duodenostomy and duodeno-duodenostomy, etc.) in paediatric surgery involve reconstruction, but adjuncts (e.g. staplers) may not always be suitable for the tissue and they may not be feasible for children with tiny body cavities. Therefore, intra-corporeal suturing and knotting approaches are crucial in achieving the reconstructive goal in the limited working space. Thus, laparoscopic intra-corporeal inguinal hernia repair can serve as an entry procedure for paediatric surgical trainees to master these basic yet crucial skills, setting an important cornerstone in the development of laparoscopic skills before they can transfer this skill to more complex reconstructive procedures.
Despite the promising results related to laparoscopic surgery, it is well known that a learning curve exists in the introduction and learning of every procedure [20]. The learning curve for an operative procedure could be evaluated with the occurrence of operative complications, patient satisfaction and hospitalisation length; however, in the literature, it is generally evaluated according to the operative time [19, 20]. The CUSUM technique was originally a method of assessing technical proficiency in the industrial sector, as well as ensuring quality control. It has gained popularity recently in the medical literature as a tool for evaluating technical performance in surgical practice—for example, in robotic surgery, laparoscopic hepatectomy, and single-incision laparoscopic colectomy [25,26,27]. Previous landmark papers on surgical training and learning curves described 20 operations and 35 operations as necessary for a trainee to master laparoscopic appendectomy and laparoscopic cholecystectomy, respectively [12, 28]. At the same time, there have been previous reports on the learning curve of other hernia techniques in children. Yoshizawa et al. reported the need for more than 30 operations before residents can perform laparoscopic extra-corporeal inguinal hernia repair safely in children without supervision [9]. Furthermore, Shibuya et al. reported the need for 1 year of training comprising 125 operations before dexterous laparoscopic extra-corporeal inguinal hernia repair can be performed by trainees [17]. Moreover, Pogorelic et al. and Barroso et al. reported that 30–35 operations are necessary for the PIRS technique to be performed safely and effectively [15, 16]. They also concluded that a surgeon with an advanced level of previous experience in paediatric laparoscopic surgery will adopt the technique more easily, with a faster learning curve, compared with a surgeon lacking in such experience.
In this study, we identified two cut-off points—that is, three phases in the learning curve of laparoscopic intra-corporeal inguinal hernia repair. The procedure in Phase 1 (Cases 1–7) required a longer duration (46 ± 9.2 vs 37.4 ± 5.7 min, p = 0.002) compared with Phase 3 (Cases 19–35) but resulted in no recurrence. At the initial learning phase, more operative time may be spent on the vigilant placement of suture and knotting, leading to better outcomes. As evidenced by the higher proportion of female patients and the heavier body weight of patients operated on in the initial phase than in subsequent phases, careful case selection appeared to play an important role in minimising the risk of the procedure in the initial learning phase. However, recurrence subsequently rose to 4% in Phase 2 (Case 8–18) because of the loosening of case selection, while the skill had yet to mature in this phase. With further accumulation of experience, trainees finally achieved results comparable to an expert with reasonable operative times and recurrence rates without the need for supervision in Phase 3.
The current study helps elucidate the skill maturation of surgical trainees and allows formulation of a framework for training (Fig. 4). At the start of surgical skill training, close supervision by a dedicated proctor with careful case selection is necessary (e.g. cases involving patients with bigger body size, a higher proportion of female patients). The trainee can first become acquainted with basic skills (i.e. intra-corporeal suturing and knotting in our study) in relatively “easy” patients before they work on “more difficult” patients (e.g. patients with smaller sizes and male patients). The recurrence rate may initially increase after the initial phase; however, as experience accumulates, the trainee will eventually reach the expert level of operative duration and complication rate without the need for further supervision.
This study is limited by the small sample size of surgeons and patients operated on and could not reflect the learning curve for all paediatric laparoscopic surgeons starting laparoscopic intra-corporeal inguinal hernia with different skills and experience levels. However, to the best of our knowledge, this is the most comprehensive report on the learning curve and training recommendations for the technique in trainees. It sets a possible reference value for those who want to start this technique and commence training in laparoscopic surgery in children. The learning curve and trajectory of a trainee is potentially influenced by the overall case volumes accumulated by the trainee as well as their growth in operative skills through other case experiences. Albeit the actual experience levels of included trainees may vary, all of them reached a minimal number of 100 major operations as part of their training requirement every half-yearly. Besides, the heterogenicity in trainee characteristic may in turn reduce the selection bias among the subjects and improve the generalisability of the study. Future prospective clinical studies recruiting more surgeons and patients are necessary to delineate the learning curves of general trainees, as well as to identify significant factors influencing the learning curve. In addition, the impact on the learning curve of previous laparoscopic experience through observation as an assistant, being a surgeon in other procedures (e.g. appendectomy, varicocelectomy, etc.), as well as the impact of the contribution from different supervisors and assistants may be evaluated as well.
Operative time and operative outcome (e.g. recurrence rate) had been utilized by myriads of study on a multitude of procedures as a tool for assessing skill performance [15,16,17, 29]. However, criticism existed on their inadequacy in being the sole assessment modality for learning curve and technical progression of a surgical trainee [30]. Other parameters e.g. the degree of trainee autonomy or independency reached can enrich the assessment of learning curve. Furthermore, future work to include the use of objective assessment tool e.g. the Global Operative Assessment of Laparoscopic Skills (GOALS) which consists of a 5-item global rating scale would be beneficial to quantify trainees’ technical competency and learning trajectory.
In conclusion, surgical trainees acquired the skill to perform laparoscopic intra-corporeal inguinal hernia repair within 18 procedures. After this, the trainees could reach the learning curve plateau in terms of operative time, and the recurrence rate eventually declined with accumulation of experience. With appropriate supervision and careful case selections, laparoscopic intra-corporeal inguinal hernia repair can be a safe and transferrable technique, even in the hands of surgical trainees. It also provides skill acquisition for minimally invasive surgery. These results offer valuable information for the accreditation and planning of laparoscopic skills training for paediatric surgical trainees.
References
Chang SJ et al (2016) The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 20(4):559–563
Chan IH, Wong KK (2017) Common urological problems in children: inguinoscrotal pathologies. Hong Kong Med J 23(3):272–281
Levitt MA et al (2002) Variability of inguinal hernia surgical technique: a survey of North American pediatric surgeons. J Pediatr Surg 37(5):745–751
Laberge JM (2002) What’s new in pediatric surgery. J Am Coll Surg 195(2):208–218
Esposito C et al (2012) Unilateral inguinal hernia: laparoscopic or inguinal approach. Decision making strategy: a prospective study. Eur J Pediatr 171(6):989–991
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19(7):927–932
Toufique Ehsan M et al (2009) Laparoscopic hernioplasties in children: the implication on contralateral groin exploration for unilateral inguinal hernias. Pediatr Surg Int 25(9):759–762
Dreuning K et al (2019) Laparoscopic versus open pediatric inguinal hernia repair: state-of-the-art comparison and future perspectives from a meta-analysis. Surg Endosc 33(10):3177–3191
Yoshizawa J et al (2013) Laparoscopic percutaneous extraperitoneal closure for inguinal hernia: learning curve for attending surgeons and residents. Pediatr Surg Int 29(12):1281–1285
Shalaby R et al (2010) Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg 45(11):2210–2216
Valsamis EM et al (2018) Learning curves in surgery: variables, analysis and applications. Postgrad Med J 94(1115):525–530
Neugebauer E et al (1995) The E.A.E.S. Consensus development conferences on laparoscopic cholecystectomy, appendectomy, and hernia repair. Consensus statements–September 1994. The educational committee of the european association for endoscopic surgery. Surg Endosc 9(5):550–563
Mari G et al (1995) A postgraduate teaching course in laparoscopic surgery. Surg Endosc 9(10):1119–1122
Hopper AN, Jamison MH, Lewis WG (2007) Learning curves in surgical practice. Postgrad Med J 83(986):777–779
Pogorelić Z et al (2021) Learning curve for laparoscopic repair of pediatric inguinal hernia using percutaneous internal ring suturing. Children (Basel) 8(4):294
Barroso C et al (2017) Learning curves for laparoscopic repair of inguinal hernia and communicating hydrocele in children. Front Pediatr 5:207
Shibuya S et al (2019) The learning curve of laparoscopic percutaneous extraperitoneal closure (LPEC) for inguinal hernia: protocoled training in a single center for six pediatric surgical trainees. BMC Surg 19(1):6
Chan KL, Tam PK (2004) Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc 18(6):957–960
Kuge H et al (2020) Learning curve for laparoscopic transabdominal preperitoneal repair: a single-surgeon experience of consecutive 105 procedures. Asian J Endosc Surg 13(2):205–210
Lim TO et al (2002) Assessing doctors’ competence: application of CUSUM technique in monitoring doctors’ performance. Int J Qual Health Care 14(3):251–258
Lipskar AM et al (2010) Laparoscopic inguinal hernia inversion and ligation in female children: a review of 173 consecutive cases at a single institution. J Pediatr Surg 45(6):1370–1374
Pant N, Aggarwal SK, Ratan SK (2014) Laparoscopic repair of hernia in children: comparison between ligation and nonligation of sac. J Indian Assoc Pediatr Surg 19(2):76–79
Gause CD et al (2017) Laparoscopic versus open inguinal hernia repair in children ≤3: a randomized controlled trial. Pediatr Surg Int 33(3):367–376
Maat S et al (2021) Comparison of intra- and extra-corporeal laparoscopic hernia repair in children: a systematic review and pooled data-analysis. J Pediatr Surg 56(9):1647–1656
Nasseri Y et al (2021) Learning curve in robotic colorectal surgery. J Robot Surg 15(3):489–495
Nomi T et al (2015) Learning curve for laparoscopic major hepatectomy. Br J Surg 102(7):796–804
Haas EM et al (2013) Critical appraisal of learning curve for single incision laparoscopic right colectomy. Surg Endosc 27(12):4499–4503
Cagir B et al (1994) The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg 4(6):419–427
Wong KP et al (2016) Determining the learning curve of transcutaneous laryngeal ultrasound in vocal cord assessment by CUSUM analysis of eight surgical residents: when to abandon laryngoscopy. World J Surg 40(3):659–664
McCulloch RA et al (2021) Assessing the performance and learning curve of orthopaedic surgical trainees in primary total hip arthroplasty. Ann R Coll Surg Engl 103(7):514–519
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Adrian Chi Heng Fung, Ivy Hau Yee Chan, and Prof. Kenneth Kak Yuen Wong have no conflicts of interest or financial ties to disclose.
Ethical approval
The project does not include any interaction or intervention with human subjects or include any access to identifiable private information therefore no IRB approval was deemed necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fung, A.C.H., Chan, I.H.Y. & Wong, K.K.Y. Outcome and learning curve for laparoscopic intra-corporeal inguinal hernia repair in children. Surg Endosc 37, 434–442 (2023). https://doi.org/10.1007/s00464-022-09530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09530-1