Abstract
Background
Peroral endoscopic myotomy (POEM) is a safe and effective approach for achalasia. However, the safety, feasibility, perioperative and long-term efficacy in treating geriatric patients has not been well evaluated.
Methods
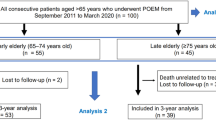
Data of 2367 patients diagnosed with achalasia and treated with POEM in the Endoscopy Center, Zhongshan Hospital, Fudan University from August 2010 to December 2017 were retrospectively reviewed. Last follow-up was in December 2018. Propensity score matching based on baseline characteristics was used to adjust for confounding. With a caliper of 0.01 in propensity scoring, 139 patients aged ≥ 65 years were matched at a 1:2 ratio with 275 patients aged < 65 years. Perioperative complications and long-term outcomes were compared between the two groups.
Results
After propensity score matching, the two groups had similar baseline clinical characteristics and distribution of propensity scores. The mean age was 70.22 years in geriatric patients and 42.02 in younger patients. Technical failure occurred in one geriatric and one non-geriatric patients (p = 0.485). The procedural time in geriatric patients was similar to younger patients [50 (interquartile range (IQR) 36–76) vs. 50 (IQR 36–70) min, p = 0.398]. There were also no significant differences in major perioperative adverse events (2.88% vs. 2.18%, p = 0.663) and hospitalization length (median 3 vs. 3 days, p = 0.488). During a median follow-up period of 41 months (IQR 26–60), mean decrease in Eckardt score and pressure of the LES were 6.63 and 11.9 mmHg in geriatric patients, which were similar to the change in non-geriatric patients (6.49 and 11.6 mmHg, p = 0.652 and 0.872, respectively). Clinical reflux occurred in 23.53% geriatric patients and 21.59% non-geriatric patients (p = 0.724). 5-year success rate of 92.94% was achieved in geriatric patients and 92.61% in younger patients (log-rank p = 0.737).
Conclusions
POEM is a safe and reliable treatment in geriatric achalasia patients with confirmed short-term and long-term efficacy compared with those in non-geriatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achalasia is a rare motility disorder of the esophagus characterized by absence of peristalsis and impaired relaxation of the lower esophageal sphincter (LES), leading to symptoms of dysphagia, regurgitation, chest pain and weight loss [1, 2].The incidence of achalasia is estimated to be 0.3–1.5 per 100,000 per year, with the highest incidence appearing in the seventh decade of life [3]. The traditional treatment of achalasia primarily aims at relieving obstructive symptoms, including medication, endoscopic management and Heller surgery [4, 5].
Peroral endoscopic myotomy (POEM) is the creation of a submucosal tunnel followed by myotomy of the lower esophageal sphincter through flexible endoscopy without surgical incisions. It has emerged as a safe and effective approach for the treatment of achalasia since the first report in 2010 [6]. However, the application of POEM in geriatric achalasia patients was rare due to higher comorbidities and assumed higher risk of invasive procedures in these patients. Moreover, the several studies of POEM in geriatric patients were limited by small sample size and short follow-up time. Therefore, we conducted this study based on a large achalasia cohort to comprehensively evaluate the safety, feasibility, perioperative and long-term efficacy of POEM in treating geriatric achalasia patients, and to systemically compare them with adult patients. To minimize the potential effects of selection bias on the patient characteristics of the two groups, we used a propensity score matching model [5].
Methods
Patients
This is a single-center, retrospective cohort study. Data of 2,367 patients diagnosed with achalasia and treated with POEM in the Endoscopy Center, Zhongshan Hospital Fudan University (Shanghai, China) from August 2010 to December 2017 were retrospectively reviewed. All patients had provided informed consent for the procedure. Preoperative evaluation of achalasia included Eckardt score [7], esophageal high-resolution manometry (HRM), esophagogastroduodenoscopy (EGD), and barium swallow. Demographic and clinical information, including patient age, sex, disease duration, sigmoid esophagus, prior treatment, residual contents, mucosal edema, and submucosal fibrosis were extracted from hospital charts. Geriatric was defined as age ≥ 65 years old. Study patients who had been included in previously published studies with more than 50 patients are shown in Supplementary Table S1. This study was approved by the local ethics committee. This study is presented according to the STROBE guidelines.
POEM procedure
The standard POEM procedure was performed as previously described: (1) submucosal injection and mucosal incision; (2) submucosal tunneling; (3) myotomy, from 2 cm proximal to mucosal entry to at least 2 cm below the cardia; and (4) mucosal entry closure [9]. All patients received general anesthesia and endotracheal intubation. Prophylactic antibiotic treatment was initiated 30 min before the procedure and continued until postoperative day 2. Postoperatively, regular proton pump inhibitors for 2 months were given. Procedural details including myotomy length, full-thickness resection and operation time were gathered from endoscopy reports, images, and videos.
Outcome measurements
Perioperative outcomes included technical failure and perioperative major adverse events. Technical failure was defined as the inability to finish the procedure after submucosal injection [8]. Major perioperative adverse events included conversion to laparoscopic or open procedure, blood transfusion, intensive care unit stay after the procedure, invasive operation postoperatively, hospital readmission after discharge, and hospital stay of more than 5 days due to adverse events [9].
Clinical follow-up outcomes included clinical reflux and clinical failure. Clinical failure was defined as a postoperative Eckardt score ≥ 4 [9]. Clinical reflux included symptomatic reflux and reflux esophagitis [10, 11]. Symptomatic reflux was defined as a score of 8 or more in the GerdQ questionnaire [11], and reflux esophagitis was diagnosed and graded by EGD based on Los Angeles (LA) Classification.
Follow-up
Patients received regular follow-up at 1 month, 3 months, 6 months, and 1 year postoperatively, and yearly thereafter. Eckardt score was obtained to evaluate clinical response. Barium swallow was performed to objectively assess treatment efficacy and clinical failure. EGD was regularly performed for both outcome evaluation and cancer screening. HRM was also advised, especially in patients with dysphagia. Detailed telephone interview was performed by trained physicians for patients who lived a long distance from our institution or who were unwilling to return for follow-up, which included questions about symptoms, as well as examinations and treatments at other hospitals. The last follow-up was in December 2018.
Propensity score matching
Propensity score matching (PSM) was performed to control for selection bias in studies comparing two nonrandomized treatment or exposure [5]. It works by matching patients according to their probability of being in the geriatric group or not. The propensity scores were estimated without regard to the outcome using a multiple logistic regression analysis with the exposure group as the dependent variable and baseline variables shown in Table 1 as independent variables. With a caliper of 0.01 in propensity scoring, patients aged ≥ 65 years were matched at a 1:2 ratio with patients aged < 65 years. In the propensity score matched cohort, the effect of age on different outcomes were compared without need to control for baseline confounders.
Statistical analyses
Categorical variables were compared using the χ2 test or Fisher’s exact test, and continuous variables were compared using the Student’s t test or Wilcoxon rank sum test. Logistic regression was used for binary outcomes. Log-rank test and Cox’s regression analysis were used for time-dependent outcomes. Missing values were handled using complete case analysis for exposure and outcomes and available case analysis for other covariates. Two-sided tests were used, and a p value < 0.05 was considered statistically significant. All statistical analyses were carried out with Stata 14.0.
Results
Patient characteristics and propensity score matching
Data of 2367 patients diagnosed with achalasia and treated with POEM were analyzed. Among them, 140 were defined as geriatric patients. Geriatric patients had longer disease duration (p < 0.001), lower Pre-POEM LES resting pressure on HRM (p < 0.001) and higher rate of sigmoid esophagus (p = 0.031) compared with non-geriatric patients (Table 1). Distribution of propensity score in two groups was also highly unbalanced (Fig. 1A). With a caliper of 0.1 in propensity scoring, 139 patients aged ≥ 65 years were matched at a 1:2 ratio with 275 patients aged < 65 years. One female geriatric patient aged 69 failed to match within a caliper of 0.1, and the information of this patient was shown in Supplementary Table S2. Three patients failed to have a second match within the caliper of 0.1 that was not duplicated with other matches. The mean age was 70.22 [standard deviation (SD) 5.68] years in geriatric group (range 65–98) and 42.04 (SD 12.77) years in non-geriatric group. After propensity score matching, the two groups had similar baseline clinical characteristics and distribution of propensity scores (Table 1 and Fig. 1B).
Procedural characteristics in geriatric and non-geriatric patients
The procedural time in geriatric patients was similar to younger patients (50 (interquartile range (IQR) 36–76) vs. 50 (IQR 36–70) min, p = 0.398). The myotomy length in geriatric patients was 10.57 ± 1.81 cm, which was significantly longer than that in non-geriatric patients (10.22 ± 1.81 cm, p = 0.024). This was primarily due to the length of esophageal myotomy (8.48 ± 1.78 cm vs. 8.10 ± 1.22 cm in geriatric and non-geriatric patients, respectively, p = 0.012), while gastric myotomy length was comparable (2.12 ± 0.43 cm vs. 2.09 ± 0.29 cm in geriatric and non-geriatric patients, respectively, p = 0.385). Most patients, 82.73% geriatric patients and 83.64% non-geriatric patients received full-thickness myotomy (p = 0.816). (Table 2)
Perioperative outcomes in geriatric and non-geriatric patients
Technical failure occurred in one geriatric and one non-geriatric patients (p = 0.485). Median hospitalization length was both 3 (IQR 2-4) days in both groups (p = 0.488). There were also no significant differences in the incidence of major perioperative adverse events (p = 0.663) (Table 2). Only 4 of the 139 geriatric patients (2.88%) had major perioperative adverse events, including 1 with delayed bleeding requiring intervention or transfusion and 3 with pneumothorax requiring drainage. Major perioperative adverse events occurred in 6 (2.18%) of the 275 non-geriatric patients, among whom 2 had delayed mucosa barrier failure, 1 had hydrothorax requiring drainage, and 3 had pneumothorax requiring drainage. Detailed information of geriatric patients with major perioperative adverse events is provided in Supplementary Table S2.
Long-term outcomes in geriatric and non-geriatric patients
Among the 2367 patients, 1540 patients had available follow-up data with a median follow-up time of 56 months (IQR 27–56), and the remaining 827 (34.94%) patients were loss to follow-up. The loss to follow-up rate was comparable in geriatric and non-geriatric patients (38.57% and 34.71%, respectively).
In the propensity score matched cohort with 414 patients, 261 patients were followed up and the loss to follow-up rate was also similar in geriatric and non-geriatric groups (38.85% and 36.00%, respectively). In the 261 patients with follow-up information, 85 were geriatric and 176 were non-geriatric patients. During a median follow-up period of 41 months (IQR 26–60), mean decrease in Eckardt score and pressure of the LES were 6.63 and 11.90 mmHg in geriatric patients, which were similar to the change in non-geriatric patients (6.49 and 17.60 mmHg, p = 0.652 and 0.872, respectively).
Clinical reflux occurred in 23.53% geriatric patients and 21.59% non-geriatric patients (p = 0.724). The rate of symptomatic reflux was also similar between geriatric and non-geriatric patients (10.59% vs. 10.23%, p = 0.928). 180 patients received postoperative EGD. Reflux esophagitis was confirmed in 27.08% geriatric patients, which is significantly higher than the 10.61% non-geriatric patients (p = 0.006). Among the 27 patients with reflux esophagitis, 25 were graded, and most patients had LA Grade A esophagitis. (Table 3)
Clinical failure occurred in 19 patients (7.28%) during follow-up, of whom 6 were geriatric patients. 5-year success rate of POEM of 92.94% was achieved in geriatric patients and 92.61% in younger patients (log-rank p = 0.737). Kaplan–Meier curve was shown in Fig. 2. In univariate Cox regression, the risk of clinical failure was similar in geriatric and non-geriatric patients (hazard ratio (HR) 0.94, 95% confidence interval (CI) 0.38–2.30, p = 0.886). (Table 3)
Discussion
Although achalasia is a rare disease in population, older people have a higher incidence compared to younger people [3]. As the cause and pathophysiology of achalasia remain largely unknown, present approaches used to treat achalasia are to lower the LES pressure, to improve empting of esophagus and to relieve symptoms rather than try to correct the underlying abnormality [1].
POEM has recently been introduced as a new minimally invasive treatment for achalasia. However, there are only a few studies of POEM in geriatric achalasia patients, and the safety and efficacy has not been fully evaluated. In 2015, Chen et al. [12] prospectively recruited 15 achalasia patients aged ≥ 65, and treated them with POEM with a median operation time of 55 min. Median myotomy length was 10 cm. Three patients underwent circular myotomy and 12 underwent full-thickness myotomy. Symptoms remitted in all cases during post-POEM follow-up of 6–39 months. Eckardt score reduced from 8 pre-operatively to 1 post-operatively. Median LES pressure decreased from 27.4 to 9.6 mmHg. Median diameter of the esophagus was also significantly decreased from 51.0 mm to 30.0 mm. Only one patient had reflux and no serious complications related to POEM were found. In 2016, Wang et al. [13] reported 31 achalasia patients aged ≥ 65, 21 of which received POEM while the other 10 received pneumatic dilation. The 15 patients in the study of Chen et al. [12] were also included in this study. The mean follow-up time was 21.8 months in POEM group, and only one case suffered from treatment failure. No severe complications were observed during operation and periodical follow-up. Tang et al. [14] reported in 2017 the comparison of 18 achalasia patients aged 60 years and above (63 ± 3.9 years, range 60–74 years) and 95 patients aged < 60 (37.7 ± 11.6 years, range 18–59 years). The procedural time was similar in both groups. There were also no significant differences in the incidence of intraoperative complications (defined as mucosal perforation, pneumothorax and bleeding) and gastroesophageal reflux rate. During the mean follow-up period of 25.2 months, treatment success defined as Eckardt score ≤ 3 was achieved in 92.9% of patients aged ≥ 60 years, and 89.9% of patients aged < 60 years, without statistical significance. Hermandez-Mondragon et al. [15] reported 12 cases of achalasia patients aged ≥ 65 years treated with POEM, with a successful rate of 98%. The above studies suggested the safety and efficacy of POEM in geriatric patients. However, these studies were limited by small sample size, lack of long-term follow-up, or lack of comparison with non-geriatric patients.
In our study, data of 2367 patients diagnosed with achalasia and treated with POEM were retrospectively reviewed, and 139 geriatric patients were matched with 275 non-geriatric patients. Perioperative complications, pre- and postoperative Eckardt score and pressure of the lower esophageal sphincter, esophageal reflux and clinical failure were compared between the two groups. To our knowledge, this is the largest cohort of POEM information with the longest follow-up worldwide. Therefore, our study provides strong evidence of safety and efficacy of POEM for the treatment of achalasia in geriatric patients.
We performed PSM from a preexisting large volume of data to balance the baseline characteristics between geriatric and non-geriatric patients. After propensity score matching, geriatric and non-geriatric had similar baseline clinical characteristics and distribution of propensity scores, suggesting less chance of confounding in studying the outcomes. In the propensity score matched cohort, geriatric patients had longer myotomy length compared with non-geriatric patients. This is probably because operators intentionally make a longer myotomy as geriatric patients are generally considered to have a longer duration and higher severity. Operation time was comparable.
Perioperative outcomes indicate the safety and efficacy of POEM. The perioperative outcomes in our study were acceptable in both geriatric and non-geriatric patients. There was no significant difference in the incidence of technical failure and major perioperative adverse events, as well as and hospitalization length. All major perioperative adverse events were relieved by conservative therapy. Traditionally, POEM was considered a procedure with high technical difficulty and risk in geriatric patients, particularly due to comorbidities and prior treatment related to long disease duration [16].Our findings demonstrate that POEM can be safely performed in geriatric patients.
In long-term follow-up, both groups experienced great decrease in Eckardt score and pressure of the LES. Clinical reflux occurred in 23.53% geriatric patients and 21.59% non-geriatric patients, and most of them only developed mild esophagitis. 5-year success rate of POEM of 92.94% in geriatric patients compared with 92.61% in younger patients also suggested satisfactory long-term efficacy.
Several limitations should be addressed when interpreting the results. First, known and unknown confounders may bias the result because of the retrospective and observational nature of this study. This is partly reduced by propensity score matching. In the matched cohort, all known baseline characteristics were well balanced between two groups, making it less likely to be confounded by these factors. Second, the loss to follow-up rate is relatively high in our study. However, there is no differential loss to follow-up rate in two groups. Third, our cohort only included Asian population, which limited the generalizability in other ethnicities.
In conclusion, we systematically analyzed the largest real-world database of long-term outcomes of POEM for the treatment of achalasia in geriatric patients compared with non-geriatric patients. POEM is a safe and reliable treatment in geriatric achalasia patients with confirmed short-term and long-term efficacy compared with those in non-geriatric patients, making it a promising primary choice for geriatric achalasia patients. Multi-center clinical trials are warranted to compare POEM with other treatment options in geriatric patients.
References
Richter JE (2010) Achalasia—an update. J Neurogastroenterol Motil 16:232–242
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet (London, England) 383:83–93
Sonnenberg A (2009) Hospitalization for achalasia in the United States 1997–2006. Dig Dis Sci 54:1680–1685
Gennaro N, Portale G, Gallo C et al (2011) Esophageal achalasia in the Veneto region: epidemiology and treatment Epidemiology and treatment of achalasia. J Gastrointest Surg 15:423–428
Rubin DB (2004) On principles for modeling propensity scores in medical research. Pharmacoepidemiol Drug Saf 13:855–857
Inoue H, Minami H, Kobayashi Y et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Ren Y, Tang X, Chen Y et al (2017) Pre-treatment Eckardt score is a simple factor for predicting one-year peroral endoscopic myotomy failure in patients with achalasia. Surg Endosc 31:3234–3241
Wu QN, Xu XY, Zhang XC et al (2017) Submucosal fibrosis in achalasia patients is a rare cause of aborted peroral endoscopic myotomy procedures. Endoscopy 49:736–744
Zhang XC, Li QL, Xu MD et al (2016) Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy 48:967–978
Li QL, Wu QN, Zhang XC et al (2018) Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc 87(1405–1412):e1403
Jones R, Junghard O, Dent J et al (2009) Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 30:1030–1038
Li CJ, Tan YY, Wang XH et al (2015) Peroral endoscopic myotomy for achalasia in patients aged >/= 65 years. World J Gastroenterol 21:9175–9181
Wang X, Tan Y, Lv L et al (2016) Peroral endoscopic myotomy versus pneumatic dilation for achalasia in patients aged >/= 65 years. Rev Esp Enferm Digest 108:637–641
Tang X, Ren Y, Gao Q et al (2017) Peroral endoscopic myotomy is safe and effective in achalasia patients aged older than 60 years compared with younger patients. Geriatr Gerontol Int 17:2407–2413
Hernandez-Mondragon OV, Solorzano-Pineda OM, Blancas-Valencia JM et al (2017) Per-oral Endoscopic Myotomy (POEM): a safe and effective treatment for achalasia in geriatric patients. Rev Med del Inst Mex del Seguro Soc 55:S376–s382
Rakita S, Bloomston M, Villadolid D et al (2005) Age affects presenting symptoms of achalasia and outcomes after myotomy. Am Surg 71:424–429
Funding
This study was supported by the Grants from the National Natural Science Foundation of China (Grant Nos. 81873552, 81570595, and 81670483), Major Project of Shanghai Municipal Science and Technology Committee (Grant Nos. 18ZR1406700, 16411950400), Shanghai Sailing Program of Shanghai Municipal Science and Technology Committee (Grant No. 2018YF1403700), Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning (Grant No. 2017YQ026), Chen Guang Program of Shanghai Municipal Education Commission (Grant No. 15CG04), and the Project of Shanghai Municipal Commission of Health and Family Planning (Grant No. SHDC12016203).
Author information
Authors and Affiliations
Contributions
Q-LL, P-HZ: Planning and conducting the study. P-HZ, M-DX, S-YC, Y-SZ, Y-QZ, W-FC, Q-LL, L-QY, X-YL, JC, Z-QL, YW, W-ZQ, J-WH, M-YC: Collecting data. X-YL, Q-LL, JC, W-FC: Analyzing and interpreting data. X-YL, Q-LL: Drafting manuscript. All authors: Final approval of manuscript: .
Corresponding authors
Ethics declarations
Disclosure
Drs. Xin-Yang Liu, Jing Cheng, Wei-Feng Chen, Mei-Dong Xu, Zu-Qiang Liu, Yun-Wang, Shi-Yao Chen, Yun-Shi Zhong, Yi-Qun Zhang, Wen-Zheng Qin, Jian-Wei Hu, Ming-Yan Cai, Li-Qing Yao, Quan-Lin Li and Ping-Hong Zhou have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Impact statement
We certify that this work is novel. We systematically analyzed the largest real-world database of long-term outcomes of POEM for the treatment of achalasia in geriatric patients compared with non-geriatric patients. POEM is a safe and reliable treatment in geriatric achalasia patients with confirmed short-term and long-term efficacy compared with those in non-geriatric patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, XY., Cheng, J., Chen, WF. et al. Effect of peroral endoscopic myotomy in geriatric patients: a propensity score matching study. Surg Endosc 34, 2911–2917 (2020). https://doi.org/10.1007/s00464-019-07070-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07070-9