Abstract
Background
Minimally invasive surgery, such as laparoscopic adrenalectomy and robotic adrenalectomy, has become a treatment of choice for benign adrenal tumors. Efforts are ongoing to minimize the invasiveness of the procedure and to reduce the number of port sites. The primary endpoint of this study was the safety and feasibility of a reduced-port site technique for robotic posterior retroperitoneal adrenalectomy (RPRA).
Methods
This study retrospectively analyzed 74 RPRAs performed by a single surgeon, including 30 conventional three-port site early-phase RPRAs, 30 three-port site late-phase RPRAs, and 14 reduced-port site RPRAs. Reduced-port site RRPA was defined as using two port sites: one for a multi-glove port and one for an additional side port. The clinicopathological features and surgical outcomes were compared in these three groups.
Results
No major complications were observed following RPRA in the three groups of patients. Operation time, pain score, and hospital stay did not differ significantly among these three groups.
Conclusions
RPRA using a reduced-port site system was safe and feasible and may be a good alternative to conventional three-port site RPRA for benign adrenal tumors in certain situations.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Laparoscopic adrenalectomy has become a standard surgical treatment option for patients with benign adrenal diseases, with transperitoneal laparoscopic adrenalectomy being the most frequent type of minimally invasive surgical technique [1, 2]. Alternative approaches, such as lateral retroperitoneal adrenalectomy and posterior retroperitoneal adrenalectomy (PRA), were developed to eliminate the need for mobilization of adjacent structures, including the intestines, spleen, and liver, and to reduce the risk of laparoscopic associated complications [2,3,4]. PRA has shown benefits over the transperitoneal approach, including fewer complications, less pain, and shorter operation time and hospitalization [5]. Robotic PRA (RPRA) may achieve better outcomes in certain situations, especially in PRA for patients with limited working space [6, 7].
Minimally invasive surgical techniques, such as laparoscopic and robotic procedures, may be further modified by reducing the number of port sites [8]. In a single-site system, for example, most of the instruments required for surgery are introduced via a single port [9]. A single-site robotic system with magnified camera views, instrument articulation, and rotation motion was shown to be feasible when performed by experienced surgeons [9, 10]. However, this single-site system has drawbacks in that placing every instrument through a single port site requires the devices to be curved and requires the switching of right and left positions to the opposite sites. These conditions limit right and left arm movements and result in collisions between instruments.
This study attempted to reduce the actual number of port sites on the patients while maximizing the number of robot arms and assistant devices to increase the quality of surgical procedures while maintaining safety equal to that of conventional adrenalectomy using three or more port sites. The primary endpoint was the safety and feasibility of the reduced-port site technique for RPRA.
Materials and methods
Study design
This retrospective study was designed to assess the safety and feasibility of reduced-port site RPRA performed by a single experienced surgeon. Reduced-port site surgery is defined as surgery that uses two port sites, a multi-glove port, and an additional side port. This study was approved by the Institutional Review Board of the Asan Medical Center (2018-1454).
In the first step, the paraspinous port incision was omitted to reduce complications related to back muscle and nerve injury. Animal experiments were performed, omitting the paraspinous port incision and making incisions only for two port sites. This technique was subsequently applied to patients. We used DaVinci Xi robotic system for RPRA in all cases. To analyze the feasibility of the new technique, patients who underwent RPRA were subdivided into three different phases according to the time of surgery: (1) conventional three-port site early-phase, (2) conventional three-port site late-phase, and (3) reduced-port (two-port) site. Early-phase was defined as the first series of patients who underwent RPRA using the conventional three-port site method prior to overcoming the personal learning curve; late-phase was defined as the last series of patients who underwent RPRA using the conventional three-port site method just prior to introducing the new reduced-port site method; and reduced-port site was defined as consecutive patients who underwent RPRA using two port sites.
Clinicopathological features of the three sets of patients were recorded, including age at operation, gender, height, weight, body mass index (BMI), and length of hospital stay. Other variables that were recorded included the type of disease, the size and site of the adrenal tumor, the mean operation time, and the numeric rating scale (NRS) pain score. These factors were compared in the three patient groups.
Patient population
From January 2016 to December 2018, 410 patients underwent adrenalectomy in our institution, including 12 who underwent open adrenalectomy, 18 who underwent laparoscopic transperitoneal adrenalectomy (LTA), and 380 who underwent PRA. For this study, the patients in PRA group with malignant tumors, such as adrenocortical carcinomas and malignant pheochromocytomas, and those with metastatic adrenal lesions from other primary carcinomas (n = 30) and laparoscopic PRA patients (n = 240) were excluded. Of the 110 patients who underwent robotic adrenalectomy for benign adrenal disease, 74 underwent RPRA for adrenal tumors < 6 cm in diameter and were enrolled in this study. These included the first 30 consecutive patients who underwent RPRA using the conventional three-port site method (early-phase), the last 30 patients who underwent RPRA using the conventional three-port site method (late-phase), and the 14 patients who underwent RPRA using the two-port site method (Fig. 1).
Surgical techniques
The conventional three-port site technique RPRA consisted of making a 1.5-cm incision at the end of the tip of the twelfth rib and a 1.0-cm incision at the end of the tip of the eleventh rib, at least 1.0 cm apart from the tip to avoid the subcostal nerve injuries. A third incision for the third port, about 1.0 cm in size, was made lateral to the paraspinous muscles in alignment with the first port site. A camera arm was inserted into the port site at the twelfth rib, and two robot arms with rigid grasping instruments and acting energy devices were inserted into the two other side ports.
Reduced-port site RPRA consisted of making a 2.0-cm incision at the end of the tip of the twelfth rib and a 1.0-cm incision at the end of the tip of the eleventh rib, at least 1.0 cm apart from the tip. The port site at the twelfth rib consisted of a multi-glove port (GLOVE port, Nelis Medical, bucheon-si/South Korea), containing a rigid robot camera arm, a rigid robot instrument arm, and an assistant instrument, for example, suction and irrigation. Another rigid robot arm was inserted into the port site at the eleventh rib place. The curved devices made for single-site port surgery were not used for the multi-glove port site. Rather, rigid instruments made for conventional three-port site robotic surgery were used. The retroperitoneal space was insufflated with CO2 at a rate of 4–6 L per minute to a pressure of 12–15 mmHg.
Indications and patient selection for RPRA
The selection of a conventional open or laparoscopic approach was based on each individual patient’s characteristics and on the anatomic and pathological features of the adrenal gland tumors. The indications for robotic PRA were similar to those for the laparoscopic approach. In addition to known indications for minimally invasive adrenalectomy, patient selection was based on body habitus and intra-abdominal adhesions, according to National Institutes of Health(NIH) and American Association of Endocrine Surgeons(AAES)/American Association of Clinical Endocrinologists(AACE) guidelines [11]. In general, patients were selected for PRA if their adrenal tumors were benign and less than 6 cm in size and if they were not expected to have significant retroperitoneal adhesions due to kidney surgery. Other indications for PRA included a short distance between the skin and Gerota’s space (generally < 7 cm) and positioning of the twelfth rib rostral to the renal hilum [12, 13].
Animal experiments assessing reduced-port site RPRA
Swine weighing ~ 20–25 kg were maintained according to the rules for animal studies of the Asan Institute for Life Science. Anesthesia was induced with propofol. After endotracheal intubation, anesthesia was maintained with halothane. The pigs were placed in the prone position. The reduced-port site approach was introduced. The kidney and adrenal gland were mobilized, and the adrenal gland was removed. Four consecutive RPRAs using two port sites were successfully performed in two pigs (Fig. 2). There were no troublesome collisions between the rigid robot instruments at the multi-glove port site, and the robot arms were manipulated comfortably throughout these procedures.
Patient positioning and port sites for reduced-port site RPRA
Incision of about 2.0 cm in length was made at the end of the tip of the twelfth rib and a 1.0-cm incision at the end of the tip of the eleventh rib. In this technique, the incision near the paraspinous muscles was omitted (Fig. 3).
Postoperative management
Postoperative pain control consisted of routine administration of oral non-steroidal anti-inflammatory drugs (NSAIDs) (acetaminophen plus tramadol hcl 325/37.5 mg) twice daily, with intravenous narcotic (ketorolac tromethamine 30 mg) administered intermittently at the request of the patient on operative day and postoperative day 1 when the NRS pain score is 4 or higher. Postoperative pain was assessed using a NRS (with scores ranging from 0 to 10), 30 min after surgery in the post-anesthesia care unit (PACU), and 4, 8, 12, 16, 24, 32, 40, and 48 h after surgery. No morbidities were recorded and patients were generally discharged on postoperative day 2, except for patients with Cushing’s syndrome. Cushing’s syndrome patients were generally discharged on postoperative day 3 for intravenous hydrocortisone steroid supplementation. Oral diet was resumed 3 h after adrenal surgery. Postoperative morbidity and mortality were assessed at 2 weeks in the out-patient clinic.
Statistical analysis
Continuous variables are reported as mean ± standard deviation with ranges and compared by ANOVA tests. Categorical variables are reported as absolute numbers and percentages, and compared by the χ2 test or Fisher’s exact test, as appropriate. Relationships between phase and duration of surgery are analyzed by scatter plots with Pearson’s correlation coefficients and illustrated as box plots. All statistical analyses were performed using SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL), with p values < 0.05 considered statistically significant.
Results
The clinicopathological characteristics of the 74 patients are shown in Table 1. There were no differences in age, gender, height, weight, BMI, types of disease, or sizes and sites of adrenal tumors among the three groups. There was a difference in hospital stays, mean operation time, and NRS pain score with significance (p < 0.05). Hospital stay was significantly longer (p < 0.05) for patients who underwent conventional three-port site early-phase RPRA than for the other groups, and mean operation time gradually decreased over time from early-phase three-port to late-phase three-port to two-port surgery. NRS pain score on the first postoperative day was significantly lower (p < 0.05) for patients who underwent reduced-port site RPRA than for the other two groups. Patients in the reduced-port group showed far greater scar satisfaction than patients in the three-port groups. None of the patients who underwent two-port site RPRA reported numbness of the lateral abdominal trunk and thigh during the hospital stay and thereafter. With the patients in the conventional three-port site group, 8 patients (13.3%) complained of numbness at operated site trunk and/or thigh from the first day of surgery. However, the numbness decreased gradually during the hospital stay and all of them were relieved before the first day of follow-up visit. None of the patients in any of the three groups experienced any intraoperative or postoperative complications, and none required conversion to open surgery.
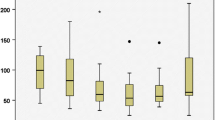
Because operation time differed significantly among the three groups, operation time was evaluated with box plots to compare their patterns (Fig. 4). For comparison, outliers in operation time among patients who underwent conventional three-port site early-phase and late-phase RPRA were assessed in separate plots. None of the patients who underwent reduced-port site RPRA were an outlier in operation time. Mean operation time was significantly longer for patients who underwent conventional early-phase three-port RPRA than for those who underwent late-phase three-port RPRA (128 vs. 102 min, p = 0.032), but operation times for reduced-port RPRA did not differ from those for early-phase (p = 0.06) and late-phase (p = 0.963) three-port RPRA.
Scatter plot evaluation showed that for the first 30 patients who underwent conventional three-port RPRA, the operation time ranged from 67 to 260 min and decreased as the number of patients increased (Fig. 5). Operation time for the last 30 patients who underwent conventional three-port RPRA ranged from 50 to 205 min, plateauing near 100 min. In comparison, operation time for the 14 patients who underwent two-port RPRA ranged from 61 to 147 min and decreased as the number of patients increased.
Discussion
Laparoscopic adrenalectomy is regarded as the treatment of choice for benign adrenal tumors [14,15,16]. Safety may be enhanced by reducing the invasiveness of the procedure by, for example, reducing the number of ports and the length of incisions. Reduced-port adrenalectomy has been reported to reduce postoperative pain and administration of analgesics [17,18,19]. Although advances in single-site surgery have enabled reduced-port surgery, single-site PRA has several drawbacks compared with multiport PRA, including collisions between instruments and unfamiliar movements of instruments lengthening operation time [20]. Moreover, surgical outcomes, including complication rates and operation times, were poorer using a single-port than using a conventional multiport approach [9, 20,21,22,23].
The present study showed that reduced-port site RPRA would result in less pain than conventional three-port site RPRA, with the two types of surgery having similar operation times. Theoretically, reducing the number of ports that are required in minimally invasive surgery for adrenal disease would further minimize the invasiveness of the procedure. The present study found that pain on postoperative day 1 and the duration and dose of analgesics were significantly lower for patients who underwent reduced-port site RPRA than for those who underwent conventional three-port site RPRA (p < 0.05). Although the surgeon who performed these operations had experience in laparoscopic PRA, a learning curve was required for RPRA. However, after short-term experience with three-port conventional RPRA, the learning curve of reduced-port RPRA was not long.
The need for minimizing the invasiveness of multiple port sites associated with laparoscopic or robotic procedures, a single-port surgery was developed, allowing a majority of the instruments required for surgery to be introduced through a single port [9, 17, 19, 20, 22, 24]. A systematic review and meta-analysis of nine studies of laparoendoscopic single-site (LESS) adrenalectomy through a rectoscope tube [20], first reported in 2005 [24], found that operation time was longer, postoperative hospital stay was shorter, and NRS pain scores were lower in all nine studies [20]. Although many patients have undergone LESS adrenalectomy, the number of patients has tended to decrease over time [22]. Our study found that NRS pain score was lower for patients who underwent reduced-port site RPRA than for those who underwent conventional three-port site RPRA.
Learning curves for laparoscopic single-site adrenalectomy were found to be affected by collision between instruments, as surgical space is limited by tumor size and obesity. Improvements in crossover technique occurring after 30 operations may reduce the difficulty of LESS adrenalectomy [25]. This study found that the learning curve was shorter for reduced-port site RPRA than for conventional three-port site RPRA. Surgeons who are able to manipulate the robotic system can better avoid collisions and so are able to focus more comfortably on the RPRA procedures.
Although reducing the number of port sites can reduce postoperative pain, reduced-port site RPRA should yield a quality of surgical outcome similar to or better than that of conventional three-port site RPRA. Therefore, rigid robot arms, rather than curved single-site instruments, were used at the multi-glove port site. This procedure enabled comfortable endo-wrist articulation while using three to four robotic arms with at least one additional assistant instrument. Reduced-port site RPRA was able to utilize the extra port within the multi-glove port site for suction, irrigation, and counter-retraction. The patient’s scar satisfaction and numbness around the incision area were also far better with two port sites than it was with three port sites. None of the patients who underwent two-port site RPRA experienced numbness at the lateral abdominal trunk or thigh.
To our knowledge, this is the first report to describe a new technique of two-port site RPRA using a multi-glove port and rigid robot arms. This study showed that this reduced-port site RPRA method can be performed safely with reasonable operation times and less pain. All patients were discharged uneventfully. Thus, reduced-port site RPRA was as safe and feasible as conventional three-port site RPRA.
The present study had several limitations. First, it was a retrospective study involving a small number of patients who underwent surgery at a single center. Thus, patient selection biases were unavoidable. In addition, the surgical indications for reduced-port site RPRA were dependent on the policies of a single, albeit experienced, surgeon, suggesting the need for other surgeons to validate the reduced-port site technique.
Conclusion
This study described an RPRA technique involving a reduction in the number of actual port sites while maximizing the acting number of robot arms. This method maintained the quality of surgical procedures, with outcomes similar to those of conventional three-arm RPRA. This reduced-port site method may be an alternative to conventional three-port site RPRA for removing benign adrenal tumors in certain situations. Future comparative studies are needed to confirm the consistency and efficacy of this procedure.
References
Dudley NE, Harrison BJ (1999) Comparison of open posterior versus transperitoneal laparoscopic adrenalectomy. Br J Surg 86:656–660
Liao CH, Chen J, Chueh SC, Tu YP, Chen SC, Yuan RH (2001) Effectiveness of transperitoneal and trans-retroperitoneal laparoscopic adrenalectomy versus open adrenalectomy. J Formos Med Assoc 100:186–191
Berber E, Tellioglu G, Harvey A, Mitchell J, Milas M, Siperstein A (2009) Comparison of laparoscopic transabdominal lateral versus posterior retroperitoneal adrenalectomy. Surgery 146(4):621–625
Fernandez-Cruz L, Saenz A, Taura P, Benarroch G, Astudillo E, Sabater L (1999) Retroperitoneal approach in laparoscopic adrenalectomy: is it advantageous? Surg Endosc 13:86–90
Lairmore TC, Folek J, Govednik CM, Snyder SK (2016) Improving minimally invasive adrenalectomy: selection of optimal approach and comparison of outcomes. World J Surg 40:1625–1631
Okoh AK, Yigitbas H, Berber E (2015) Robotic posterior retroperitoneal adrenalectomy. J Surg Oncol 112:302–304
Samreen S, Fluck M, Hunsinger M, Wild J, Shabahang M, Blansfield JA (2019) Laparoscopic versus robotic adrenalectomy: a review of the national inpatient sample. J Robot Surg 13:69–75
Brunaud L, Bresler L, Ayav A, Zarnegar R, Raphoz AL, Levan T, Weryha G, Boissel P (2008) Robotic-assisted adrenalectomy: what advantages compared to lateral transperitoneal laparoscopic adrenalectomy? Am J Surg 195:433–438
Arghami A, Dy BM, Bingener J, Osborn J, Richards ML (2015) Single-port robotic-assisted adrenalectomy: feasibility, safety, and cost-effectiveness. JSLS 19(e2014):00218
Lee S, Kim JK, Kim YN, Jang DS, Kim YM, Son T, Hyung WJ, Kim HI (2017) Safety and feasibility of reduced-port robotic distal gastrectomy for gastric cancer: a phase I/II clinical trial. Surg Endosc 31:4002–4009
Zeiger MA, Thompson GB, Duh QY, Hamrahian AH, Angelos P, Elaraj D, Fishman E, Kharlip J, American Association of Clinical Endocrinologists, American Association of Endocrine Surgeons (2009) American association of clinical endocrinologists and american association of endocrine surgeons medical guidelines for the management of adrenal incidentalomas: executive summary of recommendations. Endocr Pract 15:450–453
Taskin HE, Berber E (2012) Robotic adrenalectomy. J Surg Oncol 106:622–625
Okoh AK, Berber E (2015) Laparoscopic and robotic adrenal surgery: transperitoneal approach. Gland Surg 4:435–441
Jacobs JK, Goldstein RE, Geer RJ (1997) Laparoscopic adrenalectomy. A new standard of care. Ann Surg 225(5):495–501
Smith CD, Weber CJ, Amerson JR (1999) Laparoscopic adrenalectomy: new gold standard. World J Surg 23:389–396
Coste T, Caiazzo R, Torres F, Vantyghem MC, Carnaille B, Do Cao C, Douillard C, Pattou F (2017) Laparoscopic adrenalectomy by transabdominal lateral approach: 20 years of experience. Surg Endosc 31:2743–2751
Wu S, Lai H, Zhao J, Chen J, Mo X, Zuo H, Lin Y (2016) Laparoendoscopic single-site adrenalectomy versus conventional laparoscopic adrenalectomy: an updated meta analysis. Urol J 13:2590–2598
Han JH, Hong TH, You YK, Kim DG (2017) Surgical results of reduced port laparoscopic adrenalectomy using a multichannel port in comparison with conventional laparoscopic adrenalectomy. Asian J Surg 40:6–11
Machado MT, Nunes-Silva I, da Costa EF, Hidaka AK, Faria EF, Zampolli H, Bezerra CA (2017) Laparoendoscopic single-site retroperitoneoscopic adrenalectomy: bilateral step-by-step technique. Surg Endosc 31:3351–3352
Hu Q, Gou Y, Sun C, Xu K, Xia G, Ding Q (2013) A systematic review and meta-analysis of current evidence comparing laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy. J Endourol 27:676–683
Kan HC, Pang ST, Wu CT, Chang YH, Liu CY, Chuang CK, Lin PH (2017) Robot-assisted laparoendoscopic single site adrenalectomy: a comparison of three different port platforms with 3 case reports. Medicine 96:e9479
Narita M, Kageyama S, Okegawa T et al (2018) Urological laparoendoscopic single-site and reduced port surgery: a nationwide survey in Japan. Int J Urol 25:263–268
Sato F, Nakagawa K, Kawauchi A et al (2017) Laparoendoscopic single-site surgeries: a multicenter experience of 469 cases in Japan. Int J Urol 24:69–74
Hirano D, Minei S, Yamaguchi K, Yoshikawa T, Hachiya T, Yoshida T, Ishida H, Takimoto Y, Saitoh T, Kiyotaki S, Okada K (2005) Retroperitoneoscopic adrenalectomy for adrenal tumors via a single large port. J Endourol 19:788–792
Fukumoto K, Miyajima A, Hattori S, Matsumoto K, Abe T, Kurihara I, Jinzaki M, Kikuchi E, Oya M (2017) The learning curve of laparoendoscopic single-site adrenalectomy: an analysis of over 100 cases. Surg Endosc 31:170–177
Acknowledgments
We thank Hyungmin Kim for his assistance in the operating room and for sharing the idea of a new reduced-port site RPRA technique.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Won Woong Kim, Yu-mi Lee, Ki-Wook Chung, Suck Joon Hong, and Tae-Yon Sung have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, W.W., Lee, Ym., Chung, KW. et al. Safety and feasibility of reduced-port site surgery for robotic posterior retroperitoneal adrenalectomy. Surg Endosc 34, 4291–4297 (2020). https://doi.org/10.1007/s00464-019-07273-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07273-0