Abstract
Background
The robotic platform in pancreatic disease has gained popularity in the hepatobiliary community due to significant advantages it technically offers over conventional open and laparoscopic techniques. Despite promising initial studies, there remains scant literature on operative and oncologic outcomes of robotic pancreaticoduodenectomy (RPD) for pancreatic adenocarcinoma.
Methods
A retrospective review evaluated all RPD performed for pancreatic adenocarcinoma from 2008 to 2019 in a single tertiary institution. RPD cases were matched to open cases (OPD) by demographic and oncologic characteristics and outcomes compared using Mann–Whitney U test, log rank tests, and Kaplan–Meier methods.
Results
Thirty-eight RPD cases were matched to 38 OPD. RPD had significantly higher lymph node (LN) yield (21.5 vs 13.5; p = 0.0036) and no difference in operative time or estimated blood loss (EBL). RPD had significantly lower rate of delayed gastric emptying (DGE) (3% vs 32%; p = 0.0009) but no difference in leaks, infections, hemorrhage, urinary retention ,or ileus. RPD had significantly shorter length of stay (LOS) (7.5 vs. 9; p = 0.0209). There were no differences in 30- or 90-day readmissions or 90-day mortality. There was an equivalent R0 resection rate and LN positivity ratio. There was a trend towards improved median overall survival in RPD (30.4 vs. 23.0 months; p = 0.1105) and longer time to recurrence (402 vs. 284 days; p = 0.7471). OPD had two times the local recurrent rate (16% vs. 8%) but no difference in distant recurrence.
Conclusions
While the feasibility and safety of RPD has been demonstrated, the impact on oncologic outcomes had yet to be investigated. We demonstrate that RPD not only offers similar if not superior immediate post-operative benefit by decreasing DGE but more importantly may offer improved oncologic outcomes. The significantly higher LN yield and decreased inflammatory response demonstrated in robotic surgery may improve overall survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The operative management of oncologic pancreatic disease represents exciting prospects in modern surgery, while simultaneously being one of the most frustrating. The pancreaticoduodenectomy (PD) first garnered attention in American literature in the mid-1930s as a two-stage procedure [1, 2]. It quickly morphed within 5 years to a single-stage procedure that has remained quite similar to its modern incarnation [3]. Subsequent alternations or updates to the original procedure, such as the pylorus-preserving technique, the dunking anastomosis, and the use of novel energy devices, seem to represent variations in surgeon preference rather than real progress [4,5,6,7]. And despite these adaptions, PD remains one of the most complex operations of the alimentary track with sustained high perioperative morbidity and mortality [8, 9].
The technical stagnancy of the PD is made more salient by the progress witnessed in parallel aspects of non-operative patient care. In recent decades, international efforts have led to paradigm and practice- shifting achievements. Advances in critical care have dramatically lowered mortality, improved adjuvant chemotherapy regimens have increased survival after resection, implementation of enhanced recovery pathways have reduced length of stay (LOS) and costs, and employment of interventional radiology techniques have simplified management of complications [3, 10,11,12].
An avenue for potential operative progress and improvement of outcomes is the use of minimally invasive techniques. The laparoscopic PD approach emerged in 1994 as a viable option; however, its widespread application has been significantly limited due to the technical complexity and skill required [13]. It necessitates, among other procedural barriers, meticulous placement of suture needles into minute ductal structures followed by intracorporeal knot tying on delicate and often friable parenchyma. Mastering these operative steps requires quite advanced laparoscopic skills and is characterized by a notoriously steep learning curve [14, 15]. Another minimally invasive platform that is becoming increasingly popular and altering the concept and perception of minimally invasive PD is the robotic approach. Robotic PD (RPD) surgery, by comparison to laparoscopy, offers optical magnification, 3-D depth perception, augmented instrument articulation, and overall greater precision with suture targeting, allowing for a shorter learning curve [16, 17].
Despite RPD coming to the forefront as an attractive and inclusive opportunity for minimally invasive PD, there is still debate over its perioperative benefit. Retrospective studies examining RPD versus open PD (OPD) outcomes have demonstrated equivalent or slightly improved post-operative morbidity with comparable or decreased rates of pancreatic fistula (POPF), decreased delayed gastric emptying (DGE), and decreased LOS [18,19,20,21,22]. Oncologic outcomes demonstrate decreased R1 resections with RPD, equivalent lymph node harvests, and comparable mortality rates [18,19,20]. Despite these promising initial studies, there is, in reality, scant literature on whether RPD operative benefits can positively affect oncologic outcomes. As such, this study seeks to evaluate the long-term oncologic effects of RPD versus OPD for pancreatic ductal adenocarcinoma.
Materials and methods
A retrospective review of all patients who underwent RPD from 2008 to 2019 at a single-center tertiary institution was identified using a prospectively maintained REDCap data repository. Inclusion criteria included adult patients (age ≥ 18 years old) and a pathologic diagnosis of pancreatic ductal adenocarcinoma. Exclusion criteria were conversion to an OPD. Appropriate RPD cases were matched to OPD cases by age, gender, body mass index (BMI), ASA classification, T stage, N stage, use of neoadjuvant chemotherapy, and use of adjuvant chemotherapy. Chart abstraction was used to record demographics, pre-operative characteristics such as T stage, N stage, and use of neoadjuvant chemotherapy, and intra-operative outcomes including EBL, operative time, and lymph node (LN) yield. Data were extracted directly from pathology reports for tumor size, margin status, and lymph node positivity ratio. Immediate post-operative complications were recorded including abscess, ileus, anastomotic leak, hemorrhage, DGE, POPF, urinary retention, and wound infection. Long term outcomes were documented including 30- and 90-day readmission, and adjuvant chemotherapy use. Evidence of recurrence, recurrence pattern, mortality, and last follow-up were recorded up until September 2019.
Outcomes defined as continuous variables were reported as median (range) within groups and student t tests and Mann–Whitney U tests of comparison were used to compare normally distributed variables between groups. Outcomes defined as categorical variables were reported as number (%) within groups. A chi-squared tests were employed to compare distribution between groups. Survival and recurrence were compared between RPD and OPD using log rank tests and Kaplan–Meier methods. A p value of ≤ 0.05 was considered statistically significant. This project was approved by the institutional review board and written consent was not required.
Patient selection
Carolinas Medical Center (CMC) is a 1000-bed tertiary referral center with four fellowship trained hepatobiliary surgeons who perform over 120 PD cases per year. There is a random referral process through gastroenterology and oncology with cases evenly referred of which only two of the four surgeons offer RPD. Unlike other high-volume centers where all cases may be reviewed for an RPD approach, the internal dynamics of CMC’s referral process and individual RVU productivity model prevent a similar systematic process. Therefore, regardless of complexity or perceived case difficulty, there is no methodical or concerted effort, implicit or otherwise, to streamline easier cases into the RPD pathway.
Results
Demographic and pre-operative characteristics
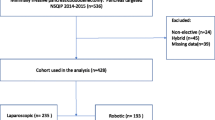
Ninety-four RPD cases were identified from a prospectively maintained data repository. Sixteen cases were converted to open and excluded; of these, nine cases were for pancreatic adenocarcinoma. Of the remaining RPD cases, only 38 cases were operated on for pancreatic adenocarcinoma and, thus, included in the analysis. These 38 RPD cases were matched to 38 OPD cases by age, gender, body mass index (BMI), ASA classification, pathologic T stage, pathologic N stage, use of neoadjuvant chemotherapy, and use of adjuvant chemotherapy (Table 1). The majority of patients were female (58%) and the median age was between 66 and 68 years old (range 38–84 years old). Most patients were ASA classification III and had a BMI in the mid-20 s. Less than a quarter of each cohort had neoadjuvant chemotherapy (18% OPD; 16% RPD) and 68% of both cohorts underwent adjuvant chemotherapy.
Perioperative outcomes
There was no significant difference in operative time between OPD and RPD (RPD: 392 min vs. OPD: 350; p = 0.1077) (Table 1). There was no significant difference in EBL between cohorts (RPD: 300 mL vs. OPD: 550; p = 0.0693). The LN yield was significantly higher in RPD cases, yielding a median of 21.5 nodes versus 13.5 nodes in OPD (p = 0.0036). There were equivalent rates of post-operative bleed requiring transfusion in both cohorts (11%). There were additionally comparable rates of ileus, urinary retention, anastomotic leak, POPF, and wound infection. There was a significantly higher incidence of DGE in the OPD of nearly 30% (RPD: 3% vs. OPD: 32%; p = 0.0009) and a significantly shorter LOS in the RPD cohort by about 1.5 days (RPD: 7.5 days vs. OPD: 9 days; p = 0.0209). Thirty and 60-day readmission rates were not significantly different with both cohorts having a 6% 30-day readmission rate and a 11–12% 90-day readmission rate. Ninety-day mortality was comparable with only two patients from the OPD having a 90-day mortality and only one from the RPD cohort (p = 0.5558).
Oncologic outcomes
As cohorts were matched by T stage, the pathologic tumor size was ultimately similar between cohorts (RPD: 30 mm vs. OPD: 29 mm; p = 0.8233) (Table 2). The grade of differentiation varied slightly between cohorts; there were significantly more moderately differentiated tumors in the RPD cohort (RPD: 66% vs. OPD: 39%; p = 0.0205) and significantly more poorly differentiated tumors in the OPD cohort (RPD: 24% vs. OPD: 47%; p = 0.0340). There was no difference in the amount of well differentiated tumors. The RPD cohort additionally had significantly more tumors with lymphovascular invasion (RPD: 71% vs. OPD: 47%; p = 0.0477) and perineural invasion (RPD: 89% vs. OPD: 51%; p = 0.0003). There was an equivalent R1 resection rate of mid 40% in both cohorts (p = 0.8170). There were no differences in LN positivity ration between cohorts. The RPD cohort had a longer median overall survival although this was not statistically significant (RPD: 30.4 vs. OPD: 23.0 months; p = 0.1105). There was also no statistical difference in time to recurrence (RPD: 402 vs. OPD: 284 days; p = 0.7471); open cases had two times the local recurrence rate (RPD: 8% vs. OPD: 16%; p = 0.2870). There was no difference in distant recurrence rates (RPD: 32% vs. OPD: 37%; p = 0.6287).
Discussion
While the feasibility and safety of RPD has been well demonstrated, the impact on oncologic outcomes has yet to be thoroughly investigated. This study demonstrates that RPD offers similar, if not superior, immediate intra-operative and post-operative benefits but more importantly may offer improved oncologic outcomes. The significantly higher LN yield and decreased inflammatory response of robotic surgery may increase time to recurrence and improve overall survival in pancreatic ductal adenocarcinoma.
Even with the literature showing equivalent if not better results with minimally invasive PD, it is still far from widespread acceptance. In a recent survey of six international associations for hepatobiliary surgery, less than one-third of surgeons said they would attempt minimally invasive PD and only 10% considered it superior to its open counterpart [23]. And although data exist that suggest inferiority when attempted at low-volume institutions; in experienced hands, minimally invasive PD is prudent and offers comparative advantages [24]. A large series of laparoscopic PD demonstrated safety and adherence to oncologic principles and a retrospective meta-analysis of over 700 RPD cases demonstrated perioperative outcomes consistent with historical open standards [25, 26]. These outcomes have been verified by other cohort studies demonstrating decreased EBL and LOS [19, 27, 28].
This retrospective propensity-matched analysis contributes substantially to the current literature by demonstrating the equivalence to OPD as well as the benefits of RPD on patient outcomes. Our RPD median operative time of 392 min was not significantly different from OPD (Table 1). It remains on the lower end for reported RPD with most high-volume centers citing times between 444 and 718 min [29]. The longer operative times demonstrated by other studies may be secondary to the extra setup and docking required or a lack of experience that may continue to improve with advances in the learning curve [30]. Our median EBL for RPD of 300 cc is also well within range of reported averages and lower than our OPD EBL. This may be attributed to the amplified view of smaller vessels, specifically when dissecting out the superior mesenteric artery and vein from the uncinate process [18, 20, 21]. The post-operative morbidity of RPD was mostly equivalent to OPD with comparable rates of ileus, urinary retention, anastomotic leak, and wound infection. POPF rates were also similar, irrespective of approach. Further, there were no differences in readmission rates (30- or 90-day) or in 90-day mortality between cohorts.
There was a significant decrease in DGE in the RPD cohort of nearly 30% (Table 1). DGE while not life-threatening does have substantial clinical consequences including prolonged LOS, higher costs, readmission, overall discomfort, requirement of feeding tube, and delays in starting adjuvant therapies [31, 32]. Although there has been considerable study on primary DGE pathogenesis, it remains poorly understood. There are negative associations demonstrated with increased intra-abdominal inflammation while robotic-sutured anastomoses decrease DGE incidence when compared with open stapled anastomoses [33, 34]. Our results further endorse the theory that DGE is influenced by intra-abdominal inflammation. As robotic techniques reduce invasive manipulation including skin incision size and tissue handling technique, there is a decreased subsequent inflammatory stress response brought about by such surgical trauma [35, 36]. Of note, as our OPD gastrojejenal anastomoses are done in a hand-sewn manner, we can extrapolate that perhaps the decreased disturbance in hemostasis and blunted immune response resulting in decreased inflammation in RPD cases is lessening post-operative DGE. Further study is clearly required as this is a speculative conclusion.
Our analysis demonstrates a trend towards improved long-term oncologic outcomes with RPD which has yet to be investigated in the literature. There was a significantly higher LN yield in RPD cases of 21.5 nodes vs. 13.5 nodes in OPD (Table 2). LN harvest plays a strong prognostic role in pancreatic ductal adenocarcinoma with multiple studies showing that survival is independently predicted by total LN harvest [37,38,39,40]. Similar relationships have also been shown in ampullary adenocarcinoma [41]. Our study demonstrated a trend towards decreased recurrence rates in the RPD cohort, with a difference of nearly 15% (RPD: 53% vs. OPD: 39%). When recurrence pattern was assessed, the local recurrence rate was twice as high in OPD cases (OPD: 16% vs. RPD: 8%) which may be explained by an inferior LN harvest and examination [42, 43]. Further, the median overall survival for RPD cases was over 7 months longer than OPD cases. Although this was not statistically significant, a type II error may be present due to the small sample size.
While robotic surgery may offer advantages, a constant concern across surgical fields is its financial impact and whether cost may be prohibitive. A study out of Italy demonstrated a significantly increased operative cost for robotic pancreatectomies when compared to open cases [44]. However, when total hospital costs, which include LOS and readmission, are investigated, there is no difference in cost between robotic and open surgery [18, 45,46,47]. Of note, anecdotally there is a tendency for high-volume centers to routinely begin OPD cases with diagnostic laparoscopy. Incorporating the cost of even a brief laparoscopic evaluation may presumably further close the intra-operative cost gap between OPD and RPD. Ultimately, there appears to be a need for more comparative cost analyses before definitive conclusions can be extrapolated [48]. Our center is currently investigating our costs between RPD and OPD and will be presenting the data shortly.
A key criticism and limitation of this study includes patient selection bias. The decision to employ a minimally invasive approach remains highly selective and, even at high-volume centers, is rarely protocolized. As mentioned, regardless of difficulty, there is no effort to direct uncomplicated cases to the RPD pathway. Referrals are random to each of the hepatobiliary surgeons with only half performing RPD. Further, we matched the RPD patients to OPD counterparts by demographic and oncologic characteristics; however, this is not infallible or equivalent to a randomized prospective approach. For instance, we were unable to match for grade of differentiation. With the OPD cohort having more patients with grade 3 differentiation, they may in fact have a population with worse biologic disease. Fortunately, there are active randomized prospective studies comparing RPD and OPD forthcoming [49]. Finally, this is a very small sample size of only 38 patients per group. The risk of a type II error is high and thus, trends and non-significant results demonstrated in this manuscript may in fact be significant when a larger cohort is compared.
Conclusion
This propensity-matched retrospective cohort trial demonstrates that RPD is a safe and comparable alternative to OPD. Further, it may offer both post-operative and oncologic benefit by decreasing rates of DGE and improving LN harvest, which may affect recurrence and overall survival rates. As such, RPD can be an effective addition to the armamentarium of a modern hepatobiliary surgeon.
References
Whipple AO, Parsons WB, Mullins CR (1935) Treatment of carcinoma of the ampulla of Vater. Ann Surg 102(4):763–779
Schnelldorfer T, Sarr MG (2009) Alessandro Codivilla and the first pancreatoduodenectomy. Arch Surg 144(12):1179–1184
Fernandez-del Castillo C et al (2012) Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery 152(3 Suppl 1):S56–63
Senda Y et al (2018) Randomized clinical trial of duct-to-mucosa versus invagination pancreaticojejunostomy after pancreatoduodenectomy. Br J Surg 105(1):48–57
Kennedy EP, Yeo CJ (2011) Dunking pancreaticojejunostomy versus duct-to-mucosa anastomosis. J Hepatobiliary Pancreat Sci 18(6):769–774
Diener MK et al (2017) Partial pancreatoduodenectomy versus duodenum-preserving pancreatic head resection in chronic pancreatitis: the multicentre, randomised, controlled, double-blind ChroPac trial. Lancet 390(10099):1027–1037
Keck T et al (2016) Pancreatogastrostomy versus pancreatojejunostomy for RECOnstruction after PANCreatoduodenectomy (RECOPANC, DRKS 00000767): perioperative and long-term results of a multicenter randomized controlled trial. Ann Surg 263(3):440–449
Winter JM et al (2006) 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10(9):1199–1210 discussion 1210-1
Newhook TE et al (2015) Morbidity and mortality of pancreaticoduodenectomy for benign and premalignant pancreatic neoplasms. J Gastrointest Surg 19(6):1072–1077
Neoptolemos JP et al (2017) Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet 389(10073):1011–1024
Takagi K et al (2019) Effect of an enhanced recovery after surgery protocol in patients undergoing pancreaticoduodenectomy: a randomized controlled trial. Clin Nutr 38(1):174–181
Sohn TA et al (2003) Pancreaticoduodenectomy: role of interventional radiologists in managing patients and complications. J Gastrointest Surg 7(2):209–219
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410
Patel B et al (2018) Laparoscopic pancreaticoduodenectomy in Brisbane, Australia: an initial experience. ANZ J Surg 88(5):E440–e444
Wang M et al (2016) Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg 20(5):924–935
Bodner J et al (2005) The da Vinci robotic system for general surgical applications: a critical interim appraisal. Swiss Med Wkly 135(45–46):674–678
Shyr BU et al (2018) Learning curves for robotic pancreatic surgery-from distal pancreatectomy to pancreaticoduodenectomy. Medicine (Baltimore) 97(45):e13000
Baker EH et al (2015) Robotic pancreaticoduodenectomy for pancreatic adenocarcinoma: role in 2014 and beyond. J Gastrointest Oncol 6(4):396–405
Chen S et al (2015) Robot-assisted laparoscopic versus open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc 29(12):3698–3711
Lai EC, Yang GP, Tang CN (2012) Robot-assisted laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy—a comparative study. Int J Surg 10(9):475–479
Zhou NX et al (2011) Outcomes of pancreatoduodenectomy with robotic surgery versus open surgery. Int J Med Robot 7(2):131–137
Boggi U et al (2016) Robotic-assisted pancreatic resections. World J Surg 40(10):2497–2506
van Hilst J et al (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 19(3):190–204
de Rooij T et al (2016) Minimally invasive versus open pancreatoduodenectomy: systematic review and meta-analysis of comparative cohort and registry studies. Ann Surg 264(2):257–267
Wang M et al (2015) Laparoscopic pancreaticoduodenectomy: single-surgeon experience. Surg Endosc 29(12):3783–3794
Kornaropoulos M et al (2017) Total robotic pancreaticoduodenectomy: a systematic review of the literature. Surg Endosc 31(11):4382–4392
Bao PQ, Mazirka PO, Watkins KT (2014) Retrospective comparison of robot-assisted minimally invasive versus open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg 18(4):682–689
Chalikonda S, Aguilar-Saavedra JR, Walsh RM (2012) Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc 26(9):2397–2402
Dai R, Turley RS, Blazer DG (2016) Contemporary review of minimally invasive pancreaticoduodenectomy. World J Gastrointest Surg 8(12):784–791
Napoli N et al (2016) The learning curve in robotic pancreaticoduodenectomy. Dig Surg 33(4):299–307
Ahmad SA et al (2012) Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg 256(3):529–537
Marsh Rde W et al (2015) Pancreatic cancer and FOLFIRINOX: a new era and new questions. Cancer Med 4(6):853–863
Park YC et al (2003) Factors influencing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Am Coll Surg 196(6):859–865
Jung JP et al (2018) Use of video review to investigate technical factors that may be associated with delayed gastric emptying after pancreaticoduodenectomy. JAMA Surg 153(10):918–927
Zawadzki M et al (2017) Comparison of inflammatory responses following robotic and open colorectal surgery: a prospective study. Int J Colorectal Dis 32(3):399–407
Shibata J et al (2015) Surgical stress response after colorectal resection: a comparison of robotic, laparoscopic, and open surgery. Tech Coloproctol 19(5):275–280
Basturk O et al (2015) Substaging of lymph node status in resected pancreatic ductal adenocarcinoma has strong prognostic correlations: proposal for a revised N classification for TNM staging. Ann Surg Oncol 22(Suppl 3):S1187–S1195
Strobel O et al (2015) Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg 261(5):961–969
La Torre M et al (2014) Prognostic assessment of different lymph node staging methods for pancreatic cancer with R0 resection: pN staging, lymph node ratio, log odds of positive lymph nodes. Pancreatology 14(4):289–294
Showalter TN et al (2011) The influence of total nodes examined, number of positive nodes, and lymph node ratio on survival after surgical resection and adjuvant chemoradiation for pancreatic cancer: a secondary analysis of RTOG 9704. Int J Radiat Oncol Biol Phys 81(5):1328–1335
Chen SC et al (2015) The role of lymph nodes in predicting the prognosis of ampullary carcinoma after curative resection. World J Surg Oncol 13:224
Tsai HL et al (2007) The prognostic significance of total lymph node harvest in patients with T2–4N0M0 colorectal cancer. J Gastrointest Surg 11(5):660–665
Lee SR et al (2014) Lymph node ratio predicts local recurrence for periampullary tumours. ANZ J Surg 84(5):353–358
Boggi U et al (2013) Feasibility of robotic pancreaticoduodenectomy. Br J Surg 100(7):917–925
Cunningham KE et al (2016) A policy of omitting an intensive care unit stay after robotic pancreaticoduodenectomy is safe and cost-effective. J Surg Res 204(1):8–14
Barbash GI, Glied SA (2010) New technology and health care costs—the case of robot-assisted surgery. N Engl J Med 363(8):701–704
Mesleh MG et al (2013) Cost analysis of open and laparoscopic pancreaticoduodenectomy: a single institution comparison. Surg Endosc 27(12):4518–4523
Del Chiaro M, Segersvard R (2014) The state of the art of robotic pancreatectomy. Biomed Res Int 2014:920492
de Rooij T et al (2018) Minimally invasive versus open pancreatoduodenectomy (LEOPARD-2): study protocol for a randomized controlled trial. Trials 19(1):1
Funding
No external funding source was used to conduct this study. All authors had complete access to the data that support the publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. John Martinie serves as a proctor, course director, and speaker for Intuitive Surgical, Medtronic, and Ethicon. Drs. Maria Baimas-George, Michael Watson, Keith J Murphy, David Iannitti, Erin Baker, Lee Ocuin, and Dionisios Vrochides have no conflicts of interests of financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baimas-George, M., Watson, M., Murphy, K.J. et al. Robotic pancreaticoduodenectomy may offer improved oncologic outcomes over open surgery: a propensity-matched single-institution study. Surg Endosc 34, 3644–3649 (2020). https://doi.org/10.1007/s00464-020-07564-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07564-x