Abstract
Background
Outcome data on robotic major hepatectomy are lacking. This study was undertaken to compare robotic vs. ‘open’ major hepatectomy utilizing patient propensity score matching (PSM).
Methods
With institutional review board approval, we prospectively followed 183 consecutive patients who underwent robotic or ‘open’ major hepatectomy, defined as removal of three or more Couinaud segments. 42 patients who underwent ‘open’ approach were matched with 42 patients who underwent robotic approach. The criteria for PSM were age, resection type, tumor size, tumor type, and BMI. Survival was individually stratified for hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (IHCC), and colorectal liver metastases (CLM). The data are presented as: median (mean ± SD).
Results
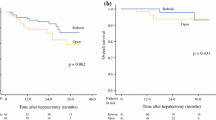
Operative duration for the robotic approach was 293 (302 ± 131.5) vs. 280 (300 ± 115.6) minutes for the ‘open’ approach (p = NS). Estimated Blood Loss (EBL) was 200 (239 ± 183.6) vs. 300 (491 ± 577.1) ml (p = 0.01). There were zero postoperative complications with a Clavien–Dindo classification ≥ III for the robotic approach and three for the ‘open’ approach (p = NS). ICU length of stay (LOS) was 1 (1 ± 0) vs. 2 (3 ± 2.0) days (p = 0.0001) and overall LOS was 4 (4 ± 3.3) vs. 6 (6 ± 2.7) days (p = 0.003). In terms of long-term oncological outcomes, overall survival was similar for patients with IHCC and CLM regardless of the approach. However, patients with HCC who underwent robotic resection lived significantly longer (p = 0.05).
Conclusion
Utilizing propensity score matched analysis, the robotic approach was associated with a lower EBL, shorter ICU LOS, and shorter overall LOS while maintaining similar operative duration and promoting survival in patients with HCC. We believe that the robotic approach is safe and efficacious and should be considered a preferred alternative approach for major hepatectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Complete surgical resection is the only chance for cure in the treatment of various hepatic neoplasms. The complexity of liver anatomy, including tumor proximity to intrahepatic biliovascular structures and hepatic parenchymal physiology, demands the highest operative performance to overcome the technical challenges associated with hepatic tumor resection. With the increased safety of open liver resection secondary to improvements in knowledge of liver anatomy, superior instrumentation, and improved perioperative critical care management, liver surgeons have embarked on newer techniques in the form of laparoscopic approaches in the last decade. Randomized trials have been published confirming the benefits of laparoscopic liver resection when compared to the traditional ‘open’ approach in terms of lower blood loss, quicker recovery, shorter length of hospital stay and decreased postoperative complications [1, 2].
Despite the benefits offered by laparoscopy in liver resection, delicate vessel dissection in the porta hepatis, bleeding control for hemostasis during parenchymal transection, bile duct suturing to manage bile leaks, and the potential need to create a hepaticojejunostomy anastomosis are difficult to achieve by many liver surgeons. As a result, ‘open’ conversion during laparoscopic liver resection has been reported to be as high as 35% by several institutions [3, 4]. A decade later, robotic liver resection has been introduced as a new and improved method to overcome the inherent limitations of straight instrumentation in laparoscopy; although missing tactile feedback, visual cues are improved via the three-dimensional camera, while wristed instrumentation provides a significant improvement to what can be achieved in a minimally invasive fashion in terms of suturing for anastomosis or rapid bleeding control.
The rise of minimally invasive techniques offers a chance to provide a superior perioperative course to these patients without compromising long-term oncological outcomes [4]. Despite the clear advantage of a robotic platform when compared to conventional laparoscopy, such as the wristed instrumentation and three-dimensional visualization, its adoption in North America for minimally invasive hepatobiliary operations has been slow and data on robotic liver operations are scarce. A few case series of robotic minor hepatectomy have been published but none of these are of major hepatectomy besides publications from our group of authors [5,6,7]. Justification of the incorporation of the robotic platform and education of the hepatobiliary community requires comparative data.
To this effect we sought to publish data from our tertiary hepatobiliary center by Propensity Score Matching (PSM) patients undergoing robotic and ‘open’ approaches to major hepatectomy. This is the largest North American single institution PSM study comparing robotic and ‘open’ major liver resection for the treatment of Hepatocellular Carcinoma (HCC), Intrahepatic Cholangiocarcinoma (IHC) and Colorectal Liver Metastases (CLM). The data and its analysis will add to the growing literature and assist surgeons in directing their patients to the best care in the treatment of these difficult diseases. Our hypothesis in undertaking this study is that patients undergoing robotic major hepatectomy for liver tumors have superior perioperative outcomes with no detriment to long-term oncological survival compared to those undergoing an ‘open’ approach.
Materials and methods
Data source and inclusion criteria
With institutional review board approval, we prospectively followed 183 consecutive patients who underwent robotic (n = 125) or ‘open’ (n = 58) major hepatectomy, defined as removal of three or more segments, for HCC, IHC or CLM between 2016 and 2021. This includes some patients operated via ‘open’ approach in 2016 before the initiation of our robotic liver program in 2017. After propensity score matching for age, resection type (as determined by major vs minor resection), tumor size, tumor type, and BMI, 42 patients undergoing robotic and 42 patients undergoing ‘open’ resection were matched. A small number of patients with miscellaneous tumors were included and classified in an “other” category. These included patients with an isolated single metastatic breast cancer lesion, an isolated metastatic ovarian cancer, an isolated metastatic renal cell carcinoma, symptomatic enlarging hemangioma and large adenomas > 5 cm without degeneration.
Patient variables
The following variables were studied: age, sex, BMI, operative duration, tumor size, resection margin distance, tumor type, Estimated Blood Loss (EBL), perioperative complications, Intensive Care Unit (ICU) length of stay, overall Length of Stay (LOS), readmission within 30 days and mortality up to 90-days. In addition, long-term overall survival (OS) was examined and Kaplan–Meier method was utilized for survival analysis.
Operative duration was defined as the time from the first incision to the placement of the final dressing. Intraoperative complications were defined as events necessitating major deviations from the planned procedure. Postoperative complications that significantly impacted the patients' clinical progress, as defined by a postoperative event that increased their LOS by more than one standard deviation above the mean, were compiled together as a single outcome variable. The Clavien–Dindo Classification (CDC) system was used to grade the severity of postoperative complications.
Operative technique
The following has been described in other publications, but has been reproduced for the sake of familiarity [8, 9]. Starting from 2017, we began to utilize the Intuitive Surgical Inc. da Vinci® Robotic Platform (Intuitive Surgical, Sunnyvale, CA, USA) to undertake minimally invasive hepatobiliary resections. Due to our satisfactory results in undertaking robotic liver surgery, we utilize this approach as the standard of care unless a major contradiction exists, which for our technical purposes is the need for major vascular resection and reconstruction. The following is our institutional approach to robotic liver surgery.
Patients are positioned supine on the operating table, induced with general endotracheal anesthesia. We routinely place a central venous catheter for CVP monitoring during major hepatectomy. An 8 mm trocar is inserted through the umbilicus for the robotic camera. Two 8 mm robotic ports are utilized at the right and left midclavicular lines in parallel. The latter is often upsized to a 12mm trocar if robotic stapling is required. A fourth 8 mm robotic port is placed along the left anterior axillary line at the level of the umbilicus. Finally, an Advanced Access Gelport® (Applied Medical, Rancho Santa Margarita, CA, USA), placed between the right midclavicular line and the umbilicus, is used for bedside suctioning and specimen extraction. An AirSeal® (ConMed, Utica, NY, USA) port is inserted through the Gelport for insufflation and smoke evacuation (Fig. 1).
Reverse Trendelenburg (15°) with a slight left tilt (5°) position is applied. The da Vinci Xi® robotic surgical system is docked over the patient's right shoulder and paired with the operating table to allow for intraoperative bed motion. The bedside assistant stands to the right of the patient, opposite from the scrub nurse (Fig. 2).
The operation begins with liver inspection and division of the falciform ligament all the way up to the hepatocaval confluence. Cephalad retraction of the liver to expose the porta hepatis is performed by non-grasping robotic bowel grasper. A thorough search for peritoneal carcinomatosis is undertaken and any concerning peritoneal lesions are biopsied for an intraoperative frozen section examination. Potential occult intrahepatic metastasis is ruled out by intraoperative ultrasonography. Identified lesions determined resectable are marked. Inflow vascular control to the ipsilateral hemiliver is obtained by individual dissection and ligation of the corresponding hepatic artery and portal vein. Once inflow control is obtained, the first 2 cm of superficial parenchymal transection is undertaken using monopolar scissor cautery. An extended vessel sealer and bipolar energy forceps are then used for deeper liver parenchymal transection following a modified crush-clamp technique, taking care to note of any significant portal or hepatic venous branches.
In our so-called modified crush-clamp technique, we use the robotic fenestrated forceps to crush the liver tissue, using limited laparoscopic irrigation to wash away the crushed tissue, while cautiously applying bipolar energy to obtain hemostasis on either side of the transection planes. This way, we can spare larger biliovascular structures from inadvertent partial transection, preventing nuisance bleeding. In contrast, the classical crush-clamp technique of parenchymal transection, described in many liver surgery textbooks, uses Kelly clamps during an open liver resection while applying the Pringle maneuver. Bipolar energy device is not applied for tissue hemostasis at the end of the tissue crushing. Additionally, we apply clips to medium sized biliovascular structures to prevent postoperative bile leaks or unnecessary intraoperative bleeding. Smaller biliovascular structures can be safely taken with the vessel sealer. A low CVP (<5mmHg) is strictly followed during the liver parenchymal splitting to reduce blood loss. Our technique has been well refined and we do not feel the need to routinely use the Pringle maneuver as a consequence, even in major hemihepatectomies. Finally, the bile duct pedicle and hepatic vein are transected using robotic 45 mm stapler. In operations for IHCC, the operating surgeon performs lymphadenectomy for both open and robotic resections as a standard procedure for IHCC.
Frozen section examination is performed for all resected specimens to confirm R0 resection margins. Once the specimens are detached, they are placed in an extraction bag and removed via the Gelport® incision. The surgeon accompanies the specimen to the Pathologist and a concordant measurement of the resection margin is conducted.
Statistical analysis
Data were maintained on an Excel (Microsoft Corporation Redmond, WA) spreadsheet and analyzed using GraphPad InStat version (3.0) (GraphPad Software La Jolla, CA). Statistical tests performed where appropriate were: F-test, Mann–Whitney U test, Student’s T-test, and Fisher’s exact test. Kaplan Meier curve estimated overall survival (OS). Significance was accepted with 95% probability. For illustrative purposes, data were presented as: median(mean ± standard deviation).
Results
183 patients were included and followed prior to PSM; 125 patients in the robotic cohort and 58 in the ‘open’ cohort. Prior to PSM, the tumor size was significantly greater in the ‘open’ cohort (7[8 ± 5.5] vs 5[5 ± 3.7] cm, p = 0.0003), while BMI was significantly lower in the ‘open’ cohort (26[26 ± 5.15] vs 28[28 ± 5.93] kg m−2, p = 0.03). The ‘open’ cohort had a statistically significantly greater EBL (300[471 ± 544.8] vs 200[253 ± 253.9] ml, p = 0.005), postoperative complications (15 vs 8 p = 0.0012), LOS (6 vs 4 days, p = 0.01) and 90-day mortality (7 vs 1 deaths, p = 0.0015) (Table 1).
After PSM, there were no differences between the ‘open’ and robotic cohorts in terms of age, sex, BMI, operative duration nor tumor size. The R0 and R1 resection rates were 93% and 7% for patients in the open cohort and 85% and 15% for patients in the robotic cohort respectively (p = 0.43). The ‘open’ cohort had significantly greater EBL (300[491 ± 577.1] vs 200[239 ± 183.6] ml, p = 0.01), ICU LOS (2[3 ± 2.0] vs 1[1 ± 0] days, p = 0.0001) and overall LOS (6[6 ± 2.7] vs 4[4 ± 3.3] days p = 0.003) compared to the robotic cohort. There were no statistically significant differences between the two cohorts in terms of readmission within 30 days, 90-day mortality nor postoperative complications (Table 2).
Patients undergoing resection for IHC and CLM had no statistically significant differences in terms of estimated median OS between the robotic and ‘open’ cohorts (Figs. 3 and 4). Patients undergoing robotic resection for HCC had a significantly improved estimated median OS vs patients undergoing ‘open’ approach (p < 0.05) (Fig. 5). When analyzed further, irrespective of tumor type, the robotic cohort had a statistically significantly superior estimated median OS over the ‘open’ cohort (38 vs 26 months, p < 0.05) (Fig. 6).
Discussion
This is the largest single center PSM study comparing robotic against ‘open’ major hepatectomy in North America. It demonstrates a less bloody operation, shorter length of ICU stay, and faster time to discharge. These superior perioperative outcomes support undertaking robotic major hepatectomy for patients with malignant liver tumors, confirming our hypothesis. With regards to long-term oncological outcomes, the robotic approach leads to at least similar overall survival for patients with liver cancers, with a particularly superior overall survival for patients with HCC. The data from this study are crucial in educating the hepatobiliary and oncology community at large regarding the role of the robotic platform in effecting non-inferior postoperative outcomes, and adequate long-term oncological outcomes for patients with these malignant diseases.
While prospective double blind randomized clinical trials are the gold standard in generating data, randomization in liver surgery, specifically for this study, is extremely difficult due to the rarity of both the disease and the surgical skill sets required to undertake complex hepatobiliary operations via the robotic approach. Even though not entirely perfect, PSM can control some confounders that puts retrospective studies at risk of bias. While resection via an ‘open’ technique can be undertaken for more complex liver tumors requiring major vascular resection and reconstruction, a propensity matching that includes tumor size as well as type of resection may reduce confounding factors affecting operative complexity. Along this line, the performance of a lymphadenectomy for cases of IHCC added complexity and time for operative completion, but as our propensity matching included tumor type, this did not make a difference between the two approaches in term of the outcomes of this study.
The results of the first randomized controlled trial (OSLO-COMET Trial) comparing laparoscopic and open minor hepatectomy were published by Fretland et al. in 2018 [10]. The authors demonstrated a significant reduction in LOS and postoperative complications in patients undergoing laparoscopic hepatectomy. However, their study only included patients with CLM. Neither did their trial exclusively study those undergoing major hepatectomy; even so, their study is considered the landmark paper in minimally invasive liver surgery. In terms of economical aspects, at four months, the costs of both approaches equalized. While the majority of their findings can be extrapolated to robotic hepatectomy, their cost analysis cannot; this is because of the complex and often times unclear financial implications in purchasing and maintaining a robotic platform. Finally, there was no OS analysis reported by the authors beyond 90 days. Our paper contributes more clinical data beyond COMET as it includes other cell types besides CLM—such as HCC and IHCC, which often demand more challenging wider or anatomical resections due to their insidious peritumoral vascular and parenchymal invasion. Furthermore, we also analyzed the long-term OS to prove the non-inferiority of the robotic approach in the treatment of malignant liver tumors, as questioned by many liver surgeons.
Our study demonstrated a survival benefit of the robotic approach over the ‘open’ approach, particularly in the resection of HCC, even though we did not expect this finding at the start of the study. This was not the case for other cell types in the subgroup analyses (IHCC and CLM). While the reason for this is not entirely clear at this time, understanding the carcinogenesis of these neoplasms may explain these findings. Inflammatory changes are associated with both the carcinogenesis and recurrence of HCC [11,12,13]. Since minimally invasive approaches are associated with a significantly reduced perioperative inflammatory burden that attenuates an expeditious recovery [14, 15], it is possible that this inflammatory attenuation reduces the risk of HCC recurrence, a key determinant to survival after HCC resection [16]. The perioperative period plays an important role in the much later oncological outcome of patients. For example, perioperative blood transfusions through immunosuppression worsens long-term oncologic survival [17]. Perioperative increases in inflammation via the ‘open’ approach over the robotic approach may therefore play a critical factor in the observed difference in OS. The intimate relationship of cirrhosis and chronic liver inflammation with HCC [18], which exists to a lesser extent in IHCC and even less so with CLM, may also explain why the survival benefit was most pronounced in the subgroup analysis of patients with HCC and with neither IHCC nor CLM. Molecular data demonstrating reductions in inflammatory mediators of local and metastatic recurrence after gastric cancer resection via a minimally invasive approach have been published by Yu et al. [19]. Similar reductions in inflammatory mediators of HCC recurrence after a robotic approach in comparison to an ‘open’ approach likely contributed to the observed difference in OS favoring the robotic approach.
Data from other institutions exist, but single institution datasets from North America are extremely limited. Nota et al. published a four institution American PSM study that only had 31 patients in the laparoscopic and ‘open’ cohorts respectively [20]. They demonstrated a similarly shorter length of stay in patients undergoing laparoscopic resection. Bagante et al. in a multi-institutional collaborative effort published a PSM study, which consist of 3000 patients, demonstrating fewer postoperative complications and a shorter LOS in when a minimally invasive approach was undertaken [21]; their data were drawn from NSQIP. Tee et al. published a different study from NSQIP data with a focus on elderly patients. The authors demonstrated a reduction in postoperative complications and length of stay via the minimally invasive approach to hepatectomy [22].
Although nationwide and multi-institution administrative databases have great utility, their heterogeneity in data collection and surgeon skill can affect their findings, unlike the single institution data we have presented, which eliminates biases in surgical skill. In this series, all operations were performed primarily by the same one liver surgeon (IS) with an assistant attending surgeon (SR or AR), therefore variation in operating surgeon skills is eliminated. It should be noted that some of the patients in the robotic cohort were operated at the beginning of the robotic liver surgeon’s learning curve. Thus, the beneficial effect of the robotic platform may not be fully realized due to the effect of this learning curve.
Collectively, there seems to be a consensus based on NSQIP and other data on the benefits of a minimally invasive approach to hepatectomy, including via the robotic platform, by reducing postoperative complications and length of stay. These findings are concordant with the findings of this study.
To conclude, this current study is the first to report postoperative and long-term OS benefits in patients undergoing robotic major hepatectomy using propensity score analysis and posits a plausible mechanism accounting for this unique finding based on the known links between inflammation and hepatocellular carcinogenesis. In patients where a minimally invasive approach is feasible and technical expertise is available, major hepatectomy should be undertaken in this fashion, particularly in the treatment of hepatocellular carcinoma where attenuation of perioperative inflammation may play a role in overall survival. In our institution, the robotic approach is the preferred technique and this method should be included in the armamentarium of modern liver surgeons.
References
Aghayan DL, Kazaryan AM, Dagenborg VJ, Røsok BI, Fagerland MW, Waaler Bjørnelv GM, Kristiansen R, Flatmark K et al (2021) Long-term oncologic outcomes after laparoscopic versus open resection for colorectal liver metastases : a randomized trial. Ann Intern Med 174:175–182. https://doi.org/10.7326/M20-4011
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, Hausken J, Tønnessen TI et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267:199–207. https://doi.org/10.1097/SLA.0000000000002353
Kwon Y, Cho JY, Han H-S, Yoon Y-S, Lee HW, Lee JS, Lee B, Kim M (2021) Improved outcomes of laparoscopic liver resection for hepatocellular carcinoma located in posterosuperior segments of the liver. World J Surg 45:1178–1185. https://doi.org/10.1007/s00268-020-05912-5
Goh BKP (2020) Letter regarding ‘benchmark performance of laparoscopic left lateral sectionectomy and right hepatectomy in expert centers.’ J Hepatol 73:1576. https://doi.org/10.1016/j.jhep.2020.07.002
Stewart C, Wong P, Warner S, Raoof M, Singh G, Fong Y, Melstrom L (2021) Robotic minor hepatectomy: optimizing outcomes and cost of care. HPB (Oxford) 23:700–706. https://doi.org/10.1016/j.hpb.2020.09.005
Sucandy I, Luberice K, Lippert T, Castro M, Krill E, Ross S, Rosemurgy A (2020) Robotic major hepatectomy: an institutional experience and clinical outcomes. Ann Surg Oncol 27:4970–4979. https://doi.org/10.1245/s10434-020-08845-4
Sucandy I, Luberice K, Rivera-Espineira G, Krill E, Castro M, Bourdeau T, Ross S, Rosemurgy A (2021) Robotic major hepatectomy: influence of age on clinical outcomes. Am Surg 87:114–119. https://doi.org/10.1177/0003134820945249
Sucandy I, Durrani H, Ross S, Rosemurgy A (2019) Technical approach of robotic total right hepatic lobectomy: how we do it? J Robot Surg 13:193–199. https://doi.org/10.1007/s11701-018-0881-7
Sucandy I, Gravetz A, Ross S, Rosemurgy A (2019) Technique of robotic left hepatectomy: how we approach it. J Robot Surg 13:201–207. https://doi.org/10.1007/s11701-018-0890-6
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, Hausken J, Tønnessen TI, Abildgaard A, Barkhatov L, Yaqub S, Røsok BI, Bjørnbeth BA, Andersen MH, Flatmark K, Aas E, Edwin B (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267:199–207. https://doi.org/10.1097/SLA.0000000000002353
Cariani E, Pilli M, Zerbini A, Rota C, Olivani A, Pelosi G, Schianchi C, Soliani P, Campanini N, Silini EM, Trenti T, Ferrari C, Missale G (2012) Immunological and molecular correlates of disease recurrence after liver resection for hepatocellular carcinoma. PLoS ONE 7:e32493. https://doi.org/10.1371/journal.pone.0032493
Refolo MG, Messa C, Guerra V, Carr BI, D’Alessandro R (2020) Inflammatory mechanisms of HCC development. Cancers (Basel). https://doi.org/10.3390/cancers12030641
Yeh C-C, Lin J-T, Jeng L-B, Ho HJ, Yang H-R, Wu M-S, Kuo KN, Wu C-Y (2015) Nonsteroidal anti-inflammatory drugs are associated with reduced risk of early hepatocellular carcinoma recurrence after curative liver resection: a nationwide cohort study. Ann Surg 261:521–526. https://doi.org/10.1097/SLA.0000000000000746
Shu Z-B, Cao H-P, Li Y-C, Sun L-B (2015) Influences of laparoscopic-assisted gastrectomy and open gastrectomy on serum interleukin-6 levels in patients with gastric cancer among Asian populations: a systematic review. BMC Gastroenterol 15:52. https://doi.org/10.1186/s12876-015-0276-4
Zhang H, Tong J-J, Zhang Z-N, Wang H-B, Zhang Y-H (2021) Laparoscopic left hemihepatectomy combined with right lateral hepatic lobectomy in pigs: surgical approach and comparative study of the inflammatory response versus open surgery. Vet Res Forum 12:1–6
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S (2015) Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg 261:947–955. https://doi.org/10.1097/SLA.0000000000000710
Boshier PR, Ziff C, Adam ME, Fehervari M, Markar SR, Hanna GB (2018) Effect of perioperative blood transfusion on the long-term survival of patients undergoing esophagectomy for esophageal cancer: a systematic review and meta-analysis. Dis Esophagus. https://doi.org/10.1093/dote/dox134
Qian S, Golubnitschaja O, Zhan X (2019) Chronic inflammation: key player and biomarker-set to predict and prevent cancer development and progression based on individualized patient profiles. EPMA J 10:365–381. https://doi.org/10.1007/s13167-019-00194-x
Yu G, Tang B, Yu P-W, Peng Z-H, Qian F, Sun G (2010) Systemic and peritoneal inflammatory response after laparoscopic-assisted gastrectomy and the effect of inflammatory cytokines on adhesion of gastric cancer cells to peritoneal mesothelial cells. Surg Endosc 24:2860–2870. https://doi.org/10.1007/s00464-010-1067-1
Nota CL, Woo Y, Raoof M, Boerner T, Molenaar IQ, Choi GH, Kingham TP, Latorre K, Borel Rinkes IHM, Hagendoorn J, Fong Y (2019) Robotic versus open minor liver resections of the posterosuperior segments: a multinational, propensity score-matched study. Ann Surg Oncol 26:583–590. https://doi.org/10.1245/s10434-018-6928-1
Bagante F, Spolverato G, Strasberg SM, Gani F, Thompson V, Hall BL, Bentrem DJ, Pitt HA, Pawlik TM (2016) Minimally invasive vs. open hepatectomy: a comparative analysis of the national surgical quality improvement program database. J Gastrointest Surg 20:1608–1617. https://doi.org/10.1007/s11605-016-3202-3
Tee MC, Chen L, Peightal D, Franko J, Kim PT, Brahmbhatt RD, Raman S, Scudamore CH, Chung SW, Segedi M (2020) Minimally invasive hepatectomy is associated with decreased morbidity and resource utilization in the elderly. Surg Endosc 34:5030–5040. https://doi.org/10.1007/s00464-019-07298-5
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Iswanto Sucandy, Emanuel Shapera, Cameron C. Syblis, Kaitlyn Crespo, Valerie A. Przetocki: Nothing to disclose. Sharona B. Ross: Reports personal fees and non-financial support from Intuitive Surgical Incorporated, outside the submitted work. Alexander S. Rosemurgy: Reports personal fees and non-financial support from Intuitive Surgical Incorporated, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sucandy, I., Shapera, E., Syblis, C.C. et al. Propensity score matched comparison of robotic and open major hepatectomy for malignant liver tumors. Surg Endosc 36, 6724–6732 (2022). https://doi.org/10.1007/s00464-021-08948-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08948-3