Abstract
Background
Controversy exists regarding the safety and effectiveness of minimally invasive inguinal hernia repairs in patients with a history of prior urologic pelvic operations (PUPO), such as a prostatectomy, which causes scarring and disruption of the retropubic tissue planes. Our study sought to examine whether a history of PUPO impacts surgical outcomes in males undergoing robotic-assisted inguinal hernia repair.
Methods
The Americas Hernia Society Quality Collaborative (AHSQC) database was queried to identify male patients who underwent a robotic inguinal hernia repair with 30-day follow-up. A sub-query was performed to identify subjects within the cohort with a documented history of PUPO. Propensity score matching was subsequently utilized to evaluate for differences in intra-operative complications and short-term post-operative outcomes.
Results
In total, 1664 male patients underwent robotic-assisted inguinal hernia repair, of whom 65 (3.9%) had a PUPO. After a 3:1 propensity score matching with hernia repair patients who did not have prior procedures, 195 (11.7%) males were included in the comparison cohort. There were no documented vascular, bladder, or spermatic cord injuries in either group. There was no difference in 30-day readmission rate (5% vs. 3%, respectively, p = 0.41). No hernia recurrences were recorded within the 30-day follow-up period in either group. There was no statistical difference in post-operative complications (including seroma formation, hematoma, and surgical site occurrences) between the two groups (14% vs. 8%, p = 0.18).
Conclusions
In an experienced surgeon’s hands, robotic-assisted minimally invasive inguinal hernia repair may be an alternative to open repair in patients with PUPO who were previously thought to be poor minimally invasive surgical candidates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The lifetime occurrence for the development of a groin hernia can be as high as 27–43% in males and 3–6% in females, making inguinal hernia repair one of the most commonly performed surgical operations worldwide [1]. Although open inguinal hernia repair remains the most common approach, minimally invasive surgery (MIS) techniques such as the totally extra-peritoneal (TEP) and trans-abdominal pre-peritoneal (TAPP) approach are becoming increasingly popular [2]. Consensus groups have acknowledged the advantage of these MIS techniques, including reduced early and late post-operative pain and faster recovery times compared to the open anterior approach [3].
The MIS techniques utilize a posterior approach, which involves dissecting through the retropubic space of Retzius to obtain exposure of the myopectineal orifice and reduce any hernia contents. In patients with a history of a prior urologic pelvic operation (PUPO), especially in male patients with a previous prostatectomy, the scar tissue formed in the retropubic space creates an increased level of operative difficulty and an added potential risk for complications. The HerniaSurge group acknowledged this perceived risk in their 2018 international guidelines by recommending that surgeons consider an anterior open approach when performing hernia repair on patients with prior pelvic surgery or radiation [3].
Of the two more common MIS techniques, the TAPP approach is most amenable to robotic assistance [4]. This offers the surgeon improved dexterity in the form of wristed instrumentation and an enhanced high-definition three-dimensional image. Many surgeons are utilizing the robotic platform to increase their scope of MIS and are now offering robotic-TAPP to patients previously regarded as higher risk for an MIS approach.
The aim of this retrospective study was to determine if a history of PUPO has an impact on surgical outcomes in males undergoing a robotic-assisted inguinal hernia repair.
Materials and methods
After obtaining approval from the Beaumont Health Institutional Review Board, a data query were submitted to the Americas Hernia Society Quality Collaborative (AHSQC). The AHSQC is a quality improvement database developed by the Americas Hernia Society in an effort to improve patient outcomes and optimize the cost for hernia repairs. The database contains surgeon-entered patient data including demographics, preoperative evaluation, operative details, 30-day follow-up, and patient-entered long-term follow-up data from over 45,000 patients with 325 contributing surgeons as of 2019.
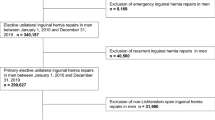
The dataset was queried to identify all male subjects who had undergone a robotic-assisted inguinal hernia repair (RIHR). The type of RIHR [i.e. TAPP, TEP, or intra-peritoneal onlay mesh (IPOM)] was not specifically sub-characterized. The dataset was than further filtered by patients with a documented history of prior pelvic surgery, specifically with a history of a urologic pelvic operation. Information was not available on the specific urologic pelvic operation performed (prostatectomy, cystoprostatectomy, bladder augmentation, etc.) We excluded subjects without 30-day follow-up. Females were also excluded to narrow our study population to focus on suspected prior prostatectomy patients.
A propensity score-matched control cohort of RIHR subjects with no history of prior urologic operation was identified using age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) class, and current nicotine use as matching variables. A 3-to-1 matching ratio was used with caliper width of 0.25.
Variables of interest collected included patient characteristics (demographic information and comorbidities), intra-operative complications, and post-operative outcomes including surgical site occurrences (SSO), surgical site infections (SSI), surgical site occurrences requiring procedural interventions (SSOPI), readmissions, re-operations, hernia recurrences, and other complications within 30 days of the operation. Statistical analysis included descriptive statistics, Pearson Chi-square, and Wilcoxon tests.
Results
In total, there were 1664 male patients identified in the data registry who had undergone a robotic inguinal hernia repair with 30-day post-operative follow-up. Of these patients, 65 were identified as having a history of PUPO. After completing 3-to-1 propensity score-matching, 195 matched patients were included in the comparison control group. As expected, there were no significant differences between the PUPO group and the control group when evaluating the matched variables (age, BMI, ASA score, and recent nicotine use) (Table 1). There were also no significant differences between the two groups when comparing history of diabetes mellitus, hypertension, chronic obstructive pulmonary disease, hepatic insufficiency, or immunosuppressant use.
There were no documented intra-operative complications, (including bladder injuries, spermatic cord injuries, or major vascular injuries) in either the PUPO group or the control group. There was also no difference in post-operative complications, 30-day hernia recurrence, readmissions, or wound morbidity (including SSO, SSI, or SSOPI) between the two groups (Table 2).
Discussion
One of the frequent challenges faced by hernia surgeons is the management of groin hernias in patients who have a history of prior pelvic surgery. With an estimated 191,000 new cases of prostate cancer diagnosed each year in the USA; prostatectomy is one of the more common pelvic urologic surgeries [5]. Previous prostatectomy is an important acquired risk factor for the development of primary inguinal hernia [3]. Males who have undergone a radical prostatectomy have nearly a fourfold increase in the need for inguinal hernia repair, with a majority of those hernias occurring within a few years after prostate surgery [6, 7]. Laparoscopic or robotic-assisted prostatectomy carries a 6.7–14.7% rate of post-operative inguinal hernia formation [8,9,10]. Some surgeons have even recommended prophylactic hernia repair be considered at the time of prostatectomy [11, 12]. Given the frequency of prostatectomies, this leads to a large number of patients with a pelvic surgical history who present for inguinal hernia repair.
Although the exact mechanism of hernia formation after prostatectomy is unclear, there is an inseparable relationship between the prostate and the myopectineal orifice [13]. During prostatectomy the retropubic space of Retzius is violated and dissection through this region causes adhesions and scar tissue formation; which can make subsequent entry into this tissue plane much more difficult. Furthermore, the scarred tissue planes may cause bladder adhesions and limit the surgeon’s ability to perform a complete medial inguinal dissection [14], and potentially lead to an increased risk of bladder injury. For these reasons, expert guidelines have generally recommended that surgeons consider an anterior approach when managing these patients [3].
Despite the guidelines, several studies have examined the safety and feasibility of the MIS techniques on patients with a history of PUPO. One single-surgeon case-controlled study found no difference in minor post-operative complications, length of stay, or early recurrence rate when performing a laparoscopic TEP repair on previous prostatectomy patients compared to patients with no surgical history [15]. Dulucq et al. found similar results when examining their single-surgeon experience with TEP after previous lower abdominal surgery [16]. Prassas et al. retrospectively reviewed 301 elective laparoscopic TEP repairs and found there was a higher incidence of post-operative scrotal hematoma in patients with prior lower abdominal surgery, but found no difference in pain or recurrence rate in their 20-month mean follow-up period [17]. The studies evaluating laparoscopic TAPP after prostatectomy have demonstrated similar findings as the TEP studies. Peitsch evaluated their experience with TAPP repair after prior open radical prostatectomy. They had one patient out of 51 who needed a laparoscopic drainage for a hemato-seroma 48 h after the initial operation, but no major vascular or bladder injuries were reported [14]. Other studies evaluating laparoscopic TAPP have also concluded it to be a safe and feasible option for patients with history of radical prostatectomy but do acknowledge its difficulty even for experienced laparoscopic surgeons [18, 19]. One of these studies reported two bladder injuries in their early learning period but reported an overall decrease in morbidity from 9.8 to 1.5% by the second half of the study period, suggesting there is a definite learning curve [18].
To our knowledge, this is one of the first studies to evaluate robotic-assisted inguinal hernia repair in patients with a history of PUPO. Given the conclusions drawn from the previous studies evaluating laparoscopic TAPP, a procedure very similar to that of the robotic approach, it is not surprising that our results showed similar findings. We found no difference in intra-operative or post-operative complications, 30-day recurrence, or readmission rates in this national patient cohort. There were also no documented major vascular, bladder, or spermatic cord injuries. The robotic platform offers surgeons enhanced dexterity and wristed instrumentation which may make dissecting through difficult scarred tissue planes more manageable. The three-dimensional high-definition stabilized image may also improve the surgeon’s ability to identify critical structures to help avoid inadvertent injury. Although we acknowledge the existence of a learning curve for the robotic-assisted approach, some may argue the learning curve is faster than that of the laparoscopic approach to inguinal hernia repair.
There are several limitations to this study. First, the patients were not randomized to receive robotic repair, they were chosen by the surgeon based on patient characteristics and surgeon expertise, which may have excluded particularly complex patients. Second, the AHSQC database relies upon surgeon-entered data with detailed surgical history not always documented with every patient. While we chose to include patients with a history of a urologic pelvic operation, there may be significant heterogeneity within this cohort as we do not have the exact operations performed. In addition, the contributing surgeons to the AHSQC have a particular interest and expertise in the field of hernia surgery; this may skew the dataset to represent more experienced surgeons. Finally, we acknowledge our dataset only offers information on short-term post-operative outcomes (30 days) and further inquiry will be required to gain insight into long-term outcomes such as hernia recurrence.
The open anterior hernia repair remains a safe and viable option for patients with a history of previous pelvic surgery; however, our findings suggest that in an experienced surgeon’s hands, robotic-assisted inguinal hernia repair may be a safe and effective alternative option in patients with prior urologic pelvic surgery who were previously thought to be poor minimally invasive candidates.
References
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Trevisonno M, Kaneva P, Watanabe Y et al (2015) A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia 19:719–724
Group H (2018) International guidelines for groin hernia management. Hernia 22:1–165
Gamagami R, Dickens E, Gonzalez A et al (2018) Open versus robotic-assisted transabdominal preperitoneal (R-TAPP) inguinal hernia repair: a multicenter matched analysis of clinical outcomes. Hernia 22:827–836
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Nilsson H, Stranne J, Stattin P, Nordin P (2014) Incidence of groin hernia repair after radical prostatectomy: a population-based nationwide study. Ann Surg 259:1223–1227
Yamada Y, Fujimura T, Fukuhara H et al (2017) Incidence and risk factors of inguinal hernia after robot-assisted radical prostatectomy. World J Surg Oncol 15:61
Zhu S, Zhang H, Xie L, Chen J, Niu Y (2013) Risk factors and prevention of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol 189:884–890
Iwamoto H, Morizane S, Hikita K, Honda M, Takenaka A (2019) Postoperative inguinal hernia after robotic-assisted radical prostatectomy for prostate cancer: evaluation of risk factors and recommendation of a convenient prophylactic procedure. Cent European J Urol 72:418–424
Majima T, Yoshino Y, Matsukawa Y et al (2018) Causative factors for de novo inguinal hernia after robot-assisted radical prostatectomy. J Robot Surg 12:277–282
Finley DS, Savatta D, Rodriguez E, Kopelan A, Ahlering TE (2008) Transperitoneal robotic-assisted laparoscopic radical prostatectomy and inguinal herniorrhaphy. J Robot Surg 1:269–272
Rogers T, Parra-Davila E, Malcher F et al (2018) Robotic radical prostatectomy with concomitant repair of inguinal hernia: is it safe? J Robot Surg 12:325–330
Miyajima A (2018) Inseparable interaction of the prostate and inguinal hernia. Int J Urol 25:644–648
Peitsch WKJ (2019) Laparoscopic transperitoneal inguinal hernioplasty (TAPP) after radical open retropubic prostatectomy: special features and clinical outcomes. Hernia 23:281–286
Le Page P, Smialkowski A, Morton J, Fenton-Lee D (2013) Totally extraperitoneal inguinal hernia repair in patients previously having prostatectomy is feasible, safe, and effective. Surg Endosc 27:4485–4490
Dulucq JL, Wintringer P, Mahajna A (2006) Totally extraperitoneal (TEP) hernia repair after radical prostatectomy or previous lower abdominal surgery: is it safe? A prospective study. Surg Endosc 20:473–476
Prassas D, Ntolia A, Brosa J et al (2019) Effect of previous lower abdominal surgery on outcomes following totally extraperitoneal (TEP) inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 29:267–270
Wauschkuhn CA, Schwarz J, Bittner R (2009) Laparoscopic transperitoneal inguinal hernia repair (TAPP) after radical prostatectomy: is it safe? Results of prospectively collected data of more than 200 cases. Surg Endosc 23:973–977
Sakon M, Sekino Y, Okada M, Seki H, Munakata Y (2017) Laparoscopic inguinal hernioplasty after robot-assisted laparoscopic radical prostatectomy. Hernia 21:745–748
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Anthony Iacco serves as a proctoring consultant for Intuitive Surgical, Inc. Andrew Angus and Alexander DeMare have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Angus, A., DeMare, A. & Iacco, A. Evaluating outcomes for robotic-assisted inguinal hernia repair in males with prior urologic surgery: a propensity-matched analysis from a national database. Surg Endosc 35, 5310–5314 (2021). https://doi.org/10.1007/s00464-020-08020-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08020-6