Abstract
Aim
To evaluate the efficacy and safety of brachytherapy with double-strand 125I seeds and biliary drainage for malignant obstructive jaundice.
Methods and Materials
42 patients with obstructive jaundice because of extrahepatic cholangiocarcinoma were enrolled. 22 patients (group A) received a biliary stent with common drainage tube implantation, and 20 patients (group B) received a biliary stent with double-strand 125I seeds radiotherapy drainage tube placement. The length, location and pathological stage of biliary stricture were recorded in the two groups. Total bilirubin (TBIL), direct bilirubin (DBIL), IgA, IgG, IgM, alanine aminotransferase and white blood cell (WBC) count were measured before and after percutaneous transhepatic cholangial drainage (PTCD). Tumor diameter was measured before and three months after PTCD, and the difference were calculated. Stent patency time, survival time, and complications were recorded.
Results
There was no significant difference in the length, location and pathological stage of biliary stenosis between the two groups. There was no significant difference in TBIL, DBIL, IgA, IgG, IgM, alanine aminotransferase and WBC count between the two groups before or after PTCD (P > 0.05). Three months after PTCD, tumors growth in group A and tumors shrinkage in group B. The difference in tumor size between the two groups before and after PTCD was statistically significant (P < 0.05). The average stent patency times in groups A and B were 3.55 ± 0.76 months and 8.76 ± 1.85 months, respectively (P < 0.05). The average survival times in groups A and B were 133.5 ± 27.8 days and 252.5 ± 114.5 days, respectively (P < 0.05). There was no statistically significant difference in the incidence of complications between the two groups (P > 0.05).
Conclusion
Double-strand 125I seeds radiotherapy biliary drainage tubes can safely and effectively control tumors, prolong the patency of biliary stents, and prolong patient survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Malignant obstructive jaundice is a common obstructive disease of the biliary tract. The causes of malignant obstructive jaundice include cholangiocarcinoma, gallbladder cancer, pancreatic cancer, and metastatic lymph nodes in the abdominal cavity [1]. Patients lack characteristic clinical manifestations in the early stages; thus, malignant obstructive jaundice is not easy to diagnose. Most patients are diagnosed in the middle and late stages and miss the opportunity to undergo surgical removal of primary lesions. The success rate of primary lesion resection is < 20%, the five-year survival rate is < 30%, and the relapse rate is high [2]. Biliary stents have become the preferred palliative treatment for malignant obstructive jaundice. Although stents can relieve obstruction, they do not treat the tumor. Most patients presented with jaundice four to six months after biliary stent implantation. The main reason is tumor progression and growth into the stent [3]. In this prospective study, self-made double-strand 125I seeds radiotherapy drainage tube combined with biliary stent was used to treat malignant obstructive jaundice. It is expected that the purpose of treating tumors can be achieved through low-dose continuous irradiation. The report is as follows..
Materials and methods
General information
This is a single-center, single-blind, randomized study designed to compare the effects of simple biliary stent and double-strand 125I seeds radiotherapy drainage tube combined with biliary stent. Inclusion criteria: (1) age between 18 and 85 years; (2) diagnosed as a malignant tumor of the extrahepatic bile duct, leading to obstructive jaundice; (3) unable to undergo surgical resection or the patient refused surgery; (4) willing Participate in this research and promise to abide by the research process. Exclusion criteria: (1) Patients with biliary obstruction unable to get through; (2) Patients with biliary fistula; (3) Patients after surgery; (4) Patients with massive ascites or multiple intrahepatic metastases; (5) Patients receiving other follow-up treatments (6) Those who refuse to sign informed consent or cannot adhere to the research process.
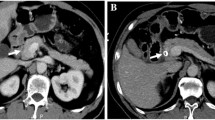
Forty-two patients with malignant obstructive jaundice who were admitted to our center from October 2016 to October 2018 were enrolled. All patients had clinical jaundice, bilirubinuria, anorexia, and bloating, and were admitted for total bilirubin (TBIL) and direct bilirubin (DBIL) elevation. Abdominal computed tomography and magnetic resonance imaging showed common bile duct obstruction and intrahepatic bile duct dilatation, which were diagnosed as extrahepatic bile duct obstruction (Fig. 1), and none of them received surgical intervention. All patients were diagnosed with extrahepatic cholangiocarcinoma by percutaneous biliary clamp biopsy. The study was approved by the medical ethics committee of the unit (ethics review number: 2018-KY-29). Patients and their family members were informed in detail about the surgical method, and patients provided informed consent.
Trial grouping
42 patients were immediately divided into two groups according to the treatment they received by computer system. There were 22 patients in group A (male, n = 13; female, n = 9) aged 44–83 years with a median age of 65 years. A Nitinol alloy stent with common biliary drainage tube placement was performed. There were 20 patients in group B (male, n = 12; female, n = 8) aged 42–85 years with a median age of 63 years. A Nitinol alloy stent with a self-made double-strand 125I seeds radiotherapy drainage tube placement was placed. All patients no longer receive other treatments.
Preoperative examination
Preoperative examination included routine bloods, blood biochemistry, blood coagulation, infectious disease screening (hepatitis B, hepatitis C, syphilis, and acquired immunodeficiency syndrome), tumor markers (carcinoembryonic antigen, cancer antigen 125, and cancer antigen 199), electrocardiogram, abdominal enhanced computed tomography or magnetic resonance imaging.
Surgical procedure
The main surgical instruments and medicines used were a percutaneous biliary puncture kit, a 5-F KMP catheter (Cook Medical, USA), an 8.5-F internal and external biliary drainage tube, a hydrophilic membrane guide wire (0.035 inch, 180 cm), a hydrophilic membrane, a hard guide wire (0.035 inch, 260 cm), an 8-F vascular sheath (Merit Medical System Inc., USA), biopsy forceps, and a nickel–titanium alloy biliary stent and associated delivery system (Nanjing Microinvasive Medical Technology Co., Ltd., China). 125I seeds (0.7 mCi; Tianjin Side Biopharmaceutical Co., Ltd., China), ioversol (Hengrui Pharmaceutical Co., Ltd., China), and a self-made double-chain radiotherapy biliary drainage tube (Henan Tuoren Medical Device Co., Ltd., China) were also used.
Interventional procedure
Lidocaine at a concentration of 0.02 g/mL was administered for local anesthesia and a puncture needle was used to puncture the tertiary branch of the right bile duct. Cholangiography (Fig. 2a) showed dilation of the intrahepatic and extrahepatic bile ducts and common bile duct stenosis or atresia. A guide wire was inserted through the sheath tube, and the sheath tube was withdrawn and advanced into the catheter along the guide wire. The catheter and guide wire were passed into the duodenum through the biliary stenosis or atresia, and pullback cholangiography was performed to show the length and location of the biliary stenosis or atresia. The harded guide wire was exchanged for. The 8-F sheath under the guidance of the guide wire and passed it into the biopsy forceps through the sheath (Fig. 2b). A lesion biopsy was performed and sent for pathological examination [4]. After receiving the pathological results, the biliary stent was sent along the hardened guide wire. The stent was accurately positioned and released (Fig. 2c). Group A received 8.5-F internal and external drainage tubes. In group B, a double-stranded radiotherapy drainage tube was placed, and 125I seeds were fed through the seed channels on both sides so that the two ends exceeded the lesion by 2 cm, and the biliary drainage tube was fixed (Fig. 2d). Postoperative single-photon emission computed tomography was performed to observe the seed irradiation range [5] (Fig. 3).
Postoperative treatment
Patients were instructed to consume liquidized food after PTCD. Patients were administered anti-inflammatory, hepatoprotective drugs, and supportive treatment. The patient's vital signs, abdominal symptoms, and liver and kidney function were observed.
Observation indicators and follow up
Drainage tubes of both groups were removed one month after PTCD. TBIL and DBIL were observed, and the difference between preoperative and postoperative values was calculated. The IgA, IgG, IgM, alanine aminotransferase and white blood cell count of patients before and one month after PTCD was calculated. Abdominal computed tomography and magnetic resonance imaging were performed before and three months after PTCD to measure the radial length of the tumor as follows: (maximum diameter + minimum diameter)/2 = tumor diameter. The difference before and after PTCD was calculated. Monthly follow up at the outpatient clinic and telephone follow up every three months of PTCD were performed and stent patency time was recorded. Patients’ survival times were recorded. According to reports in the literature, the median survival time of patients with malignant obstructive jaundice is 106–255 days, so the death of the patient and 2 years after the first patient was enrolled in this study were used as the study endpoint.
Statistical processing
SPSS 21.0 was used for statistical analysis. Measurement data are expressed as mean ± standard deviation (χ ± s), and a t-test was used to compare between groups. Count data are expressed as a percentage, and the χ2 test was used to compare between groups. A P value of < 0.05 was considered statistically significant.
Results
Comparison of general information between the two groups
Age, gender composition, preoperative TBIL and DBIL, alanine aminotransferase, white blood cell count, the length and location of biliary stenosis and tumor diameter were compared between the two groups before PTCD. No statistically significant differences were observed (Table 1).
In order for the prognosis of the two groups of patients to have a comparative meaning, this study adopted anatomical staging. Group A includes 1 case in stage IIIA (1/22, 4.5%), 18 cases in stage IIIB (18/22, 81.2%), 3 cases in stage IVA (3/22, 13.6%); group B includes 1 case in stage IIIA (1/20,5%), 17 cases of stage IIIB (17/20, 85%), and 2 cases of stage IVA (2/20, 10%).
Surgical situation
Forty-two patients underwent successful metal stent and drainage tube placement, and the success rate of a single operation was 100%. During operation, all patients had good stent positioning. The stents could expand, and the biliary tract recovered smoothly. There were no complications, such as massive biliary bleeding or pancreatitis, during or after operation. No 125I seeds were lost.
Changes in bilirubin, white blood cell count, and tumor diameter
TBIL, DBIL, and white blood cell count before and one month after PTCD were not statistically significant (P > 0.05; Table 2). Relief from jaundice was similar between the two groups, and seed implantation did not cause changes in white blood cell count. There was no statistically significant difference in IgA, IgG, and IgM before and after PTCD in group B (Table 3). In group A, the diameter of the tumor increased three months after PTCD compared with that before PTCD. In group B, the diameter of the tumor decreased compared with the tumor diameter before PTCD. The difference between the two groups was statistically significant, indicating that radiotherapy drainage tube placement effectively controlled tumor progression.
Comparison of stent patency time and survival
The average stent patency time in group A was 3.55 ± 0.76 months, while the average stent patency time in group B was 8.76 ± 1.85 months (P < 0.05). The average survival time of patients in group A was 133.5 ± 27.8 days, while the average survival time of patients in group B was 252.5 ± 114.5 days (P < 0.05; Table 4).
The dose of tumor tissue exposure
Both ends of the particle chain are 2 cm beyond the lesion, and the cumulative dose reaches 125 Gy at a distance of 0.5 cm from the seed chain, while the cumulative dose reaches 86 Gy at a distance of 1 cm from the seed chain calculated by the computerized treatment plan system (TPS).
Complications
Six patients (27.2%) in group A had minor complications, including three cases (13.6%) of minor biliary bleeding (< 10 mL), two cases (9.1%) of fever, and one case (4.5%) of abdominal pain, which improved after treatment. In group B, five patients (25.0%) had minor complications, including two cases (10%) of minor biliary bleeding, one case (5%) of fever, and two cases (10%) of abdominal pain. Vital signs in the two groups were stable after PTCD, and no fatal surgical complications occurred.
Discussion
Malignant obstructive jaundice is caused by invasion or compression of various malignant tumors or metastatic lymph nodes, resulting in biliary narrowing or atresia. At present, there are a lack of effective treatments in the clinic [1]. Surgery can remove the original lesion, but patients with malignant obstructive jaundice have no characteristic manifestations in the early stages. At the time of diagnosis, most patients with jaundice lose the chance to undergo radical surgery and can only undergo palliative treatment. The survival rate is within 30% [6, 7].
Percutaneous transhepatic cholangiography and drainage tube placement can quickly relieve jaundice. This approach is the preferred palliative treatment method, but biliary obstruction is not relieved and extubation is difficult. Biliary stents can effectively relieve biliary obstruction, making it possible for patients to remove the biliary drainage tube, but the stent has no therapeutic effect on the tumor. Continuous tumor growth may cause the tumor to penetrate the stent mesh and enter the stent, causing biliary tract restenosis. In addition, proliferation of the biliary intima after stent implantation also leads to an increased chance of biliary tract restenosis [8].
Studies have shown that low-dose, continuous radiation can effectively control tumors with low complication rates. Hasimu et al. [9] placed the strip of 125I seeds into the biliary stent. The biliary stent can effectively open the biliary obstruction, and the seed strip can radiate for a long time to exert an anti-tumor effect, reducing the chance of stent restenosis with a single row of seeds. The radiation dose was low, and the cumulative dose at a distance of 0.5 cm from the seed strip was approximately 85 Gy, while the cumulative dose at a distance of 1 cm from the seed strip was < 50 Gy. A large amount of fibrous connective tissue in the biliary tract tumor presents great resistance to penetration by radiation. Thus, higher doses are needed to effectively control the tumor. Moreover, the position of the seed strips is often biased to one side of the biliary tract, resulting in different radiation doses for the lesions on both sides of the biliary tract, and tumor control is poor. The biliary seed stent [10] consists of two parts. The outside is a self-expanding stent that can carry 125I seeds (the outer layer has a seed sheath), and the inside is a self-expanding metal support. During operation, a stent with seeds is placed first, and then a self-expanding metal stent is placed, which can effectively relieve biliary obstruction. The radiation released by seed decay can control tumor progression, but the cumulative dose of radiation outside the stent is still low. When the tumor is large, it is difficult for the radiation to cover the entire tumor, and the seeds cannot be removed after being placed. Once radiotherapy complications occur, radiotherapy cannot be terminated in time.
In this study, all patients obtained pathological results by forceps biopsy, which provided the pathological basis for subsequent treatment. The self-made double-chain 125I seeds brachytherapy biliary drainage tube was used to prepare two seed delivery channels outside the biliary drainage tube. Two rows of seeds can be loaded at the same time to form a double seed chain. The length of the seed chain depends on the extent of biliary disease. It is determined that the two ends of the seed chain generally exceed the lesion by 2 cm, and the cumulative dose reaches 125 Gy at a distance of 0.5 cm from the seed chain, while the cumulative dose reaches 86 Gy at a distance of 1 cm from the seed chain. The radiation dose to tumor tissue far exceeds that of single-stranded particle strips [11]. Combined with biliary stent placement, this approach can quickly and effectively relieve biliary obstruction. The dual seed chain can release radiation for a long period of time and a full dose can kill tumor cells. The results of this study show that compared with biliary stent placement combined with common drainage, biliary stent placement combined with double-chain radiotherapy can also play a role in reducing jaundice, prolonging stent patency time (8.76 ± 1.85 vs 3.55 ± 0.76 months), significantly shrinking the tumor after three months (0.89 ± 0.27 vs − 1.19 ± 0.42 cm). In terms of tumor control, the effect is equivalent to the biliary seeds stent [10]. The survival time was greatly extended (252.5 ± 114.5 vs 133.5 ± 27.8 days). The effect is better than simple biliary stent and biliary drainage tube [2]. The immune function was unaffected (IgA, IgG, and IgM in patients undergoing particle chain implantation have no significant changes compared with before operation). There were no serious complications related to PTCD, and the double-strand radiotherapy drainage tube permits termination of brachytherapy at any time.
Biliary stent combined with a double-strand 125I seeds brachytherapy drainage tube can quickly relieve malignant biliary obstruction and effectively control tumor progression, prolong the patency of biliary stents, and prolong patients survival. This approach is convenient and flexible with a low complication rate; thus, it is worthy of further attention in future studies.
This study has the following shortcomings. First, the sample size is small, and there are deficiencies in the assessment of tumor control rate, stent patency time, and patient survival, which need to be followed up with large samples and long-term follow-up studies; second; When calculating the radiation dose of the tumor, the drainage tube itself does not consider the obstruction of the radiation; third, the tumor tissue is compressed after the stent is placed, and there is a deviation in the measurement of the tumor size.
References
Naffaa M, Abu-Saleh N, Awad H, Khamaysi I, Karram T, Azzam ZS et al (2013) Acute obstructive jaundice and chronic cirrhosis protect against the adverse renal effects of pneumoperitoneum: role of nitric oxide. Surg Endosc 27(7):2517–2525
Sha J, Dong Y, Niu H (2019) A prospective study of risk factors for in-hospital mortality in patients with malignant obstructive jaundice undergoing percutaneous biliary drainage. Medicine (Baltimore) 98:e15131
Goutorbe F, Rouquette O, Mulliez A, Scanzi J, Goutte M, Dapoigny M et al (2017) Temporary placement of a covered duodenal stent can avoid riskier anterograde biliary drainage when ERCP for obstructive jaundice fails due to duodenal invasion. Surg Endosc 31(2):625–631
Chen WM, Wei KL, Chen YS, Chang PJ, Tung SH, Chang TS et al (2016) Transpapillary biliary biopsy for malignant biliary strictures: comparison between cholangiocarcinoma and pancreatic cancer. World J Surg Oncol 14:140
Ma J, Luo J, Gu J, Liu Q, Liu L, Zhang W et al (2018) Malignant obstructive jaundice treated with intraluminal placement of Iodine-125 seed strands and metal stents: An analysis of long-term outcomes and prognostic features. Brachytherapy 17(4):689–695
Chandrashekhara SH, Gamanagatti S (2016) Anuradha Singh, Sushma Bhatnagar: current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: a review. Indian J Palliat Care. 22(4):378–387
Morris S, Gurusamy KS, Davidson BR (2015) Cost-effectiveness of preoperative biliary drainage for obstructive jaundice in pancreatic and periampullary cancer. J Surg Res 193(1):202–209
Kwon CI, Ko KH, Hahm KB, Kang DH (2013) Functional self-expandable metal stents in biliary obstruction. Clin Endosc 46(5):515–521
Hasimu A, Gu JP, Ji WZ, Zhang HX, Zhu DW, Ren WX (2017) Comparative study of percutaneous transhepatic biliary stent placement with or without iodine-125 seeds for treating patients with malignant biliary obstruction. J Vasc Interv Radiol 28(4):583–593
Park S, Park JY, Bang S, Park SW, Chung JB, Song SY (2013) Radiotherapy prolongs biliary metal stent patency in malignant pancreatobiliary obstructions. Gut Liver 7(4):480–485
Liu Y, Lu Z, Zou DW, Jin ZD, Liu F, Li SD (2009) Intraluminal implantation of radioactive stents for treatment of primary carcinomas of the peripancreatic-head region: a pilot study. Gastrointest Endosc 69(6):1067–1073
Acknowledgements
Thanks go to TuoRen Medical Group for its assistance in manufacturing a biliary drainage tube for use in this study.
Funding
Science and Technology project od Henan Province, Grant/Award Numbers: SB201902005 and SB201902014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Zong-Ming Li, De-Chao Jiao, Xin-Wei Han, Qin-Yu Lei, Xue-Liang Zhou and Miao Xu have no conflicts of interest or financial ties to disclose.
Ethical approval
We obtained permission from the Ethics Committee of the First Affiliated Hospital of Zhengzhou University.
Informed consent
Written informed consent was obtained from patients for publication of this article and any accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, ZM., Jiao, DC., Han, XW. et al. Preliminary application of brachytherapy with double-strand 125I seeds and biliary drainage for malignant obstructive jaundice. Surg Endosc 36, 4932–4938 (2022). https://doi.org/10.1007/s00464-021-08848-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08848-6