Abstract
Background
Long-term outcomes of single-incision laparoscopic colectomy (SILC) for colon cancer (CC), as practiced in real-world settings, especially in relation to disease stage, have not been established. We examined, retrospectively, both short- and long-term outcomes of SILC versus those of multiport laparoscopic colectomy (MPLC) performed for CC in a propensity-score-matched cohort.
Methods
The study involved 263 patient pairs matched 1:1 from among 691 patients who, between January 2008 and May 2014, underwent either SILC or MPLC for a primary solitary CC at our hospital. Short-term and long-term operative outcomes were compared between the two groups.
Results
Operation time was the only surgical outcome that varied significantly between the two groups (p = 0.0004). Overall 5-year cancer-specific survival (CSS) in the SILC group was 93.7 (95% CI 89.6–96.2)%, and CSS per pathological stage (I, II and III) was 98.5 (90.0–99.8)%, 96.0 (88.2–98.7)%, and 88.3 (79.6–93.6)%, respectively, whereas overall 5-year CSS in the MPLC group was 93.3 (89.4–95.9)%, and CSS per pathological stage was 100%, 95.4 (88.3–98.3)%, and 84.1 (74.1–90.8)% (p = 0.5278, 0.2679, 0.7666, and 0.9073), respectively. Overall 3-year disease-free survival (DFS) in the SILC group was 94.0 (90.2–96.4)%, and 3-year DFS per pathological stage was 98.6 (90.4–99.8)%, 90.1 (81.4–95.0)%, and 79.0 (69.4–86.2)%, respectively, whereas overall 3-year DFS in the MPLC group was 93.2 (89.4–95.7)%, and 3-year DFS per pathological disease stage was 100%, 94.5 (87.4–97.7)% and 75.5 (64.7–83.8)% (p = 0.2829, 0.7401, 0.4335 and 0.8518), respectively. Thus, oncological outcomes did not differ significantly between groups. Incisional hernia occurred in 21 (8.0%) SILC group patients and 17 (6.5%) MPLC group patients, without a significant between-group difference (p = 0.6139).
Conclusion
Our data indicate that perioperative and oncological outcomes of SILC performed for CC are comparable to those of MPLC performed for CC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic surgery has been used for 30 years to treat patients with colorectal cancer (CRC), and its use has increased as clinical trials have provided evidence of a clinical benefit [1,2,3,4,5,6]. Single-incision laparoscopic surgery (SILS), a minimally invasive procedure that is performed through a single small umbilical incision, has gained increased attention as a feasible alternative to conventional multiport laparoscopic surgery (MPLS) [7,8,9]. Systematic reviews and randomized controlled trials have shown that single-incision laparoscopic colectomy (SILC) is as safe, feasible, and effective as multiport laparoscopic colectomy (MPLC) for treatment of CRC [10,11,12,13,14,15,16,17], and SILC reportedly yields more favorable cosmetic outcomes and less postoperative pain than multiport laparoscopic colectomy [15, 18], but long-term (5-year) outcomes [19, 20], outcomes of patients of relatively poor American Society of Anesthesiologists (ASA) physical status (PS), and outcomes related to the various pathological stages have not been clarified. Our Osaka Police Hospital is a high-volume multidisciplinary acute care hospital in Japan with a long tradition in SILS as well as MPLS, and totally extraperitoneal hernia repair, cholecystectomy, colectomy, gastrectomy, and adhesiolysis are generally performed by means of SILS. Having reported the short-term safety, feasibility, and effectiveness of SILC in the treatment of colorectal cancers [21,22,23,24,25,26], we conducted a study to clarify long-term outcomes of SILC, especially in relation to pathological disease stages. The investigation was carried out as a single-center retrospective cohort study.
Methods
Patients
The study cohort was drawn from among patients with a histologically confirmed stage I to III colon cancer (CC) (a tumor located between the cecum and recto sigmoid colon) who underwent elective curative surgery at Osaka Police Hospital between January 2008 and May 2014. Patients being treated for local recurrence, those with multiple CC lesions, those with another primary malignancy, those who underwent open colectomy, and those who had been treated by chemotherapy or chemo-radiotherapy were excluded from the cohort. Disease stages were based on the Union for International Cancer Control (UICC) TNM Classification of Malignant Tumours, 8th edition [27]. For the purpose of the study, the following data were drawn from patients’ records: patients’ clinical and operative characteristics, including age, sex, and body mass index (BMI); ASA-PS at the time of presentation; location of the tumor; clinical T (cT) stage; clinical N (cN) stage and size of the tumor; operation time; blood loss volume; extent of lymph node dissection based on the Japanese guidelines [28]; number of harvested lymph nodes; and conversion to open surgery or to MPLC and the reason for it. The following pathological variables were also obtained: pathological T (pT) stage and pathological N (pN) stage. Postoperative complications were also noted.
Treatment strategy
The hospital’s general management strategy for patients with CC is in keeping with the Japanese guidelines [28]. Clinical TNM stages were determined before treatment by means of colonoscopy and computed tomography.
Both MPLC and SILC are generally begun with placement of a 3-cm longitudinal incision in the umbilicus by the open method, and a LAPPROTECTOR wound retractor/protector and EZ Access silicon cap (Hakko Medical, Tokyo, Japan) are then placed. For MPLC, a single 12-mm port is placed in the EZ Access, and for right-sided colectomy, 5-mm ports are then inserted in the right lower quadrant, suprapubic region, left lower quadrant, and epigastric region, and for left-sided colectomy, 5-mm ports are then inserted in the right lower quadrant and left upper and lower quadrants, and a 12-mm port is inserted in the right lower quadrant. For SILC, two 12-mm ports and one 5-mm port are placed in the EZ Access. For both MPLC and SILC, the operative procedure is performed with use of 10-mm flexible-tip Olympus EndoEye (Olympus Medical Systems, Tokyo, Japan), standard straight laparoscopic instruments, and laparoscopic coagulation shears (LCS). Basically, Japanese D3 lymph node dissection [28] (complete mesocolic excision for CC and tumor-specific mesocolic resection for rectosigmoid cancer [29] with central vascular ligation) [30], which is nearly the same as complete mesocolic excision with central vascular ligation [31], is performed in cases of clinical stage II/III disease. D2 lymph node dissection (complete pericolic/perirectal and intermediate lymph node dissection) is performed in cases of clinical stage I disease [32]. When right-sided colectomy is performed, whether MPLC or SILC, a medial-to-lateral approach is used to mobilize the colon, the ileocolic artery or the ileocolic artery and right colic artery or the ileocolic and right colic artery plus the middle colic trunk are then isolated and divided, depending on the location of the tumor and variations in the vascular anatomy. When left-sided colectomy is performed, whether MPLC or SILC, a medial-to-lateral approach is used to mobilize the colon, and the inferior mesenteric artery, inferior mesenteric vein, and/or left colic artery are isolated and divided. When SILC is performed, the patient is positioned in such a way to facilitate development and maintenance of the surgical field, and for the same reason, gauze is used to hold neighboring organs under tension. In both SILC and MPLC, the specimen is extracted through the umbilical port site.
SILC was introduced at our hospital in 2009, and by 2011, it had replaced MPLC. According to the UICC TNM classification, adjuvant chemotherapy based on oral 5-fluorouracil prodrugs, FOLFOX (leucovorin calcium [folinic acid], fluorouracil, and oxaliplatin) or CAPOX (capecitabine plus oxaliplatin) [33] was considered and administered for most patients with curatively resected pathological stage III cancer and those with high-risk pathological stage II cancer.
Follow-up
Postoperative follow-up included blood draws for measurement of serum tumor markers at 3-month intervals for 2 years and then at 6-month intervals for the next 3 years, computed tomography (CT) at 6-month intervals for 5 years, and total colonoscopy at the end of year 1 and the end of year 3 [28].
Study endpoints
The primary study endpoint was 5-year cancer-specific survival (CSS), which was defined as CC-free survival from the date of surgery to the date of the 5-year follow-up examination. Data for patients who were alive at the time of the 5-year follow-up examination, with or without disease, and data for patients who died from a non-CC-related cause were censored from the survival analysis. Secondary study endpoints were 3-year disease-free survival (DFS), site(s) of recurrence, surgical outcomes, and the incidence of incisional hernia (IH) at the umbilical scar, which was evaluated on computed tomography images and/or patients’ medical records. DFS time was calculated from the date of surgery to the diagnosis of cancer recurrence, date of death from any cause or diagnosis of a second cancer, or date of the last known follow-up evaluation. Data for patients who were disease-free at the last follow-up were censored from the survival analysis.
Propensity score matching
Propensity score analysis was conducted to adjust for confounding factors. Propensity scores predicting treatment (SILC versus MPLC) based on confounding preoperative covariates including age, sex, tumor size, BMI, ASA-PS, cT stage, and cN stage were calculated by means of logistic regression with a caliper width of 0.2 standard deviations of the logit of the estimated propensity score.
Statistical analysis
Variables are shown as the number (and percentage) of patients or as median (and interquartile [IQR] range) values. Between-group differences in continuous variables were analyzed by Wilcoxon rank-sum test, and differences in categorical variables were analyzed by Pearson’s chi-square test. Survival curves were generated by the Kaplan–Meier method, and differences were analyzed by log-rank test. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated on the basis of unstratified Cox proportional hazard models. All statistical analyses were performed with JMP 15.1.0 (SAS Institute Inc., Cary, NC), and significance was accepted at p < 0.05.
The study was approved by the institutional review board of Osaka Police Hospital (IRB code 1247).
Results
Study patients and their clinical and tumor characteristics
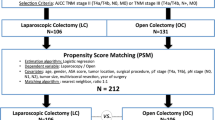
Selection of patients for the study is diagrammed in Fig. 1. Of 819 patients who underwent elective curative surgery at our hospital between January 2008 and May 2014 for histologically confirmed stage I to III CC, 15 were treated for recurrent cancer, 71 underwent open surgery, and 42 were treated for either synchronous or metachronous cancer. These patients were excluded, leaving 691 patients for our analysis: 393 treated by SILC and 298 treated by MPLC. Propensity score matching yielded two groups of 263 patients each (distribution of the logit-transformed propensity scores is shown in Fig. 2). Patients’ clinical and tumor characteristics are for the entire cohort, per treatment group, and for the propensity-score-matched patients, also per treatment group, in Table 1. Among patients in the entire cohort, only ASA-PS, cT stage, and tumor size differed significantly between groups, with ASA-PS being significantly better, cT stage being significantly lower and tumors being significantly smaller in the SILC group than in the MPLC group (p = 0.0005, p = 0.000, and p = 0.0390, respectively). Among propensity-score-matched patients, there was no significant between-group difference in patients’ clinical or tumor characteristics.
Operative outcomes
Operative outcomes and pathological findings are shown in Table 2. Of the numerous operative outcomes assessed, only operation time differed significantly between the two groups, being significantly shorter in the SILC group than in the MPLC group (p = 0.0004). One patient in the SILC group required conversion to MPLC due to the inaccessibility of hepatic flexure from the umbilicus, and nine required conversion to open surgery—three because of severe adhesions and six because of poor visibility. Eight MPLC group patients required conversion to open surgery—five because of severe adhesions and three because of poor visibility. Postoperative outcomes are shown per study group in Table 3. The overall incidence of Clavien-Dindo complications was significantly greater in the MPLC group than in the SILC group (p = 0.016). However, the incidences per grade did not differ significantly between the two groups. IH at the umbilical scar occurred in 21 (8.0%) patients in the SILC group and 17 (6.5%) patients in the MPLC group, without a significant difference between them (p = 0.6139).
Oncological outcomes
The median observation period was 61.3 (59.4–63.4) months for patients in the SILC group and 61.2 months (I60.7–65.9) for patients in the MPLC group. HRs for CCS and DFS in the propensity-matched SILC group were 1.24 (95% CI 0.63–2.46) (p = 0.5286) and 0.31 (95% CI 0.80–2.14 (p = 0.2844), respectively. Kaplan–Meier survival curves are shown for each of the two groups in Fig. 3. Overall 5-year CSS in the propensity-score-matched SILC group was 93.7 (95% CI 89.6–96.2)%, and CSS per pathological disease stage (I, II, and III) was 98.5 (95% CI 90.0–99.8)%, 96.0% (95% CI 88.2–98.7)%, and 88.3 (95% CI, 79.6–93.6)%, respectively, whereas overall 5-year CSS in the propensity-score-matched MPLC group was 93.3% (95% CI, 89.4–95.9), and CSS per pathological disease stage (I, II, and III) was 100% (95% CI not applicable), 95.4 (95% CI 88.3–98.3)%, and 84.1 (95% CI 74.1–90.8)% (p = 0.5278, 0.2679, 0.7666 and 0.9073), respectively. Overall 3-year DFS in the propensity-score-matched SILC group was 94.0 (95% CI 90.2–96.4)%, and 3-year DFS per pathological disease stage was 98.6 (95% CI 90.4–99.8)%, 90.1% (95% CI 81.4–95.0)%, and 79.0 (95% CI 69.4–86.2)%, respectively, whereas overall 3-year DFS in the propensity-score-matched MPLC group was 93.2 (95% CI 89.4–95.7)%, and 3-year DFS per pathological disease stage (I, II and III) was 100% (95% CI, not applicable), 94.5 (95% CI 87.4–97.7)%, and 75.5 (95% CI 64.7–83.8)% (p = 0.2829, 0.7401, 0.4335 and 0.8518), respectively. Thus, oncological outcomes did not differ significantly between groups. Sites and treatment of recurrence are shown per propensity-score-matched group in Table 4. Neither the incidence nor sites of recurrence differed significantly between groups. Overall, the rate at which recurrence was treated did not differ significantly between groups, and the rates at which recurrence was treated by surgery or chemotherapy specifically did not differ significantly between groups, although chemotherapy was much less common in the SILC group. The incidence and sites of recurrence among patients with pathological stage II disease are shown per group in Table 5. Neither the incidence nor sites of recurrence differed between patients in the SILC group and those in the MPLC group (p = 0.3240). Administration vs. non-administration of adjuvant chemotherapy among patients with pathological stage III disease is shown per group in Table 6. There was no significant between-group difference in the percentage of patients given adjuvant chemotherapy or in the percentage of patients who completed such therapy (p = 0.9127 and 0.9555, respectively).
Kaplan–Meier curves for cancer-specific survival among the total matched patients (A), matched pStage I patients (B), matched pStage II patients (C), matched pStage III patients (D), and disease-free survival among the total matched patients (E), matched pStage I patients (F), matched pStage II patients (G), matched pStage III patients (H). 3YCSS, 3-year cancer-specific survival; 5YCSS, 5-year cancer-specific survival; 3YDFS, 3-year disease-free survival; 5YDFS, 5-year disease-free survival; MPLC multiport laparoscopic colectomy, SILC single-incision laparoscopic colectomy
Discussion
Our data indicate that CCS, DFS, site of recurrence, and short-term postoperative complications do not differ between treatment of CC by SILC or by MPLC.
It is difficult to compare our data with data reported from past studies on SILC for CRC due to differences in inclusion and exclusion criteria and/or study endpoints, but there are some notable distinctions. Although the quality of the surgery is best reflected in the 5-year survival of patients with pathological stage II and III disease, some studies of SILC performed for CRC included not only patients with advanced disease but also patients with early-stage disease, and the majority did not cover overall survival and/or DFS at 5 years [34,35,36]. Some studies used postoperative factors including pathological T and pathological N stages for propensity score matching [37, 38], although, in theory, preoperative factors should be used. In a previously reported retrospective study of 5-year survival in a propensity-matched cohort, 96% of the patients were of ASA-PS ≤ 2 [37], a percentage that does not well represent patients treated in real-world clinical practice. In the study described herein, we applied minimal exclusion criteria so that we could evaluate surgical and oncological outcomes of SILC vs. those of MPLC obtained in real-world settings. The 88.3% 5-year CSS and 71.9% 5-year DFS achieved as a result of SILC were even better than the 82% 5-year CCS and the 62% 5-year DFS documented in a SILC case series [39], and the 79.0% 3-year DFS achieved as a result of SILC was better than the 65% 3-year DFS documented through pooled analysis of randomized trials of various adjuvant chemotherapy regimens used in cases of pathological stage III CC [40]. The question of whether the surgical technique, especially open or conventional laparoscopic surgery, is responsible for the recurrence of CRC remains [41, 42], but we note here that we found no significant difference in the sites of recurrence between SILC and MPLC.
We also found short-term surgical outcomes to be fairly consistent with those of previously reported studies. However, we did find operation time to be significantly shorter for patients who underwent SILC than for those who underwent MPLC, a finding not consistent with that of previously reported studies [35, 37, 43]. A possible explanation for the discrepancy is that the surgeons who perform MPLC may be less experienced than those who perform SILC and require assistance, thus, taking the same amount of time to perform MPLC as that taken by surgeons who perform SILC. Although the rate of conversion from SILC to MPLC or open surgery among our study patients was 3.8% and within previously reported range of 0% to 9.5% [34,35,36,37,38], the need we encountered to add a port was specific to SILC, namely, an inability to access the splenic flexure from the umbilicus. That inability would have been overcome in MPLC with use of an alternative port. This means that the feasibility of SILC is influenced by patients’ anatomy even above the pelvis, if protrusion of the sacral promontory is exaggerated [44].
Although the incidence of IH following SILS, especially single-incision laparoscopic cholecystectomy, is reported from some studies to be higher than that following MPLS [45, 46], the incidence of SILC-associated IH remains unclear [47, 48]. The documented incidence of IH did not differ significantly between our SILC group and our MPLC group, possibly due to the fact that some known risk factors for IH, including obesity, specimen extraction through the umbilical port site, and surgical site infection [47, 49], did not differ significantly between our propensity-score-matched SILC and MPLC groups.
Our study findings should be interpreted in light of our study limitations. Because the study was retrospective in nature and included patients from a single institution, there is a potential for selection bias despite the propensity score matching. Further, variables such as perioperative care were not factored into the analysis. Advances in treatment, including systemic chemotherapy, which were implemented during the study period [50] might also have influenced our study results, although the rates of induction and completion of adjuvant chemotherapy were similar between the two groups. The possibility of a type 2 statistical error cannot be ruled out. Randomized clinical trials have been conducted, and results in terms of long-term outcomes are expected to be released in the near future [17, 35]. Nonetheless, considering that reports of SILC in the real-world CC population are limited, we believe the data reported herein will help surgeons in considering SILC for CC surgery. On the basis of our experience thus far, we conclude that SILC is a possible option for surgical treatment of CC. We caution that the procedure should be performed by surgeons with expertise in SILS.
References
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr., Hellinger M, Flanagan R, Jr., Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surgery 246:655–662; discussion 662–654
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Hewett PJ, Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Rieger NA, Smith JS, Solomon MJ, Stephens JH, Stevenson AR (2008) Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg 248:728–738
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y, Kitano S (2014) Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg 260:23–30
Haueter R, Schutz T, Raptis DA, Clavien PA, Zuber M (2017) Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg 104:1141–1159
Lo CW, Yang SS, Tsai YC, Hsieh CH, Chang SJ (2016) Comparison of laparoendoscopic single-site versus conventional multiple-port laparoscopic herniorrhaphy: a systemic review and meta-analysis. Hernia 20:21–32
Xu AM, Huang L, Li TJ (2015) Single-incision versus three-port laparoscopic appendectomy for acute appendicitis: systematic review and meta-analysis of randomized controlled trials. Surg Endosc 29:822–843
Makino T, Milsom JW, Lee SW (2012) Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg 255:667–676
Podda M, Saba A, Porru F, Pisanu A (2016) Systematic review with meta-analysis of studies comparing single-incision laparoscopic colectomy and multiport laparoscopic colectomy. Surg Endosc 30:4697–4720
Yang TX, Chua TC (2013) Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Colorectal Dis 28:89–101
Luján JA, Soriano MT, Abrisqueta J, Pérez D, Parrilla P (2015) Single-port colectomy VS multi-port laparoscopic colectomy. systematic review and meta-analysis of more than 2800 procedures. Cir Esp 93:307–319
Hoyuela C, Juvany M, Carvajal F (2017) Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: a systematic review and meta-analysis. Am J Surg 214:127–140
Maggiori L, Tuech JJ, Cotte E, Lelong B, Denost Q, Karoui M, Vicaut E, Panis Y (2018) Single-incision laparoscopy versus multiport laparoscopy for colonic surgery: a multicenter, double-blinded, randomized controlled trial. Ann Surg 268:740–746
Kang BM, Kim HJ, Kye BH, Lee SC, Lee KY, Park SJ, Lee SH, Lim SW, Lee YS, Kim JH, Lee J, Kim MK, Kim JG (2018) Multicenter, randomized single-port versus multiport laparoscopic surgery (SIMPLE) trial in colon cancer: an interim analysis. Surg Endosc 32:1540–1549
Watanabe J, Ota M, Fujii S, Suwa H, Ishibe A, Endo I (2016) Randomized clinical trial of single-incision versus multiport laparoscopic colectomy. Br J Surg 103:1276–1281
Hiraki M, Takemasa I, Uemura M, Haraguchi N, Nishimura J, Hata T, Mizushima T, Yamamoto H, Doki Y, Mori M (2014) Evaluation of invasiveness in single-site laparoscopic colectomy, using “the PainVision system” for quantitative analysis of pain sensation. Surg Endosc 28:3216–3223
team TACSmaec (2020) Survival Rates for Colorectal Cancer.
(2005) 2005 Update of ASCO Practice Guideline Recommendations for Colorectal Cancer Surveillance: Guideline Summary. J Oncol Pract 1:137–139
Tei M, Otsuka M, Suzuki Y, Akamatsu H (2018) Initial experience of single-port laparoscopic multivisceral resection for locally advanced colon cancer. Surg Laparosc Endosc Percutan Tech 28:108–112
Tei M, Otsuka M, Suzuki Y, Kishi K, Tanemura M, Akamatsu H (2018) Safety and feasibility of single-port surgery for colon cancer in octogenarians. Anticancer Res 38:2967–2972
Tei M, Otsuka M, Suzuki Y, Kishi K, Tanemura M, Akamatsu H (2018) Clinical outcomes of single-port surgery for colon cancer in octogenarians. Surg Laparosc Endosc Percutan Tech 28:164–169
Tei M, Otsuka M, Suzuki Y, Kishi K, Tanemura M, Akamatsu H (2018) Safety and feasibility of single-port laparoscopic low anterior resection for upper rectal cancer. Am J Surg 216:1101–1106
Tei M, Wakasugi M, Omori T, Ueshima S, Tori M, Akamatsu H (2015) Single-port laparoscopic colectomy is safe and feasible in patients with previous abdominal surgery. Am J Surg 209:1007–1012
Suzuki Y, Tei M, Wakasugi M, Masuzawa T, Ohtsuka M, Mikamori M, Saito T, Furukawa K, Imasato M, Kishi K, Tanemura M, Akamatsu H (2020) Role of single-incision laparoscopic surgery in the management of small bowel obstruction. Surg Endosc. https://doi.org/10.1007/s00464-020-07671-9
James D. Brierley MKG, Christian Wittekind (2016) TNM Classification of Malignant Tumours, 8 edn, John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK
Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34
Zaheer S, Pemberton JH, Farouk R, Dozois RR, Wolff BG, Ilstrup D (1998) Surgical treatment of adenocarcinoma of the rectum. Ann Surg 227:800–811
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis 11:354–364; discussion 364–355
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Rectum JSfCotCa (2019) Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3d English Edition [Secondary Publication]. J Anus Rectum Colon 3:175–195
Boyne DJ, Cuthbert CA, O’Sullivan DE, Sajobi TT, Hilsden RJ, Friedenreich CM, Cheung WY, Brenner DR (2019) Association between adjuvant chemotherapy duration and survival among patients with stage II and III colon cancer: a systematic review and meta-analysis. JAMA Netw Open 2:e194154
Kim CW, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2017) Oncologic outcomes of single-incision laparoscopic surgery for right colon cancer: a propensity score-matching analysis. Int J Surg 45:125–130
Song Z, Li Y, Liu K, Jiang Y, Shi Y, Ji X, Zhang T, Wu H, Shi Y, Zhao R (2019) Clinical and oncologic outcomes of single-incision laparoscopic surgery for right colon cancer: a propensity score matching analysis. Surg Endosc 33:1117–1123
Yun JA, Yun SH, Park YA, Huh JW, Cho YB, Kim HC, Lee WY (2016) Oncologic outcomes of single-incision laparoscopic surgery compared with conventional laparoscopy for colon cancer. Ann Surg 263:973–978
Miyo M, Takemasa I, Ishihara H, Hata T, Mizushima T, Ohno Y, Doki Y, Mori M (2017) Long-term outcomes of single-site laparoscopic colectomy with complete mesocolic excision for colon cancer: comparison with conventional multiport laparoscopic colectomy using propensity score matching. Dis Colon Rectum 60:664–673
Katsuno G, Fukunaga M, Nagakari K, Yoshikawa S, Azuma D, Kohama S (2016) Short-term and long-term outcomes of single-incision versus multi-incision laparoscopic resection for colorectal cancer: a propensity-score-matched analysis of 214 cases. Surg Endosc 30:1317–1325
Hirano Y, Hiranuma C, Hattori M, Douden K, Yamaguchi S (2019) Long-term oncological outcomes of single-port laparoscopic surgery for colon cancer. ANZ J Surg 89:408–411
Schmoll HJ, Twelves C, Sun W, O’Connell MJ, Cartwright T, McKenna E, Saif M, Lee S, Yothers G, Haller D (2014) Effect of adjuvant capecitabine or fluorouracil, with or without oxaliplatin, on survival outcomes in stage III colon cancer and the effect of oxaliplatin on post-relapse survival: a pooled analysis of individual patient data from four randomised controlled trials. Lancet Oncol 15:1481–1492
Nagata H, Kawai K, Hata K, Tanaka T, Nozawa H, Ishihara S (2020) Laparoscopic surgery for T4 colon cancer: a risk factor for peritoneal recurrences? Surgery 168:119–124
Hasegawa H, Okabayashi K, Watanabe M, Ashrafian H, Harling L, Ishii Y, Sugiyama D, Seishima R, Darzi A, Athanasiou T, Kitagawa Y (2014) What is the effect of laparoscopic colectomy on pattern of colon cancer recurrence? A propensity score and competing risk analysis compared with open colectomy. Ann Surg Oncol 21:2627–2635
Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST (2011) The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg 254:933–940
Hamabe A, Takemasa I, Uemura M, Nishimura J, Mizushima T, Ikeda M, Yamamoto H, Sekimoto M, Doki Y, Mori M (2014) Feasibility of single-port laparoscopic surgery for sigmoid colon and rectal cancers and preoperative assessment of operative difficulty. J Gastrointest Surg 18:977–985
Antoniou SA, Garcia-Alamino JM, Hajibandeh S, Weitzendorfer M, Muysoms FE, Granderath FA, Chalkiadakis GE, Emmanuel K, Antoniou GA, Gioumidou M, Iliopoulou-Kosmadaki S, Mathioudaki M, Souliotis K (2018) Single-incision surgery trocar-site hernia: an updated systematic review meta-analysis with trial sequential analysis by the Minimally Invasive Surgery Synthesis of Interventions Outcomes Network (MISSION). Surg Endosc 32:14–23
Connell MB, Selvam R, Patel SV (2019) Incidence of incisional hernias following single-incision versus traditional laparoscopic surgery: a meta-analysis. Hernia 23:91–100
Buckley FP 3rd, Vassaur HE, Jupiter DC, Crosby JH, Wheeless CJ, Vassaur JL (2016) Influencing factors for port-site hernias after single-incision laparoscopy. Hernia 20:729–733
Watanabe J, Ishibe A, Suwa Y, Suwa H, Ota M, Kubota K, Yamanaka T, Kunisaki C, Endo I (2020) Hernia incidence following a randomized clinical trial of single-incision versus multi-port laparoscopic colectomy. Surg Endosc
Benlice C, Stocchi L, Costedio MM, Gorgun E, Kessler H (2016) Impact of the specific extraction-site location on the risk of incisional hernia after laparoscopic colorectal resection. Dis Colon Rectum 59:743–750
Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TM, Myklebust T, Tervonen H, Thursfield V, Ransom D, Shack L, Woods RR, Turner D, Leonfellner S, Ryan S, Saint-Jacques N, De P, McClure C, Ramanakumar AV, Stuart-Panko H, Engholm G, Walsh PM, Jackson C, Vernon S, Morgan E, Gavin A, Morrison DS, Huws DW, Porter G, Butler J, Bryant H, Currow DC, Hiom S, Parkin DM, Sasieni P, Lambert PC, Møller B, Soerjomataram I, Bray F (2019) Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol 20:1493–1505
Acknowledgements
The authors thank Dr. Michitaka Honda of Fukushima Medical University for his advice on statistical issues and Prof. Tina Tajima of St. Marianna University School of Medicine for her meticulous English editing.
Funding
The work described herein was supported by departmental resources only.
Author information
Authors and Affiliations
Contributions
YS and MT conceived and designed the study, YS, MT, MW, MO, and HA acquired data, YS, MT, and HA analyzed and interpreted the data, YS drafted the manuscript, MT, MW, YN, AN, MM, KF, MO, JM, MI, TA, KK, and HA critically revised the article and MT, MW, YN, AN, MM, KF, MO, JM, MI, TA, KK, and HA approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Disclosures
None of the authors: Yozo Suzuki, Mitsyoshi Tei, Masaki Wakasugi, Toru Masuzawa, Masahisa Ohtsuka, Manabu Mikamori, Takuro Saito, Kenta Furukawa, Mitsunobu Imasato, Kentaro Kishi, Masahiro Tanemura, or Hiroki Akamatsu has a conflict of interest or financial tie to disclose.
Ethical Approval
The present manuscript is an original contribution not previously published and not under consideration for publication elsewhere, and, if accepted, will not be published anywhere in similar form, in any language. All authors have read and approved the manuscript, and the study was approved by the institutional research ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, Y., Tei, M., Wakasugi, M. et al. Long-term outcomes of single-incision versus multiport laparoscopic colectomy for colon cancer: results of a propensity score-based analysis. Surg Endosc 36, 1027–1036 (2022). https://doi.org/10.1007/s00464-021-08367-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08367-4