Abstract
Background
While high-volume Centers of Excellence (COE) for bariatric surgery may have improved clinical outcomes, their disparate distribution results in longer travel distances for patients. The purpose of this study was to investigate effect of distance from COE on outcomes and readmission.
Methods
This was a retrospective study of all adults, aged 18 years or older, receiving bariatric surgery from April 2009 to March 2012 in the province of Ontario. Main outcomes included 30-day complication rates and readmission. Multivariable logistic regression was used to examine the impact of distance from patients’ primary residence to their bariatric COE on patient outcomes and readmissions.
Results
Five thousand and seven patients were identified, two-thirds residing within 100 km of a COE with a mean distance of 117.2 km. The majority of patients did not reside within a Local Integrated Health Network (LHIN) that contained a COE, while 18.3% of patients lived in rural areas. Using multivariable adjustment, for every 10 km increase from the COE where surgery was performed, the Odds Ratio (OR) for complications was 1.00 [95% Confidence Interval (CI) 0.99–1.01; P = 0.747]. Additionally, both residing in a LHIN without a COE, OR 1.10 (95% CI 0.87–1.40; P = 0.434), and rural status, OR 0.97 (95% CI 0.77–1.23; P = 0.821) showed no increase in risk of complication. Similarly, further distances did not influence rate of readmission, OR 0.99 (95% CI 0.98–1.00; P = 0.077) nor did rural status OR 1.31 (95% CI 0.97–1.76; P = 0.076).
Conclusion
The COE model, where a few centers in high population areas service a large geographic region, is adequate in ensuring patients that live further away receive appropriate short-term care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Regionalization of care for specialized procedures has the reported benefits of improved outcomes mainly due to the subsequent increase in surgical volume and concentrated expertise. However, there are potential downsides to centralization of health care services which include the increasing distance between patients and their hospital of treatment [1, 2]. This increase may lead to reduced access to care [3, 4]. Moreover, though the phenomenon of distance bias has been previously reported on, where patients who live further from treatment centers have better long-term outcomes specifically in the medical oncology literature [5, 6], more recent surgical literature has pointed to worse outcomes and a longer length of stay for patients who live further from their treatment center [7,8,9,10]. Therefore, though there may be a benefit from regionalization due to volume-based outcomes, certain patients may actually do worse based on the reorganization of resources further from their home.
The creation of the Centers of Excellence (COE) model for healthcare delivery in bariatric surgery has not only increased distances for patients but has been shown to decrease access to health services specifically for patients who live further from their COE [4, 11]. Furthermore, distance may decrease follow-up after bariatric surgery [12,13,14,15,16,17,18,19] and for similar reasons, patients may be limited in their ability to easily seek early follow-up care for postoperative complications. This may require increased readmission rates in lieu of adequate outpatient care. Therefore, while regionalization can lead to better volume-based outcomes, there may exist a group of patients who suffer from worse health outcomes and differing patterns of health care use based on their proximity to treatment facilities.
In Ontario’s universal health care system, publically funded bariatric surgery is offered almost exclusively using the COE model. Within Ontario, a province of 12.8 million people in an area double the size of Texas, ensuring access to care can be difficult and expensive. This study aims to ascertain whether the COE model of healthcare delivery in bariatric surgery creates a subset of patients who suffer from poorer short-term outcomes and inefficient health resource utilization. More specifically, we hypothesize that distance may increase short-term complications and readmissions after bariatric surgery.
Materials and methods
This was a retrospective cohort study in which the principle objective was to determine whether increasing distance from a bariatric COE was associated with increased short-term overall complication and readmission rates. This study was approved by the research ethics board of St. Joseph’s Hospital, Hamilton, Ontario.
Setting and population
The Ontario Bariatric Network (OBN) manages the publicly funded regionalized bariatric care system within Ontario. At the time of this study, it comprises four bariatric COEs which performed Roux-en-Y gastric bypass (RYGB) and longitudinal sleeve gastrectomy (SG). Referrals for bariatric surgery in Ontario are centralized within the OBN and distributed to centers based on geographic proximity. Despite Ontario’s large size, approximately 70% of the population lives in a small area in Southern Ontario, known as the Golden Horseshoe, which contains three of the four COE consisting of seven of the eight hospitals within these COEs. The OBN also serves as an entity for bariatric education which is directed to all primary care physicians within Ontario, regardless of region.
Patient population
This study included patients who received RYGB or SG within the province of Ontario for the purposes of weigh loss between April 2009 and March 2012. Patients were greater than 18 years of age and were selected for surgery based on NIH criteria [20].
Data sources
Patient demographics, co-morbidities, operations, and outcome data were derived from the Canadian Institute for Health Information (CIHI) Hospital Morbidity Database and Discharge Abstract Database. These data included all potential admissions and readmissions within Ontario for the time period. These data contained information on patient administrative health regions, defined as Local Health Integration Networks (LHINs). There are 14 LHINs in Ontario roughly divided on the basis of population that directly administer the region’s health care resource allocation.
Exposures and outcome
The primary exposure for this study was distance from patients’ home to the COE where their surgery was performed. Patient forward sortation areas were used as a proxy for home address. These are neighborhood size units utilized by Canada’s postal system and are represented by the first three characters of a patient’s postal code. The locations of Ontario’s hospitals were derived from Desktop Mapping Technologies Incorporated’s Enhanced Points Of Interest File. Distances were calculated using the straight-line distance between the patient neighborhood centroid and the COE where they received care.
The main outcomes of interest in this study were short-term overall complication rate and readmissions. Complications had to have occurred during index hospital admission or during a readmission within 30 days of index procedure. Complications are outlined in Table 1 and include specific surgical and medical complications. In addition, the CIHI database allows for identification of general complications that are defined by CIHI as an identified adverse event which extended length of stay by 24 h or required a separate, unplanned procedure. This represents a composite outcome that is determined by the CIHI during the initial data collection process and therefore is the most comprehensive outcome afforded by the dataset. Hospital readmissions were included if they occurred within 30 days of the index procedure. Readmissions to any hospital in Ontario were included within this study.
In addition to distance, rural status of a patient’s neighborhood was examined as a predictor of overall complications and readmission. Rurality was derived from the patients’ postal codes as, in Canada, each postal code is defined as being either rural or urban. Also, whether a patient lived and consequently had surgery within a LHIN that contained a COE (as compared to traveling outside of their LHIN to have surgery) was also examined to determine if an association existed with the outcomes of interest.
Statistical analysis
Descriptive statistics were used to describe the patient population. Patient demographic data were compared using the Chi-square statistic for categorical variables and the Student’s t test for continuous variables. Multivariable logistic regression was used to control for confounding in order to determine the extent to which the aforementioned exposures were associated with short-term overall complications and readmissions. Clinically relevant predictors entered in the model included procedure type, age, gender, baseline co-morbidities, the different COEs, distance from COE, rural status, and whether a COE was within a patient’s LHIN (vs not). Distance from COE was utilized as a continuous variable within the model and presented on a per 10 km basis for simplicity rather than per km. The outcomes of complications and readmission were binary variables. Marginal analysis was used to look at the adjusted relationship between both outcomes and distances. Odds Ratios (OR) with 95% confidence intervals (CI) were reported. Statistical significance was set at P < 0.05. Stata software was used for data analysis (StataCorp. 2013. Stata Statistical Software: Release 12.1. College Station, TX: StataCorp LP).
Results
The population baseline characteristics are detailed in Table 2. There were a total of 5007 patients who underwent either a RYGB (91.7%) or an SG (8.3%), with almost 99% performed laparoscopically. Approximately two-thirds of the patients lived within 100 km of the COE where surgery was performed. The mean distance from patient residence to the COE where bariatric surgery occurred was 117.2 km (standard deviation 168.5 km, data not displayed). The majority of patients were female (81.9%), which differed slightly between patients within and beyond 100 km, but was statistically significant (P = 0.047). Co-morbidities differed between those within 100 km of their COE and above 100 km. Generally, the patients greater than 100 km away were older (44.5 vs 44.4 years; P = 0.022), and had higher rates of hypertension, hyperlipidemia, obstructive sleep apnea, and gastroesophageal reflux disease (P < 0.05). While the rates were also higher for diabetes, renal failure, coronary artery disease, and chronic obstructive pulmonary disease, they were not statistically significant. Overall complication rates were 11.7% in the cohort and readmission rates were 6.1%.
Table 3 outlines the univariate analysis of the exposures of interest and both the overall complication and readmission rates. With every 10-km increase in distance a patient lived from their COE, there was no increase in complication (OR 1.00, P = 0.213). Having a COE within the patient’s home LHIN was associated with a higher complication rate, OR 1.30 (95% CI 1.09–1.55; P = 0.004). Patients from neighborhoods classified as rural had higher complications rates, OR 1.14 (95% CI 0.91–1.41) but was not statistically significant, P = 0.251. There was a statistically significant decreased rate of readmission with increased distance from a COE, but this amounted to just a 1% decrease in the odds of readmission for every 10-km increase in distance, OR 0.99 (P = 0.043). Both having a COE within the patient’s home LHIN and coming from a neighborhood classified as rural had higher rates of readmission but were not significant (P > 0.05).
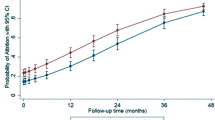
Figures 1 and 2 show the relationships between distance and the outcomes. The scatter plots display weighted markers based on the number of patients within each 50 km interval. The scatter plots are fitted with a line. Both plots demonstrate a decrease in events over distance, although as discussed above, overall complications in non-significant while readmission reaches significance.
Table 4 details the multivariable analysis. After adjustment, there appears to be no association between the odds of complications and increased distance, OR 1.00 (95% CI 0.99–1.01; P = 0.747). Having a COE within a patient’s LHIN, OR 1.10 (95% CI 0.87–1.40), and residing within a rural area, OR 0.97 (95% CI 0.77–1.23) do not appear to be significantly predictive of overall complications, P = 0.434 and P = 0.821, respectively. Similarly, readmission rate does not appear to be associated with distance from the COE, with an odds ratio remaining 0.99 (95% CI 0.98–1.00) though not reaching significance, P = 0.077. While living within a LHIN that contains a COE is not associated with readmission, OR 1.00 (95% CI 0.73–1.37; P = 0.996), living within a rural neighborhood trends towards significance, OR 1.31 (95% CI 0.97–1.76; P = 0.076).
Figures 3 and 4 display the marginal analysis of the multivariable models. Over units of distance, each patient is run through the model to give the average effect on complication rates (Fig. 3) and readmission rates (Fig. 4). The shaded area represents the 95% CI. Figure 3 illustrates a slight increase over distance of the probability of complications with very wide CIs. Figure 4 demonstrates a declining readmission rate with distance.
Discussion
This study is unique in that it is the first to assess the effect of distance on short-term outcomes and readmissions in bariatric surgery. Our data show that distance from a COE did not result in worsened short-term outcomes for bariatric surgery patients or higher readmission rates. Specifically, the OR for complications for every 10-km increase in distance from the COE where patients had bariatric surgery was 1.00 (P = 0.747) while for readmission, OR 0.99 (P = 0.077). Additionally, patients living in a LHIN with a COE within its boundaries had no effect on complication or readmission rates. Finally, patients living in rural areas also did not suffer increased complications, but trended towards higher readmission rates, OR 1.31 (95% CI 0.97–1.76; P = 0.076).
There is an abundance of evidence suggesting that regionalization of bariatric surgery, with the resultant high volume status and designation as a COE, improves patient outcomes [21,22,23,24,25,26,27,28]. Improved outcomes include a reduction in overall complications, death, and reoperation [26,27,28]. While the majority of evidence points to this positive effect of centralization, a number of studies do call into question whether this ‘volume-outcome hypothesis’ is in fact true, citing poor study design and lack of appropriate controls for comparison and suggesting that perhaps centralization is just one part in a number of initiatives improve outcomes [29,30,31]. These include technical changes over time, surgeon experience, policy changes, and improved technologies. In addition to improved outcomes, costs also appear to be lower [24, 26, 27, 32]. The implementation of a center of excellence model in bariatric surgery has led to an increased distance to treatment facilities as well as a decreased delivery of bariatric surgery for patients who live further from regionalized centers [4, 11]. The effect of this increased distance and unequal distribution on short-term outcomes had not been previously explored in bariatric surgery. Previous medical literature related to oncologic outcomes actually found that patients coming from further away had improved outcomes, a poorly understood phenomenon [5, 6]. More recent findings in the surgical literature found that patients who lived further from their treatment facility had poorer outcomes [7, 8]. However, the latter study by Chou et al. found that readmission was not affected by distance, similar to this study [8]. Additionally, the first orthopedic surgery study that examined the effect of distance on complications after reorganization to a COE model for total joint arthroplasties also found no effect of distance on rates of complications [33].
This study is important from a policy perspective. With bariatric surgery comparatively new in Ontario and Canada as a whole, it is incumbent upon policy makers to make evidence-based decisions on resource allocation and evaluate the COE strategy currently employed to service its populace. Despite Ontario’s large size, compounded by the fact that approximately 70% of the population within the Golden Horseshoe and the remainder dispersed over a vast landmass, it appears distance from COE did not have any negative effect on complication rates or need for re-hospitalization in a bariatric regionalized care system. This is important, as a reverse distance bias would have been problematic for policy makers. As it stands, from an outcomes perspective, there should continue to be concern based on the increased distance for patients created by regionalization. Bariatric surgery poses a unique patient population and previous studies have demonstrated high variation in the knowledge, familiarity, and comfort level of primary care providers in dealing with bariatric surgery and morbidly obese patients [34, 35].
This study has several limitations. CIHI is an administrative database and is subject to response bias and measurement error [36, 37]. The administrative character of the database also limits our ability to adjust for all clinically relevant variables. Despite controlling for COE in our multivariable analysis, there remained heterogeneity between surgeon practices which could not be adjusted for, though all centers met criteria for OBN center of excellence designation. We also did not have capture emergency or outpatient visits and thus we used readmission as our health utilization proxy. Additionally, the findings of the study applied to Ontario specifically and our findings may not be entirely generalizable to different health systems. Finally, a number of initiatives as part of the roll out of the Ontario Bariatric Network included education to primary care physicians and local hospitals to ensure quality care that could not be accounted for in our analysis. However, these campaigns were for all of Ontario and not for specific areas and therefore we do not believe would have a great impact on the analysis.
Despite the fact that increased distance to COEs is a consequence of regionalization of bariatric surgery, our study found no short-term impact of distance on complications or readmission. Considering the benefits to outcomes of high volume regionalized centers, the data in this study affirm the viability of this model as a method for healthcare delivery.
References
Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC (2003) Regionalization of high-risk surgery and implications for patient travel times. JAMA 290:2703–2708. https://doi.org/10.1001/jama.290.20.2703
Kansagra SM, Curtis LH, Schulman KA (2004) Regionalization of percutaneous transluminal coronary angioplasty and implications for patient travel distance. JAMA 292:1717–1723. https://doi.org/10.1001/jama.292.14.1717
Goodman DC, Fisher E, Stukel TA, Chang C (1997) The distance to community medical care and the likelihood of hospitalization: is closer always better? Am J Public Health 87:1144–1150
Doumouras AG, Saleh F, Gmora S, Anvari M, Hong D (2016) Regional variations in the public delivery of bariatric surgery: an evaluation of the center of excellence model. Ann Surg 263:306–311. https://doi.org/10.1097/SLA.0000000000001129
Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, Haraf DJ, Brockstein BE, Sellergren SA, Vokes EE (2003) Is patient travel distance associated with survival on phase II clinical trials in oncology? J Natl Cancer Inst 95:1370–1375
Paltiel O, Ronen I, Polliack A, Epstein L (1998) Two-way referral bias: evidence from a clinical audit of lymphoma in a teaching hospital. J Clin Epidemiol 51:93–98
Etzioni DA, Fowl RJ, Wasif N, Donohue JH, Cima RR (2012) Distance bias and surgical outcomes. Med Care 51:1. https://doi.org/10.1097/MLR.0b013e318270bbfa
Chou S, Deily ME, Li S (2014) Travel distance and health outcomes for scheduled surgery. Med Care 52:250–257. https://doi.org/10.1097/MLR.0000000000000082
Jackson KL, Glasgow RE, Mone MC, Sheng X, Mulvihill SJ, Scaife CL (2014) Does travel distance influence length of stay in elective pancreatic surgery? HPB 16:543–549. https://doi.org/10.1111/hpb.12180
Jackson KL, Glasgow RE, Hill BR, Mone MC, Sklow B, Scaife CL, Sheng X, Peche WJ (2013) Does travel distance influence length of stay in elective colorectal surgery? Dis Colon Rectum 56:367–373. https://doi.org/10.1097/DCR.0b013e31827e939e
Livingston EH, Burchell I (2010) Reduced access to care resulting from centers of excellence initiatives in bariatric surgery. Arch Surg 145:993. https://doi.org/10.1001/archsurg.2010.218
Moroshko I, Brennan L, O’Brien P (2012) Predictors of attrition in bariatric aftercare: a systematic review of the literature. Obes Surg 22:1640–1647. https://doi.org/10.1007/s11695-012-0691-3
Lara MD, Baker MT, Larson CJ, Mathiason M, Lambert PJ, Kothari SN (2005) Travel distance, age, and sex as factors in follow-up visit compliance in the post-gastric bypass population. Surg Obes Relat Dis 1:17–21. https://doi.org/10.1016/j.soard.2004.11.001
Jenkins TM, Xanthakos S, Zeller MH, Barnett SJ, Inge TH (2011) Distance to clinic and follow-up visit compliance in adolescent gastric bypass cohort. Surg Obes Relat Dis 7:611–615. https://doi.org/10.1016/j.soard.2011.01.039
McVay MA, Friedman KE, Applegate KL, Portenier DD (2013) Patient predictors of follow-up care attendance in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis 9:956–962. https://doi.org/10.1016/j.soard.2012.11.005
Wheeler E, Prettyman A, Lenhard MJ, Tran K (2008) Adherence to outpatient program postoperative appointments after bariatric surgery. Surg Obes Relat Dis 4:515–520. https://doi.org/10.1016/j.soard.2008.01.013
DeNino WF, Osler T, Evans EG, Forgione PM (2010) Travel distance as factor in follow-up visit compliance in postlaparoscopic adjustable gastric banding population. Surg Obes Relat Dis 6:597–600. https://doi.org/10.1016/j.soard.2010.09.008
Jennings N, Boyle M, Mahawar K, Balupuri S, Small P (2013) The relationship of distance from the surgical centre on attendance and weight loss after laparoscopic gastric bypass surgery in the United Kingdom. Clin Obes 3:180–184. https://doi.org/10.1111/cob.12031
Sivagnanam P, Rhodes M (2010) The importance of follow-up and distance from centre in weight loss after laparoscopic adjustable gastric banding. Surg Endosc 24:2432–2438. https://doi.org/10.1007/s00464-010-0970-9
NIH Conference (1991) Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med 115:956–961
Zevin B, Aggarwal R, Grantcharov TP (2012) Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 256:60–71
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium, Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W, Pories W, Courcoulas A, McCloskey C, Mitchell J, Patterson E, Pomp A, Staten MA, Yanovski SZ, Thirlby R, Wolfe B (2009) Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 361:445–454. https://doi.org/10.1056/NEJMoa0901836
Birkmeyer NJO, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD (2010) Hospital complication rates with bariatric surgery in Michigan. JAMA 304:435–442
Morton JM, Garg T, Nguyen N (2014) Does hospital accreditation impact bariatric surgery safety? Ann Surg 260:504–508. https://doi.org/10.1097/SLA.0000000000000891 (discussion 508–9).
Gebhart A, Young M, Phelan M, Nguyen NT (2014) Impact of accreditation in bariatric surgery. Surg Obes Relat Dis 10:767–773. https://doi.org/10.1016/j.soard.2014.03.009
Flum DR, Kwon S, MacLeod K, Wang B, Alfonso-Cristancho R, Garrison LP, Sullivan SD, Bariatric Obesity Outcome Modeling Collaborative (2011) The use, safety and cost of bariatric surgery before and after Medicareʼs national coverage decision. Ann Surg 254:860–865. https://doi.org/10.1097/SLA.0b013e31822f2101
Nguyen NT, Nguyen B, Nguyen VQ, Ziogas A, Hohmann S, Stamos MJ (2012) Outcomes of bariatric surgery performed at accredited vs nonaccredited centers. J Am Coll Surg 215:467–474. https://doi.org/10.1016/j.jamcollsurg.2012.05.032
Kwon S, Wang B, Wong E, Alfonso-Cristancho R, Sullivan SD, Flum DR (2013) The impact of accreditation on safety and cost of bariatric surgery. Surg Obes Relat Dis 9:617–622. https://doi.org/10.1016/j.soard.2012.11.002
Dimick JB, Nicholas LH, Ryan AM, Thumma JR, Birkmeyer JD (2013) Bariatric surgery complications before vs after implementation of a national policy restricting coverage to Centers of Excellence. JAMA 309:792–799. https://doi.org/10.1001/jama.2013.755
Simunovic M, Urbach D, Major D, Sutradhar R, Baxter N, To T, Brown A, Davis D, Levine MN (2010) Assessing the volume-outcome hypothesis and region-level quality improvement interventions: pancreas cancer surgery in two Canadian Provinces. Ann Surg Oncol 17:2537–2544. https://doi.org/10.1245/s10434-010-1114-0
Doumouras AG, Saleh F, Anvari S, Gmora S, Anvari M, Hong D (2017) Mastery in bariatric surgery: the long-term surgeon learning curve of Roux-en-Y gastric bypass. Ann Surg 267:489–494. https://doi.org/10.1097/SLA.0000000000002180
Doumouras AG, Saleh F, Tarride J-E, Hong D (2016) A population-based analysis of the drivers of short-term costs after bariatric surgery within a publicly funded regionalized center of excellence system. Surg Obes Relat Dis 12:1023–1031. https://doi.org/10.1016/j.soard.2016.02.016
Nwachukwu BU, Dy CJ, Burket JC, Padgett DE, Lyman S (2015) Risk for complication after total joint arthroplasty at a center of excellence: the impact of patient travel distance. J Arthroplasty 30:1058–1061. https://doi.org/10.1016/j.arth.2015.01.015
Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF (2009) Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity (Silver Spring) 17:1710–1716. https://doi.org/10.1038/oby.2009.62
Balduf LM, Farrell TM (2008) Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res 144:49–58
Canadian Institute for Health Information (2011) Data quality documentation, hospital morbidity database, 2010–2011—executive summary. CIHI, Ottawa
Canadian Institute for Health Information (2009) Data quality documentation, discharge abstract database, 2008–2009—executive summary. CIHI, Ottawa
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Aristithes Doumouras, Fady Saleh, Dennis Hong have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Doumouras, A.G., Saleh, F. & Hong, D. The effect of distance on short-term outcomes in a regionalized, publicly funded bariatric surgery model. Surg Endosc 33, 1167–1173 (2019). https://doi.org/10.1007/s00464-018-6383-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6383-x