Abstract
Background
Nonobstetric surgical interventions are required in some women during pregnancy. The most common nonobstetric conditions requiring surgery during pregnancy are acute appendicitis and cholecystitis. This study aimed to evaluate pregnancy outcomes and complications following surgical procedures for presumed nonobstetric surgical interventions during pregnancy, and to compare the outcomes between the laparoscopic and open approaches.
Methods
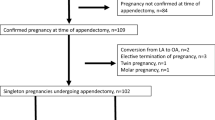
We conducted a retrospective study of patients who underwent laparoscopic or open surgery during pregnancy for nonobstetric surgical indications at our institution between 2008 and 2016.
Results
A total of 62 consecutive patients who underwent surgical intervention due to nonobstetric causes during pregnancy were included in our study. Of these, 35 (56.5%) were managed with laparoscopy and 27 (43.5%) with the open approach. Patients who underwent laparoscopy had a significantly shorter hospital stay and lower pain score on postoperative day 2 than those who underwent open surgery (5.5 vs. 7.2 days, p = 0.03 and 1.4 vs. 2.4, p < 0.01, respectively). There were no significant differences in operative complications between both groups. In advanced pregnancy (gestational age ≥ 23 weeks), 7 patients (41.2%) were managed with laparoscopy and 10 (58.8%) with the open approach. No differences in surgical complications were found between both groups in advanced pregnancy as well.
Conclusions
In our study, laparoscopic surgery was found to be feasible and safe in the late second and third trimesters as well as in the first and early second trimesters without adverse effects on pregnancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Nonobstetric surgical interventions are required in approximately 1 in 133 to 1 in 45 women during pregnancy [1, 2]. The most common conditions for which nonobstetric surgery is required during pregnancy are acute appendicitis and cholecystitis. Other surgical indications include a persistent adnexal mass or adnexal torsion, intestinal obstruction, and abdominal pain of unknown etiology [3, 4]. Although laparoscopic surgery during pregnancy is reluctantly performed because of concerns of possible adverse effects on the mother and developing fetus, the use of this approach in the first and early second trimester has been increasing considerably over the past decade. Lemieux et al. demonstrated that laparoscopic surgery for suspected appendicitis is a safe alternative to open surgery and no significant differences were found in the rate of preterm delivery between trimesters in cases of surgery [5]. Other reports have stated the advantages of the laparoscopic approach based on comprehensive literature reviews; they have concluded that laparoscopy is increasingly being utilized during pregnancy and, as evidence accumulates, no increase in the adverse outcome rate has been reported [6]. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Guidelines Committee suggests that laparoscopy can be used safely during any trimester of pregnancy [4]. However, there is still limited data on the role of laparoscopic surgery, especially in the late second and third trimesters. Most surgeons are still hesitant to use laparoscopy in advanced pregnancy because of reduced fetal perfusion during surgery, technical difficulty in obtaining adequate exposure for surgery, the risk of uterine injuries, and the potential risk of abortion and preterm delivery.
The aim of this study was to evaluate the clinical and obstetric outcomes of pregnancies and compare the complications following surgical procedures between the laparoscopic and open approaches for various nonobstetric surgical conditions during pregnancy, especially in the late second and third trimesters.
Materials and methods
This retrospective study was performed in the Obstetrics and Gynecology Department of Dongguk University Ilsan Hospital, which is a referral center affiliated with Dongguk University College of Medicine, Korea. This study was approved by the Institutional Review Board of the Dongguk University Ilsan Hospital (IRB No. 2017-09002). To identify eligible patients, medical records from 2008 to 2016 containing data on pregnancy and non-obstetrical indications, such as appendicitis, cholecystitis, adnexal mass, adnexal torsion, and hemoperitoneum, based on the International Classification of Disease, Ninth Revision, and Clinical Modification (ICD-9-CM), were extracted. The records of all pregnant women who underwent surgery were evaluated. All women in this study were diagnosed primarily based on clinical examination and imaging studies. Patients who needed surgical diagnosis or treatment that could not be postponed until after delivery were included. The surgical approach was decided by the judgment of surgeon on the basis of the patient’s condition, pregnancy trimesters, and skills of the surgeon. Cholecystectomy was performed in patients who were diagnosed with symptomatic cholelithiasis or acute cholecystitis in pregnancy and were nonresponsive to medical treatment. Surgical interventions for maternal adnexal masses were performed if the mass became symptomatic, grew in size, had suspected adnexal torsion, or had certain characteristics that required pathologic confirmation. The reasons for surgery were divided into infectious and non-infectious causes, for evaluating the possibility of chorioamnionitis.
Preoperative management
All patients were nil per os for surgery. Patients were administered intravenous antibiotics and intravenous hydration using crystalloid fluid before surgery, if needed. Obstetric ultrasonography was also performed to confirm gestational age (GA) and fetal viability before surgery. All patients were assessed by an obstetrician to exclude the probability of any other pregnancy-related diseases.
Laparoscopic technique
Patients were placed in the supine position with the table tilted to the left. Intra- and postoperative pneumatic compression stockings were used for prophylaxis of deep venous thrombosis. A Foley catheter was placed and a prophylactic antibiotic was used intravenously before incision. The Veress needle or the Hasson technique was used based on the surgeon’s preference. The Hasson technique was used in cases of advanced pregnancy or obese mothers for avoiding injury to the gravid uterus and internal abdominal organs due to the trocar. For patients over the 20th week of pregnancy, insertion of the first trocar was performed under ultrasonographic guidance. For ultrasonography-guided trocar insertion, the probe was placed sagittally near the umbilicus and the level of the uterine fundus was identified. The first skin incision was made on or above the umbilicus, and the Veress needle or trocar was advanced from the end of the probe keeping the beam in line, considering the fundus level and other intra-abdominal organs. The first trocar for the camera was placed in a more cephalad direction, toward the xiphoid process, above the uterine fundus. Insufflation was performed with carbon dioxide and an intra-abdominal pressure of 10–15 mmHg was maintained during the operation. An 11-mm trocar was used for a 0° or 30° 10-mm laparoscope and one or two subsequent trocars were placed under laparoscopic visualization (Fig. 1). The trocar position was determined based on the GA and surgical procedure. The surgical specimen was removed using an endobag.
Postoperative management
Tococardiography was routinely performed right after the surgical intervention to evaluate uterine contraction and fetal monitoring. Prophylactic tocolytic agents were not provided routinely, but were administered if the patient experienced uterine contractions before and/or after surgery. Early ambulation after surgery was recommended to prevent deep vein thrombosis. Ultrasonography was repeated before discharge from the hospital.
Clinical data regarding demographic information, operative data, and postoperative outcomes were collected. Operative data included the type of surgery, operative time, estimated blood loss, and intraoperative complications. Postoperative outcomes included surgical outcome, pathological findings, length of hospital stay, and postoperative complications. Obstetric data included GA at delivery, delivery type, Apgar score at 1 and 5 min, birth weight, and maternal and fetal complications. The intensity of pain and discomfort felt at about 24 and 48 h after surgery was assessed using the Numeric Rating Scale (NRS) for pain [7]. The NRS for pain is an 11-point scale where the end points are the extremes of no pain (score 0) and pain as bad as it could be, or worst pain (score 10).
We compared surgical and pregnancy outcomes between patients undergoing laparoscopy and open surgery. The primary outcomes were the surgery-related complication rate and the 1-month preterm delivery rate. Secondary outcomes were all other procedure- and pregnancy-related parameters. Pregnancy trimesters were divided into the first (1–14 weeks), second (15–28 weeks), and third (29–42 weeks). Preterm delivery was defined according to birth in or before the 37 weeks of gestation, as defined by the American College of Obstetricians and Gynecologists [8], and 1-month preterm delivery was defined as preterm birth within 1 month after surgery for presumed nonobstetric causes. We also compared surgical and pregnancy outcomes according to surgical approach in advanced pregnancy for the evaluation of laparoscopy efficacy in the late second and third trimester. Advanced pregnancy was defined as GA ≥ 23 weeks because it is considered to represent the threshold of fetal viability.
Comparisons were made using Student’s t test, Pearson’s Chi-square test, Fisher’s exact test, and analysis of variance (one-way ANOVA) when appropriate. A p value < 0.05 was considered statistically significant. SPSS version 21.0 (Armonk, NY: IBM Corp.) was used for all statistical analyses.
Results
A total of 62 consecutive patients who underwent surgical intervention due to nonobstetric causes during pregnancy were included in our study. Of these patients, 35 (56.5%) were managed with laparoscopy and 27 (43.5%) with the open approach. No laparoscopic case was converted to open surgery. Twenty-two patients (35.5%) were first-trimester pregnancies, 32 (51.6%) were second-trimester pregnancies, and 8 (12.9%) were third-trimester pregnancies. The laparoscopic approach was utilized until 35 weeks of gestation.
Demographic data are summarized in Table 1. Patients who underwent laparoscopy had a significantly shorter hospital stay than those undergoing open surgery (5.5 vs. 7.2 days, p = 0.03). There was a significant difference in pain score on postoperative day 2 between the laparoscopic and open surgery groups (1.4 vs. 2.4, p < 0.01). Although significant differences were not demonstrated in the pain score on postoperative day 1 between both groups (2.6 vs. 3.5, p = 0.08), patients in the laparoscopic surgery group complained of less postoperative pain than those in the open surgery group. No other statistically significant differences were found between groups with respect to maternal age, pre-pregnancy body mass index (BMI), GA at surgery, operative time, and estimated blood loss (Table 1).
The most common conditions leading to surgery were acute appendicitis (62.9%), followed by ovarian cyst (14.5%), adnexal torsion (12.9%), cholecystitis (6.5%), and others (3.2%) (Table 2). Of patients who underwent open surgery, one patient with suspected acute appendicitis showed right adnexal torsion with a normal appendix, and one patient underwent myomectomy for a large 20-cm subserosal myoma. Nine patients underwent ovarian cystectomy, including three patients with ovarian cysts > 6 cm, two patients with growing cyst size, and four patients with a suspicious borderline malignant tumor, for which pathologic confirmation was required. One patient who underwent laparoscopic surgery for hemoperitoneum had a heterotopic pregnancy. She had developed hemoperitoneum because of a ruptured left tubal pregnancy with a normal intrauterine pregnancy. She underwent left salpingectomy and hematoma evacuation through a laparoscopic approach and had a normal pregnancy until 36 weeks of GA and birth.
The overall complication rate was 19.3% (12/62) (Table 3). Wound complications occurred in one patient (2.9%) in the laparoscopic surgery group, and three patients (11.1%) in the open surgery group. Four patients (11.5%) in the laparoscopic surgery group and 6 patients (22.2%) in the open surgery group were treated with tocolytic agents because of preterm labor after surgery. One-month preterm delivery occurred in one patient in the open surgery group (3.7%). There were no significant differences in postoperative complications between two groups. Seven women in the laparoscopic surgery group and nine women in the open surgery group were lost to follow-up, so obstetric outcome information was available only for 46 women. The GA at delivery, rate of cesarean section, and time from surgery to delivery showed no significant differences between groups.
Table 4 shows comparisons of perioperative and postoperative variables in advanced pregnancy between the laparoscopic and open surgery groups. Seventeen patients underwent surgical intervention in advanced pregnancy (GA ≥ 23 weeks of gestation). Of these, 7 patients (41.2%) were managed with laparoscopy and 10 (58.8%) with the open approach. Laparoscopic surgery was performed for patients with appendicitis (57.1%), ovarian cyst (14.3%), and adnexal torsion (28.1%). Open surgery was performed for patients with acute appendicitis (80.0%), cholecystitis (10.0%), and adnexal torsion (10.0%). There were no significant differences in GA at surgery, operative time, and hospital stay between the laparoscopic and open surgery groups. Patients who underwent laparoscopic surgery complained of less pain on postoperative day 2 than those undergoing open surgery. Tocolytic agents were administered in two patients due to preterm labor in the laparoscopic surgery group and five patients in the open surgery group. The patient with 1-month preterm delivery was a woman at 34 weeks of gestation who underwent appendectomy via the open approach. She presented with a 1-day history of right lower quadrant abdominal pain, tenderness, an elevated white blood cell count of 13,670/μL, no fever, and an abdominal sonogram showing a hypoechoic tubular structure with swelling. A 7 × 1.4-cm congested necrotic appendix was noted intraoperatively and the pathologic diagnosis was acute suppurative appendicitis. Preterm labor occurred after surgery and tocolytic agents were administered for 69 h. After ceasing tocolytic agents, the preterm labor subsided and the patient could be discharged on the 4th postoperative day. Approximately 2 weeks later, she presented with membrane rupture and spontaneous preterm delivery, with an estimated GA of 36 weeks. The baby had an Apgar score of 5 at 1 min and 7 at 5 min and required neonatal intensive care due to prematurity. There was no pathologic evidence of chorioamnionitis in the placenta and umbilical cord. The baby had no neurologic damage or other complications at 3 months.
Discussion
Management of nonobstetric surgical conditions among pregnant patients may present a dilemma to the surgeon, obstetrician, anesthesiologist, and neonatologist because the medical team must weigh the risks and benefits of surgery not only to the mother but also to the fetus. Surgeries during pregnancy may expose the mother and/or fetus to risks of fetal loss, wound complications, pain, preterm labor, and preterm delivery. However, delayed diagnosis and treatment of surgical diseases in pregnancy may lead to further complications, such as tissue necrosis and peritonitis, leading to spontaneous abortion, preterm labor, and chorioamnionitis. Therefore, if surgeries are necessary for pregnant patients, the optimal surgical approach should be decided upon on the basis of the patient’s condition, trimester of pregnancy, and skills of the surgeon, as well as consideration of the risks and benefits of laparoscopic and open surgery. Early concerns over laparoscopic surgery performed on pregnant patients were centered on the potential risk to the mother and fetus due to trocar insertion, CO2 insufflation, and technical ability to obtain the proper operative exposure with a gravid uterus. However, laparoscopic surgery has been increasingly reported with good outcomes in pregnant patients, similar to outcomes in nonpregnant patients. Studies demonstrating the safety and efficacy of laparoscopy during pregnancy have been reported, and this may provide more options in managing pregnant patients with surgery [2, 4].
In our study, we compared maternal demographics and surgical outcomes between patients who underwent laparoscopy and those who underwent open surgery. A shorter hospital stay and lower pain scores were found in the laparoscopic group compared with the open surgery group. There were no significant differences in postoperative complications, including wound complications and 1-month preterm delivery, which were similar to the findings of other studies [5, 9,10,11,12]. Laparoscopic surgery has many advantages in pregnant patients, including lower risk of wound complications, less postoperative pain, shorter hospital stays, and decreasing the risks of thromboembolic events due to early mobilization. The laparoscopic approach allows for better visualization of the operative field and decreases the need for uterine manipulation. It can be used for various nonobstetric surgical causes such as appendicitis, cholecystitis, or adnexal problems with similar incision site and size. Although infectious causes were anticipated to represent higher risk-related inflammation of the mother such as in chorioamnionitis, our data suggest that there was no effect on pregnancy outcome and complications in this regard. In addition, diagnostic laparoscopy is safe and effective when used selectively in the workup and for the treatment of acute abdominal conditions in pregnancy; prompt proceeding to diagnostic laparoscopy may allow for early identification and intervention when other evaluations are equivocal to diagnose acute abdominal disease in pregnancy. Laparoscopic surgery for pregnant patients with nonobstetric surgical conditions is a less invasive approach and a safe alternative to open surgery [5, 12].
Although laparoscopic surgery is recommended irrespective of GA by SAGES and previous studies [4, 6], limited data are available regarding laparoscopy in advanced pregnancy because most laparoscopic procedures are performed during the first and early second trimester. It is believed that laparoscopic access in advanced pregnancy is difficult because of the enlarged uterus and congestion. Most surgeons are reluctant to perform laparoscopic surgery in pregnant women because of fear of the diminished available working space due to the enlarged uterus, risk of uterine injury, and perceived risk of excessive manipulation of the gravid uterus leading to preterm labor. However, several studies have reported the feasibility and overall favorable outcomes of laparoscopic surgery performed in the second and third trimesters of pregnancy [13,14,15,16]. In this study, we observed no significant differences in the outcomes and complications of surgery in advanced pregnancy. In addition, we have shown that laparoscopic surgery at up to 35 weeks of GA can be performed safely. The operative field is not obscured by the gravid uterus at up to 35 weeks of gestation. The upper GA limit for the laparoscopic approach is not defined and several surgical strategies for advanced pregnancy were introduced to reduce possible complications. Managing trocar insertion is the most important factor for reducing the trauma to the uterus and obtaining adequate exposure. To avoid injury to the gravid uterus, use of the Hasson technique (an open method of port insertion), ultrasonography-guided trocar insertion, and more cephalad placement of the umbilical port could be helpful. The insufflation pressure should be managed to strike a balance between adequate visualization of the intra-abdominal cavity and adverse outcomes of the mother and fetus. Maintaining an intra-abdominal pressure below 10–15 mmHg can be utilized to minimize significant hypercarbia and respiratory acidosis in both mother and fetus, maintain adequate venous return, and provide adequate visualization of the intra-abdominal cavity. A left lateral tilt of the patient also can help reduce compression of the inferior vena cava and aorta and avoid decreasing blood supply to the uterus [15,16,17,18,19]. Regarding fetal monitoring, ACOG has recommended that if the fetus is considered to be viable, simultaneous electronic fetal heart rate and contraction monitoring should be performed before and after the procedure to assess fetal well-being and the absence of contractions. When nonobstetric surgery is planned, a qualified individual should be available to interpret fetal heart rate patterns and an obstetrician who can perform cesarean delivery must be readily available [20].
Due to the retrospective design of this study, it has several strengths and limitations. The most important limitation is the reliance on retrospective data and the small sample size, which increases the likelihood of a type II error. Data were collected from all available electronic medical records, but data related to obstetric outcomes and babies were limited to a few patients. However, a prospective study is difficult to conduct and collection of a large volume of cases is intrinsically challenging because of the urgency or emergency of the treatment. In addition, every patient in our study was followed up for at least 4 weeks after surgery at outpatient clinics, which is a sufficient amount of time to evaluate acute complications related to surgery. Additionally, in our study, nonobstetric surgical interventions were performed for various indications in a relatively large sample size, instead of for one particular disease as in other studies [5, 9, 10, 12]. Our study demonstrated that laparoscopy could be used for many different indications, even in advanced pregnancy.
In summary, based on our study, the laparoscopic approach could be performed safely and efficiently in pregnant patients during any trimester of pregnancy and for various indications compared with open surgery, with decreased maternal co-morbidities including a reduced length of hospital stay, reduced pain after surgery, and prevention of long incisions in a gravid patient without major complications. If the surgeon is experienced and careful attention and the use of strategies to minimize complications of laparoscopic surgery during pregnancy are ensured, laparoscopic surgery is a reproducible technique that has both therapeutic and diagnostic advantages.
References
Kort B, Katz VL, Watson WJ (1993) The effect of nonobstetric operation during pregnancy. Surg Gynecol Obstet 177:371–376
Nezhat FR, Tazuke S, Nezhat CH, Seidman DS, Phillips DR, Nezhat CR (1997) Laparoscopy during pregnancy: a literature review. JSLS 1:17–27
Erekson EA, Brousseau EC, Dick-Biascoechea MA, Ciarleglio MM, Lockwood CJ, Pettker CM (2012) Maternal postoperative complications after nonobstetric antenatal surgery. J Matern Fetal Neonatal Med 25:2639–2644
Guidelines Committee of the Society of American G, Endoscopic S, Yumi H (2008) Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy: this statement was reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), September 2007. It was prepared by the SAGES Guidelines Committee. Surg Endosc 22:849–861
Lemieux P, Rheaume P, Levesque I, Bujold E, Brochu G (2009) Laparoscopic appendectomy in pregnant patients: a review of 45 cases. Surg Endosc 23:1701–1705
Jackson H, Granger S, Price R, Rollins M, Earle D, Richardson W, Fanelli R (2008) Diagnosis and laparoscopic treatment of surgical diseases during pregnancy: an evidence-based review. Surg Endosc 22:1917–1927
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthrit Care Res 63(Suppl 11):S240–S252
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin (2001) Assessment of risk factors for preterm birth. Clinical management guidelines for obstetrician-gynecologists. Number 31., October 2001. (Replaces Technical Bulletin number 206, June 1995; Committee Opinion number 172, May 1996; Committee Opinion number 187, September 1997; Committee Opinion number 198, February 1998; and Committee Opinion number 251, January 2001). Obstet Gynecol 98:709–716
Chang SD, Yen CF, Lo LM, Lee CL, Liang CC (2011) Surgical intervention for maternal ovarian torsion in pregnancy. Taiwan J Obstet Gynecol 50:458–462
Sadot E, Telem DA, Arora M, Butala P, Nguyen SQ, Divino CM (2010) Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc 24:383–389
Reedy MB, Galan HL, Richards WE, Preece CK, Wetter PA, Kuehl TJ (1997) Laparoscopy during pregnancy. A survey of laparoendoscopic surgeons. J Reprod Med 42:33–38
Halkic N, Tempia-Caliera AA, Ksontini R, Suter M, Delaloye JF, Vuilleumier H (2006) Laparoscopic management of appendicitis and symptomatic cholelithiasis during pregnancy. Langenbecks Arch Surg 391:467–471
Upadhyay A, Stanten S, Kazantsev G, Horoupian R, Stanten A (2007) Laparoscopic management of a nonobstetric emergency in the third trimester of pregnancy. Surg Endosc 21:1344–1348
Geisler JP, Rose SL, Mernitz CS, Warner JL, Hiett AK (1998) Non-gynecologic laparoscopy in second and third trimester pregnancy: obstetric implications. JSLS 2:235–238
Donkervoort SC, Boerma D (2011) Suspicion of acute appendicitis in the third trimester of pregnancy: pros and cons of a laparoscopic procedure. JSLS 15:379–383
Weiner E, Mizrachi Y, Keidar R, Kerner R, Golan A, Sagiv R (2015) Laparoscopic surgery performed in advanced pregnancy compared to early pregnancy. Arch Gynecol Obstet 292:1063–1068
Afflick DG, Handrahan DL, Egger MJ, Price RR (1999) The laparoscopic management of appendicitis and cholelithiasis during pregnancy. Am J Surg 178:523–529
Rollins MD, Chan KJ, Price RR (2004) Laparoscopy for appendicitis and cholelithiasis during pregnancy: a new standard of care. Surg Endosc 18:237–241
Clark SL, Cotton DB, Pivarnik JM, Lee W, Hankins GD, Benedetti TJ, Phelan JP (1991) Position change and central hemodynamic profile during normal third-trimester pregnancy and post partum. Am J Obstet Gynecol 164:883–887
ACOG Committee on Obstetric Practice (2011) Nonobstetric surgery during pregnancy. ACOG Committee Opinion No 474. Obstet Gynecol 117:420–421
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hayan Kwon, Minhee Lee, Hyun Soo Park, Sang Ho Yoon, Chae Hyeong Lee, and Ju-Won Roh have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kwon, H., Lee, M., Park, H.S. et al. Laparoscopic management is feasible for nonobstetric surgical disease in all trimesters of pregnancy. Surg Endosc 32, 2643–2649 (2018). https://doi.org/10.1007/s00464-018-6189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6189-x