Abstract
Background
There is a paucity of prospective data related to surgeon ergonomics, which affects career longevity. Robotic surgical systems may mitigate pain and workload. We hypothesized that ergonomic outcomes would vary based on surgeon height and gender, and the relative benefit of robotic surgery would vary based on these demographics.
Methods
Surgeons received questionnaires to fill out immediately before and after surgery to enable calculation of pain scores and task load. Surgeons who were ≤ 66 inches tall were considered “short”. Univariable and multivariable regression analyses were performed where appropriate using Stata-MP version 14.2 (StataCorp LLC, College Station, TX).
Results
There were 124 questionnaires given to 20 surgeons; 97 (78%) were returned, and 12 (12%) laparoscopic operations were excluded, leaving 85 (69%) questionnaires for further analysis: 33 (38%) from short surgeons, and 24 (28%) from women, for 30 (35%) robotic and 55 (65%) open operations. There were 44/85 (52%) surgeons who reported worse pain after surgery. Overall pain scores (1.1 ± 2.6 vs 1.5 ± 2.6, p = 0.70) were similar for robotic and open operations. In multivariable analysis, greater surgeon pain scores were significantly associated with short surgeons (p < 0.001), male surgeons (p < 0.001), and long operative times (p = 0.03). Physical demand was lower for robot vs open operations (median 10 vs 13, p = 0.03). When short surgeons (p = 0.04) and male surgeons (p = 0.03) were examined as sub-groups, lower physical demand during robotic operations persisted, but was lost when only examining tall surgeons (p = 0.07) and female surgeons (p = 0.13).
Conclusions
Short surgeons and male surgeons reported significantly more pain after both open and robotic operations but had less physical demand when using the robotic system. Future work should focus on mitigation of surgeon height-related factors and seek to understand ergonomic gender differences beyond height.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgeon ergonomics affects career longevity. Up to 40% of surgeons report work-related musculoskeletal injures, and approximately half seek treatment [1]. Injuries may lead to missed work, fewer operations being performed, and impaired performance in the operating room [2]. Thus, while the surgical field has historically fostered a culture of self-sacrifice [1], many surgeons believe this an important subject to examine [3]. Robotic surgery is increasingly being used [4], and given an absence of data to demonstrate robotic superiority [5] with additional concerns about cost [6], many arguments in favor of robotic surgery are related to surgeon comfort [7,8,9]. Prospective ergonomic data from surgeons are sparse. Most surgeons report pain is greater during open compared to robotic operations [10] given the ergonomic advantages of robotic surgery. Namely, the operative surgeon is sitting down un-scrubbed, performing surgery by looking into a zoomed in three-dimensional video display, using pincer hand controls and foot pedals. Beyond the ability to sit and rest one’s arms during robotic procedures, discomfort related to table height [3] and instrument size/weight [11] are avoided. We therefore hypothesized that surgeon height would affect surgeon discomfort related to operating, and that ergonomic benefit from the robot would vary based on surgeon height. Since female and male surgeons often have different height [11], we further hypothesized that there would be a differential ergonomic benefit from the robotic platform based on gender. To evaluate this, we prospectively collected data from surgeons including demographics, body discomfort before and after surgery, procedure-specific information, and mental and physical task load related to performing the surgery.
Methods
Over a one-month period, surgeons were provided with questionnaires to fill out immediately before and after surgery. Information regarding surgeon demographics, the surgery performed, intraoperative ergonomics, and task load during surgery were queried. All robotic operations were performed using either the da Vinci Xi or Si robotic system (Intuitive Surgical, Inc., Sunnyvale, CA). While individual surgeons were noted as first time or repeat participants when they were given blank questionnaires to enable a participant count, there were no patient or surgeon identifiers on the questionnaires, allowing for anonymous completion. Completed questionnaires were returned either to the first author or placed in a locked box in the surgeon dictation room. A drop in questionnaire return rates was noted during the study; this was addressed after 44 questionnaires had been collected by giving surgeons a $5 gift card with the questionnaire as an incentive to complete and return.
Pain was ranked on the questionnaire before and after surgery using the Body Part Discomfort scale [12] (Fig. 1A). Pain was scored from 0 (no pain) to 4 (severe pain) to calculate a pain score (pre-surgery minus post-surgery pain), which was then categorized as better, the same, or worse pain after surgery for the entire body, and for the following body areas: neck/shoulders, upper back, lower back, arms, and legs. Task loads were assessed on the questionnaire after surgery using the National Aeronautics and Space Administration (NASA) Task Load Index (Fig. 1B), which measures mental demand, physical demand, temporal demand, performance, effort, and frustration [13]. Raw scores for each task load type range from 1 (no demand) to 20 (maximum demand), and total task load ranges from 6 (no demand for all task load types) to 120 (maximum demand on all task load types). Surgeons who were ≤ 66 inches tall were considered short (below average adult height in the US [14]). Obesity was defined by body mass index [15].
Chi-squared analysis, Z-score, Student’s T-test, Mann–Whitney, Kolmogorov–Smirnov, univariable and multivariable linear and logistic regression analyses with and without interaction were performed where appropriate using Stata-MP version 14.2 (StataCorp LLC, College Station, TX). Initial selection of variables within models were theory driven and optimized using Akaike and Bayesian information criteria. This study was reviewed by the institutional review board (IRB) and determined to be exempt. Per the IRB, all surgeons who were provided with a questionnaire were also provided with a form explaining their implied consent by completing the survey and returning it.
Results
There were 124 questionnaires given to 20 surgeons; 97 (78%) were returned. Laparoscopic operations were excluded (n = 12), leaving 85 questionnaires for further analysis: 33 (38%) from shorter surgeons (≤ 66 inches tall), and 24 (28%) from women, for 30 (35%) robotic and 55 (65%) open operations (Table 1). Robotic surgery was more often used by surgeons age 41–50 years old (p = 0.03), by surgeons with higher monthly operative volume (p = 0.05), and when surgery was performed in the lower abdomen/pelvis (p < 0.001). Surgical times were lower for robotic operations (3.1 ± 0.5 vs 4.2 ± 0.7 h, p = 0.04); however, median surgical time for all operations was 3 h, and there were similar numbers of short (< 3 h) and long (3 + hours) operations in the open and robotic surgical groups (p = 0.25). During robotic operations, surgeons less often used a step stool (< 0.001), and less often took a 5 min or longer break during surgery (p = 0.05). Additional characteristics including surgeon gender, surgeon height, patient BMI, and estimated blood loss were similar between captured robotic and open operations.
Surgeon pain scores
There were 44/85 (52%) surgeons who reported worse pain after surgery. Overall average pain scores (1.1 ± 2.6 vs 1.5 ± 2.6, p = 0.70) were similar for robotic and open operations. Pain scores by specific body area were further compared by height, gender, and operative approach (Fig. 2). The primary affected body areas were the neck/shoulders and lower back. Short surgeons had greater upper back (p = 0.01), lower back (p = 0.04), lower extremity (p = 0.04), and neck/shoulder pain (p = 0.001). There was also a difference in lower back pain for open versus robotic surgery (p = 0.006). Specifically, a greater number of surgeons had increased lower back pain after performing robotic surgery (40% vs 27%), but some surgeons conversely reported an improvement in lower back pain after robotic surgery, a phenomenon which did not occur after open surgery (13% vs 0%). Of note, differences in hand/arm pain scores by group were not observed.
Frequency of pain reported by body region for A Surgical approach, B Surgeon gender, and C. Surgeon height. “Better”, “Same”, and “Worse” refer to the comparison of pain before performing surgery to pain after performing surgery. The left and right sides of each graph indicate the variables being compared. Bars extending further from center indicate increasing percentage of surgeons with a pain score in that group. Bold* = statistically significant
Regression analysis was performed to compare overall pain scores by surgeon and surgery variables (Table 2). In univariable analysis, greater surgeon pain scores were significantly associated with long operative times (p = 0.02). In multivariable analysis, greater surgeon pain scores were significantly associated with short surgeon stature (p < 0.001), male surgeon gender (p < 0.001), and long operative times (p = 0.03). While there were no tall women in the surgeon cohort, pain differences by gender persisted when only short surgeons as a sub-group were examined (p = 0.002), and when the model included an interaction between gender and height (p < 0.001), with no additional significant factors identified.
Surgical task load
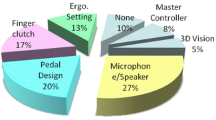
Task load histograms are presented in Fig. 3. The median surgeon task load ratings for mental demand, physical demand, temporal demand, and effort were lower for robotic compared to open operations, but this difference only achieved statistical significance for physical demand (robot median 10, range 1–16; open median 13, range 1–20, p = 0.03). When shorter surgeons (p = 0.04) and male surgeons (p = 0.03) were examined as sub-groups, lower physical demand during robotic operations persisted; this association was lost when only examining tall surgeons (p = 0.07) and female surgeons (p = 0.13).
Histograms of the raw NASA Task Load Index components and total raw NASA Task Load score comparing robotic to open operations. The x-axis is the task load score, and y-axis is the number of respondents. Higher numbers on the x-axis indicate increased task load, and taller lines on the y-axis indicate more respondents per score. Heavy black lines indicate the median score. Bold* = statistically significant
Overall task load for robotic (median 48, range 6–106) and open (median 64, range 9–98) operations were similar. In multivariable analysis including gender, age, surgeon height, operative time, operative approach, patient BMI, and pain score, the only variable significantly associated with above median overall task load was long operative time (OR 3.2, 95% CI 1.1–9.2, p = 0.03). This association persisted when only short surgeons were examined as a sub-group (OR 15.9, 95% CI 1.2–217.1, p = 0.04). Conversely, when examining only tall surgeons, this association was lost (p = 0.34).
Discussion
The present study is a prospective evaluation of surgeon task load and pain after performing surgery for 20 surgeons who performed 85 operations. We found that surgeons ≤ 66 inches in height (short surgeons) reported significantly more pain compared to their taller counterparts after both open and robotic operations. Men also reported more pain than women. While there were no tall women in the surgeon cohort studied, this gender difference persisted in multivariable analysis and when only short surgeons were examined. Additionally, the physical demand component of task load was rated lower for robotic operations. In sub-group analysis this finding persisted for shorter surgeons and male surgeons but was lost for taller surgeons and female surgeons. Thus, we did find that ergonomics in the operating room differed by surgeon height and surgeon gender.
Our findings are comparable to previous survey-based studies, in which more than two thirds of surgeons recall pain related to performing surgery [1, 10]. There are, however, some differences. Lee et al. reported the results of a survey given to general, urologic, and gynecologic surgeons, and found no specific demographic associated with increased pain during robotic surgery other than increased low back stiffness for those who performed > 200 robotic cases/year [16]. Plerhoples et al. surveyed robotically trained surgeons, and found that taller surgeons more often attributed their pain to open surgery compared to robotic surgery [10]. Sutton et al. surveyed members of the Society of American Gastrointestinal and Endoscopic Surgeons and similarly found that taller surgeons as well as male surgeons more often reported lower back and lower extremity discomfort [11]. While the present study also showed increased pain for male participants, we conversely found that shorter surgeons experienced more pain and physical demand during both open and robotic operations. A potential reason for the difference in findings between survey-based studies and the present study may be the influence of recall bias and/or the inability to adjust for surgical time, which we also found significantly influenced surgeon pain after performing surgery.
This work does have limitations. Its emphasis is on acute pain and does not address chronic pain in surgeons present before surgery that is believed to be work-related. This may account for a substantial amount of pain experienced by surgeons while in the operating room, and is better addressed by longitudinal and survey-based studies [1]. It should also be noted that we did not compare ergonomic results from traditional laparoscopic surgery. The primary reason for this is because our institution was an early adopter of robotic technology [17] and continues to have a focus on robotic surgery. As such, the number of operations performed with traditional laparoscopy were too low to provide meaningful comparisons. We have demonstrated previously that institutional factors play a role in the use of robotic surgery [18]. This is likely due to the upfront investment and infrastructure required from the surgeons, operating room staff, and the institution, which influences surgeon choice of approach [19]. Survey studies show that surgeons attribute occupation-related pain most often to laparoscopic surgery [1, 9,10,11]. In contrast, prospective studies that evaluate pain immediately after surgery are less conclusive. A study of 16 post-surgery questionnaires showed no significant difference in pain, stiffness, or numbness for surgeons performing open and laparoscopic surgeries [20]. Another study that performed workplace ergonomic risk assessments on 81 surgeons found similar values for those performing open and laparoscopic operations [21]. Armijo et al. compared neck and upper extremity electromyography (EMG) activations in 16 surgeons performing laparoscopic and robotic operations, and demonstrated that muscle fatigue and self-reported fatigue were similar [22]. Their work and others corroborate our finding that robotic surgery is not always “pain free,” and that further ergonomic optimization may be possible [16, 22, 23].
To continue nationwide efforts in improving academic medicine inclusivity [24, 25], future work studying surgical ergonomics should further examine mitigation of surgeon height-related factors. We found that more than 50% of surgeons used a step stool during open operations; the issue of table height as it pertains to surgeon ergonomics has long been known and has been reported to affect both men and women [11, 26]. Data related to step stool type and availability, as well as number of steps used may be helpful. Additional work should also seek to understand why male and female surgeon ergonomics might differ beyond height [1].
References
Stucky C-CH, Cromwell KD, Voss RK et al (2018) Surgeon symptoms, strain, and selections: systematic review and meta-analysis of surgical ergonomics. Ann Med Surg 27:1–8
Davis WT, Fletcher SA, Guillamondegui OD (2014) Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res 189(2):207-212.e6. https://doi.org/10.1016/j.jss.2014.03.013
Wauben L, Van Veelen M, Gossot D, Goossens R (2006) Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc Other Interv Techn 20(8):1268–1274
Stewart CL, Ituarte PHG, Melstrom KA et al (2019) Robotic surgery trends in general surgical oncology from the National Inpatient Sample. Surg Endosc 33(8):2591–2601. https://doi.org/10.1007/s00464-018-6554-9
Jayne D, Pigazzi A, Marshall H et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580. https://doi.org/10.1001/jama.2017.7219
Barbash GI (2010) New technology and health care costs–the case of robot-assisted surgery. N Engl J Med 363(8):701
Tarr ME, Brancato SJ, Cunkelman JA, Polcari A, Nutter B, Kenton K (2015) Comparison of postural ergonomics between laparoscopic and robotic sacrocolpopexy: a pilot study. J Minim Invasive Gynecol 22(2):234–238. https://doi.org/10.1016/j.jmig.2014.10.004
Szeto GP, Poon JT, Law WL (2013) A comparison of surgeon’s postural muscle activity during robotic-assisted and laparoscopic rectal surgery. J Robot Surg 7(3):305–308. https://doi.org/10.1007/s11701-012-0374-z
Law KE, Lowndes BR, Kelley SR et al (2020) NASA-Task Load Index differentiates surgical approach: opportunities for improvement in colon and rectal surgery. Ann Surg 271(5):906–912. https://doi.org/10.1097/sla.0000000000003173
Plerhoples TA, Hernandez-Boussard T, Wren SM (2012) The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg 6(1):65–72. https://doi.org/10.1007/s11701-011-0330-3
Sutton E, Irvin M, Zeigler C, Lee G, Park A (2014) The ergonomics of women in surgery. Surg Endosc 28(4):1051–1055
Corlett EN, Bishop R (1976) A technique for assessing postural discomfort. Ergonomics 19(2):175–182
Hart SG (2006) NASA-task load index (NASA-TLX); 20 years later. Sage publications Sage CA, Los Angeles, pp 904–908
Fryar CD, Kruszan-Moran D, Gu Q, Ogden CL (2018) Mean body weight, weight, waist circumference, and body mass index among adults: United States, 1999–2000 through 2015–2016
Centers for Disease Control and Prevention (2020) Defining Adult Overweight and Obesity. Accessed Sept 28, 2020
Lee G, Lee M, Green I, Allaf M, Marohn M (2017) Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surg Endosc 31(4):1697–1706
Link BA, Nelson R, Josephson DY, Lau C, Wilson TG (2009) Training of urologic oncology fellows does not adversely impact outcomes of robot-assisted laparoscopic prostatectomy. J Endourol 23(2):301–306
Stewart CL, Dumitra S, Nota C et al (2019) Hospital factors strongly influence robotic use in general surgery. Surgery 166(5):867–872
BenMessaoud C, Kharrazi H, MacDorman KF (2011) Facilitators and barriers to adopting robotic-assisted surgery: contextualizing the unified theory of acceptance and use of technology. PLoS ONE 6(1):e16395
Nguyen NT, Ho HS, Smith WD et al (2001) An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg 182(6):720–724
Aghilinejad M, Ehsani AA, Talebi A, Koohpayehzadeh J, Dehghan N (2016) Ergonomic risk factors and musculoskeletal symptoms in surgeons with three types of surgery: Open, laparoscopic, and microsurgery. Med J Islam Repub Iran 30:467
Armijo PR, Huang C-K, High R, Leon M, Siu K-C, Oleynikov D (2019) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc 33(7):2323–2331
Craven R, Franasiak J, Mosaly P, Gehrig PA (2013) Ergonomic deficits in robotic gynecologic oncology surgery: a need for intervention. J Minim Invasive Gynecol 20(5):648–655
Acosta D (2020) Achieving excellence through equity, diversity, and inclusion. Association of American Medical Colleges. Accessed Oct 9, 2020, https://www.aamc.org/news-insights/achieving-excellence-through-equity-diversity-and-inclusion
Aysola J, Barg FK, Martinez AB et al (2018) Perceptions of factors associated with inclusive work and learning environments in health care organizations: a qualitative narrative analysis. JAMA Netw Open 1(4):e181003–e181003. https://doi.org/10.1001/jamanetworkopen.2018.1003
Berquer R, Smith WD, Davis S (2002) An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc Interv Tech 16(3):416–421. https://doi.org/10.1007/s00464-001-8190-y
Funding
Portions of this work were funded by the American Cancer Society MRSG 16–047-01-MPC. Dr. Yuman Fong has the following disclosures, all unrelated to this work: scientific consultant for Medtronic, Johnson and Johnson, Olympus, Avra Robotics, Perfint Robotics, and Intuitive Surgical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Camille Stewart, Mustafa Raoof, Thanh Dellinger, and Susanne Warner have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stewart, C., Raoof, M., Fong, Y. et al. Who is hurting? A prospective study of surgeon ergonomics. Surg Endosc 36, 292–299 (2022). https://doi.org/10.1007/s00464-020-08274-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08274-0