Abstract
Background
Per oral endoscopic myotomy (POEM) has emerged as a promising option for the treatment of achalasia. This study assessed POEM training process, outcomes, and improvement in quality of life after POEM performed by an interventional endoscopist (mentor) with trainees.
Methods
We performed a retrospective review of data for patients who underwent POEM with involvement of trainees. Trainees were trained in performing mucosotomy, submucosal dissection, creating submucosal tunnel, identifying gastroesophageal junction, myotomy, and closure of mucosal incision in a step-by-step fashion. Trainees’ performance on each step was evaluated by the mentor based on several key points in each step. The short form 36 (SF36) was obtained before and certain times after the primary POEM procedure was performed.
Results
Sixty-two patients, 26 males and 36 females with a mean age of 59 years, who underwent POEM were enrolled. A checklist included all related items for each step was established. All trainees obtained competence within 6 cases for each step. 61/62 (98.3%) patients had a significant improvement in the Eckardt’s score post POEM: 9.3 ± 1.5 prior to POEM and 2.6 ± 1.2 after the POEM (P = 0.001) and a decrease in mean lower esophageal sphincter pressure (LES): pre- and post-procedure mean LES pressures were 28.5 ± 11.4 and 12.1 ± 4.5 mmHg, respectively (P = 0.001). The SF-36 questionnaire demonstrated a significant improvement in quality of life and comparable with those without trainees in other studies.
Conclusion
This preliminary study showed for the first time that training for POEM can be performed in a step-by-step fashion, learning mucosal incision, submucosal dissection, myotomy, and mucosal incision closure from an expert interventional endoscopist without increasing adverse events. The checklist for each step could be used as an important guide in training POEM. The outcomes of POEM in this study were similar to those reported by others without trainees. Further multiple center studies are needed to verify this training process and to establish a formal training protocol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with esophageal motility disorders present with progressive dysphagia to solids and liquids, regurgitation, chest pain, and weight loss. Achalasia cardia is the best defined of the esophageal motility disorders characterized by failure of lower esophageal sphincter (LES) relaxation and aperistalsis of the esophageal body [1,2,3,4]. Traditionally it has been treated either medically, endoscopically by botulinum injection into LES and pneumatic dilation or surgically with disruption of the lower esophageal sphincter [1,2,3,4,5]. The effect of botulinum injection is short lived and it is used only in patients who are poor candidates for other therapies. Pneumatic dilation and surgical myotomy have been effective in the treatment of achalasia, and have been shown to have similar outcomes at 2 years of follow-up [2, 4, 6,7,8]. Pneumatic dilation has been effective with type 1 and type 2 achalasia but loses durability in long term, and is associated with 2–4% risk of esophageal perforation. Surgical disruption of the LES with laparoscopic Heller myotomy has been effective. However, there is a 15% risk of acid reflux despite fundoplication. Dysphagia and inability to belch from fundoplication can cause significant discomfort for patients [2, 9].
Per oral endoscopic myotomy (POEM) is currently being performed successfully worldwide in many centers for achalasia cardia [10]. Since its advent in 2010 [11], worldwide adoption of the POEM procedure has progressed at a rapid rate. Published data suggest that POEM is safe and effective [10, 12,13,14,15,16,17].
POEM is a special endoscopic procedure being performed within a submucosal tunnel in the esophagus. Trainees for this procedure are not routine gastroenterological fellows or surgical residents, instead, they are usually advanced endoscopy trainees, who have completed their 3-year gastroenterology fellowship or 5-year general surgical training. There are no reports on how to train those advanced trainees in performing this special procedure and no data on the safety and efficacy of performing POEM in endoscopy units by Gastroenterologists with trainees. We report our single-center experience-performing POEM in 62 symptomatic patients by an interventional endoscopist with trainees in the endoscopy unit at a major tertiary center and hopefully more studies will be followed to establish a unique training process for POEM in the future.
Materials and methods
The study was approved by institutional review board at Emory University School of Medicine. Beginning December of 2012, all patients who were evaluated at our institution for esophageal motility disorder, including achalasia, and who were candidates for pneumatic dilation or laparoscopic myotomy were offered POEM as part of a retrospective outcomes study. Exclusion criteria included an inability to tolerate general anesthesia and any contraindications to an endoscopy. Preoperative assessment of all patients included confirmation of a symptomatic esophageal motility disorder as defined by standard high-resolution manometry [18], standard upper gastrointestinal endoscopy, barium swallow, and chest computed tomography. The data collected included type of achalasia, Eckardt score, endoscopic data, length of myotomy, total duration of procedure, and intraoperative and postoperative complications. The Eckardt score is a clinically accepted system for evaluating achalasia both before and after treatment. Adverse events were graded based on ASGE lexicon’s severity grading system [19]. Short form SF 36 [20] data were obtained from consenting patients by either direct interview or a telephone interview prior to POEM, and at 1, 3, 6 months and 1 year Post POEM. Clinical success was defined by symptomatic improvement with Eckardt score of ≤ 3.
We used the Given Imaging ManoScan™ 360 High-Resolution Manometry system to assess esophageal motor function as well as resting and residual LES pressure/integrated relaxation pressure. After the manometry catheter is inserted into the nares and the distal tip appropriately passed into stomach, patients were placed in a semi-recumbent position and allowed to accommodate to the catheter. Next, a 30-s recording was made with the patient at rest without swallowing. This interval is called the Landmark Frame™ (Given Imaging). During the Landmark Frame, the basal mean LES pressure is determined relative to the gastric pressure utilizing the esleeve software incorporated on the HRM system.
Trainees during the procedure
Each trainee worked closely with the training endoscopist (mentor). The mentor performed more than 50 POEM before the study. All four trainees had some experience with endoscopic submucosal dissection (ESD) prior to performing POEM cases. All trainees (one junior faculty and three advanced endoscopy fellows) participated in ESD of rectal or gastric lesions, in at least 5 cases before performing POEM. Specifically, they were involved with performing the marking, incision, submucosal dissection, and closure, prior to performing POEM. All of them watched at least 3 POEM procedures before hands-on experience with the procedure. One of the trainee was a faculty. He completed his 3-year GI fellowship training 5 years prior to POEM training. He had performed thousands of EGD, colonoscopy, ERCP, etc. The other three were advanced endoscopy fellows. They completed their 3-year fellowship training, and had performed hundreds of EGD and colonoscopies. Each of them had performed at least 100 ERCP and 100 EUS. None of them had performed POEM on animal models or cadavers. At the first step, they only participated in the establishment of submucosal tunnel by dissecting submucosal layer, then moved to participate in myotomy as the second step. In the third step, they started performing mucosal incision, the first and important step of the procedure, to create a submucosal tunnel orifice. This step is also the most time-consuming step in POEM procedure. Trainees closed each incision with endoclips in each case. All trainees were trained to use the Veress needle or angiocatheter to decompress symptomatic capnoperitoneum.
In addition, to assess the endoscopic performance skill on POEM, the mentor also asked and accessed the trainees’ knowledge in each step, and the trainees had to have the knowledge, and could have satisfactorily completed the step without any instructions from the mentor before they moved to the next step. A checklist for each step in POEM procedure was established to comprehensively include all relative items in each step (Table 1). Finally, each trainee performed all steps with minimal or no input from the mentor.
POEM procedure
All procedures (except two without trainees) were performed by the mentor along with trainees during the study period. All the procedures were performed under general anesthesia in the endoscopy suite, with the patient in supine position. Patient preparation and surgical technique have been described in our previous study and others [10, 21]. The same basic technique [21] was used for all cases. Patients were kept on clear liquids for 2 days prior to POEM and NPO after midnight prior to the day of planned POEM. Patients were administered 4.5 g of piperacillin/tazobactam intravenously or 500 mg of levofloxacin intravenously (if allergic to penicillin) during the procedure and during hospitalization. Oral antibiotics were prescribed on discharge for a total of 7 days. A gastroscope (GIF-H190; Olympus, Tokyo, Japan) with a transparent distal cap attachment (MH-588; Olympus, Japan) was used for all procedures. The esophagus was cleared of any retained particulate matter with water lavage and suction. A triangle tip knife (Olympus, Japan) was used to perform mucosal incision. Carbon dioxide was used for insufflation (UCR, Olympus, Japan) in all cases during the entire length of procedure. Coagrasper (FD-411 QR, Olympus, Japan) was used to achieve hemostasis in the submucosal plane in the soft coagulation mode (ERBE, Germany).
The technique consisted of four basic steps: (i) Mucosal incision, (ii) Submucosal tunneling, (iii) Myotomy, and (iv) Mucosal incision closure. A submucosal bleb of normal saline dyed with methylene blue was created 10 cm above the endoscopically visualized GEJ in the posterior esophagus (5′O clock position) with an injection needle (23G, NM4004-042, Olympus, Japan). A 2-cm mucosal incision was made to facilitate entry into submucosal space. In the process of establishing a submucosal tunnel, repetitive cycles of dissection and injection with dyed normal saline are necessary to delineate the submucosal layer from the muscular layer and to avoid full-thickness perforation or mucosal injury. Careful electrocauterization was used to create and extend a submucosal tunnel from 10 cm above the GEJ to approximately 2 cm past the GEJ into the gastric cardia. After a 12-cm tunnel had been completed, a distal-to-proximal or proximal-to-distal circular myotomy, not full-thickness myotomy, was performed. Mucosal incision was closed with standard endoscopic clips (Resolution clip, Boston Scientific Corporate Marlborough, MA, USA) or (Instinct clips, Cook Medical, INC, Bloomington, IN, USA).
All patients were evaluated with gastrograffin swallow esophagogram on the first postoperative day if there were no complications. If normal, they were then started on a full liquid diet and subsequently discharged. They maintained this diet for 1 week and then were allowed soft food. Patients were followed up in clinic at 1 month post POEM. A high-resolution Manometry was performed at 6 months post POEM and an EGD was performed 6 months post POEM.
Statistical analysis
Data were prospectively collected, and comparison of the pre- and post-procedure parameters were done. Normally distributed data were analyzed using a paired t test. The SF-36 was expressed as medians and analyzed using the Wilcoxon signed-rank test. A P value less than 0.05 was considered statistically different.
Results
General patients’ information and procedure outcomes
A total of 62 patients with esophageal motility disorder underwent POEM at our institution during the study period (Table 2). Of these 62 patients (mean age 59, range 36–85 years, 26 men and 36 females), 13 patients had type 1 achalasia, 47 had type 2 achalasia, 1 patient had type 3 achalasia, and 1 patient who could not undergo manometry was classified as hypertensive LES. The mean Eckardt’s score was 9.3 ± 1.5 prior to POEM. Pre-procedure mean LES pressure was 28.5 ± 11.4 mmHg. Five patients had sigmoid esophagus. Twenty-three patients (37%) had prior botulinum injection, five patients (8%) had prior balloon dilation, and four patients (6%) had prior Heller’s myotomy. They all had those therapies at least 3 months prior to the POEM procedure. POEM was successfully completed in all the patients and all patients underwent a posterior myotomy (5 o’clock position). The mean myotomy length (± SD) was 7.5 ± 0.8 cm. Mean procedure time (min) was 77.6 ± 27.3 and length of hospital stay (days) was 2.8 ± 1 (Table 3).
There were four complications graded according to the ASGE lexicon of adverse events (Table 4); one patient needed chest tube placement for pneumothorax by cardiothoracic surgery within an hour of POEM, one patient developed elevated troponins from thyroid storm following POEM secondary to undiagnosed hyperthyroidism.
Significant pneumoperitoneum developed in 1 patient intraprocedurally, which was successfully decompressed by the endoscopist with temporary placement of a Veress needle (Genicon, Winter Park, Fla). One patient had small volume hematemesis from ibuprofen intake 1 week after POEM, from incision site as seen on EGD which did not require any endoscopic therapy. Therefore, actually only two complications were directly associated with the procedure. Those advent events had no association with the trainees’ status. There were no cases of mucosal injuries or postoperative leaks or infection in the submucosal tunnel.
Trainees’ outcomes
All four trainees were successful in step 1 after an average of 4.25 patients (range 3–6), step 2 with an average of 4.0 patients (range 3–5), and step 3 with an average of 5.0 patients (range 3–6). Three of the four trainees have started performing POEM independently. For each step in POEM, trainees needed 3–6 patients to acquire the adequate skill and completed the step, such as dissection, hemostasis, and myotomy, without instructions from the mentor. Finally, each of them performed two cases of entire POEM with the mentor, but without instructions from the mentor. Therefore, the total threshold number to be able to perform POEM independently was about 20 cases for each trainee.
Clinical outcomes
Overall, patients who underwent POEM for achalasia had a significant improvement in dysphagia. The mean Eckardt’s score was 9.3 ± 1.5 prior to POEM and 2.6 ± 1.2 after the POEM (P = 0.001), 2.2 ± 1.5 (n = 62) at 3 months post POEM (P = 0.001), 2.1 ± 1.7 (n = 57) at 6 months Post POEM (P = 0.001), and 2.1 ± 2.18 (n = 52) at 1 year post POEM (P = 0.001). Pre-procedure and post-procedure mean LES pressure (n = 41) was 28.5 ± 11.43 and 12.1 ± 4.5 mmHg, respectively (P = 0.001) (Fig. 1). Postoperative GERD with PPI use was seen in 8/62 (12.9%). All patients started PPI the day of the POEM procedure and continued for 8 weeks. If patient had GERD symptoms, then PPI was continued as needed. Thirty-six (58%) patients underwent a follow-up EGD that was normal. Three patients had retained endoscopic clips that were removed endoscopically. No procedure-related adverse events were seen during follow-up. Clinical success was defined by symptomatic improvement with Eckardt score of ≤ 3. One patient did not have any response after POEM procedure. Two patients had recurrence of symptoms, including dysphagia, regurgitation, etc, one month after POEM. One patient had recurrence of symptoms three months after POEM (characteristics of non-responders in Table 5). Two patients underwent repeat esophageal HRM, which revealed high resting LES pressure and opted for Heller myotomy. Two other patients refused any further interventions.
Improvement in quality of life
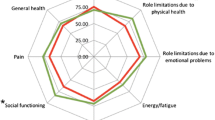
SF 36 data were obtained for 54 patient’s pre POEM, 54 patients at 1 month post POEM, 52 patients at 3 months post POEM, 49 patients at 6 months post POEM, and 46 patients at 1 year post POEM. Outcomes for the eight domains of SF 36 are shown in Table 6. The SF-36 questionnaire demonstrated a significant improvement in quality of life in several domains. At 1 month (n = 54) all domains other than physical functioning and role limitation due to physical functioning domains were significantly improved. At 3 months (n = 52) all domains other than physical functioning were significantly improved. At 1 year (n = 46), bodily pain, vitality, social functioning, and mental health were significantly improved (Fig. 2).
Discussion
POEM has emerged as a safe and effective alternative modality in the treatment of achalasia [10, 12, 22]. Traditionally, PD and LHM remained the mainstay of treatment with equal efficacy at 2 years [2]. POEM becomes more appealing than surgical myotomy since it avoids external incision and dissection of esophageal hiatus, thus allowing for early recovery and less pain with the procedure [13]. Moreover, the cost of performing POEM is significantly lower compared to surgical myotomy [9].
The main aims of the study were to evaluate training process, clinical outcomes, safety, and quality of life via the SF 36 questionnaire following POEM in a tertiary care endoscopy unit with trainee involvement. There is no report on how to train trainees in this particular procedure. There are limited data on the safety and efficacy of POEM in an endoscopy unit performed by gastroenterologists [9, 16] and no data on the experience of POEM performed with trainees. Very few studies have reported validated Quality of Life inventories improvement with POEM (22/25). In the current study, we report using key points in each step of the POEM procedure to assess the trainees’ performance and the outcomes of POEM performed in an endoscopy unit with trainees. Trainees are experienced endoscopists, training to recognize the anatomy and orientation inside the submucosal tunnel in the esophagus, which is the most important issue, rather than timing the procedure, in training with this special procedure. To our knowledge, this is the first report of how to train trainees in POEM procedure and the outcomes of POEM performed with trainee involvement.
Trainees can be trained on animal models or cadavers. Trainees can be trained by performing a few proctored cases with an experienced endoscopist. The short-term training may not be sufficient and it tends to have relatively higher complications with the first 20 cases of POEM (Personal communication by Dr. Qiang Cai with POEM experts in Asia). One published paper suggested that a possible training process might first involve observation of POEM performed by specialists, then training on non-survival and survival porcine models, followed by training in humans under specialist guidance and finally, performance of POEM in humans. However, it is only a suggestion and the paper did not provide any data to support this suggestion [23]. One study on 40 patients suggested mastery of operative technique in POEM is evidenced by a decrease in length of operation, variability of minutes per centimeter of myotomy, and incidence of inadvertent mucosotomies and plateaus in about 20 cases for experienced endoscopists. The study also suggested that the learning curve can be shortened with very close supervision and/or proctoring, but did not show how to supervise and/or proctor [24]. However, another study on 36 patients showed that overall procedure time did not decrease with experience and may not be an important marker of procedural skill for POEM [25]. A more recently study showed efficiency was attained after 40 POEMs and mastery after 60 POEMs, but did not mention the minimal numbers for trainees to be able to perform POEM alone [26].
Therefore, based on those spare information, there is no protocol on how to train trainees performing POEM. Since POEM is a unique endoscopic procedure and learners are usually experienced endoscopists, training process should be unique and how to access the competency should be different as well. The important things in performing POEM are to identify the anatomy, such as the mucosal layer, the muscular layer, and the gastrointestinal junction. Our study showed trainees, without experience in animal models or cadavers, performing POEM procedure step by step with an experienced mentor was safe and did not see any adverse events, such as inadvertent mucosotomies. Since making an incision to establish the entrance of a submucosal tunnel is an important/difficult step of the procedure, and any injury or perforation at this step may force earlier termination of the procedure, trainees should learn this step at the end of their training. In our experience, trainees should learn how to perform POEM in a step-by-step fashion, beginning with submucosal dissection, establish a sub mucosal tunnel; to myotomy; to making an initial incision to creating an entrance into the submucosal tunnel, prior to performing an entire procedure. Based on our experience from this study, a minimum of 20 cases will be needed to perform POEM independently.
In addition to the step-by-step training process, the outcomes of the study with trainees are similar to that of other studies without trainees. Our study included patients who underwent prior botulinum injection (37%), pneumatic balloon dilatation (8%), and surgical myotomy (6%). In the present series, more than 90% of patients maintained an Eckardt score of ≤ 3 at 1-year follow-up. Symptoms recurred in four patients after POEM. Post POEM acid reflux needing continuation of PPI was seen in 8/62 (12.9%) of patients.
As described by authors in prior studies, performing POEM in endoscopy units is advantageous in many fronts, such as ergonomic design, familiar environment, ready availability of various trained personnel and equipment, less cumbersome than performing in operating room, time saving, and economic [9, 16] Our current series also confirms the safety profile of POEM performed by expert endoscopists in an endoscopy unit. There were no occurrences of mucosal injury or postoperative leaks. The explanation for no mucosal injury in this study could be the advantage of the step-by-step training in the study and trainees recognized the anatomy better under the tutoring of the mentor.
Few studies have reported positive improvement in QOL after POEM [27, 28]. In this study, we collected short form SF-36 QOL improvement data in patients undergoing POEM. Significantly, we have noticed an improvement in several domains of QOL assessment within 1 month after POEM. In our series, six domains of QOL assessment (by SF-36 from) have shown significant improvement post POEM. The improvement in scores in general health, vitality, social functioning, and role limitation due to emotional problems is likely due to positively impacting eating habits, improving nutrition status, and emotional well-being [27]. Moreover, this explains the emotional component of suffering from achalasia besides dysphagia and chest pain as seen in a prior study [27]. Importantly, improvement in vitality contributes to overall well-being. It is not surprising to see any improvement in physical functioning and role limitation due to physical health as these are not related achalasia symptoms. QOL assessment with LHM has shown an improvement in vitality or energy/fatigue, mental health or emotional well-being, and general health only but has not shown an improvement in social functioning and role limitation due to emotional problems [29, 30]. Our study concurs with prior reported improvement in both domains with POEM. These data reinforces the positive impact of POEM in patients with achalasia [27].
Limitation of the present study is its retrospective evaluation in a single center with 4 trainees without any comparison groups. Although we perform symptom assessment and EGD if it was indicated, we do not routinely perform pH studies for the assessment of gastroesophageal reflux disease (GERD) on all post POEM patients as is being done in some centers; thus, we do not have the true estimate of GERD post POEM.
In conclusion, despite some limitations, this is the first report on how to train trainees in performing POEM, via step-by-step assessment of key points in each step to judge the competency of this unique endoscopic procedure and the threshold number for trainees to perform POEM independently is around 20 cases. In our experience, performing POEM with trainees is feasible, safe, and has excellent outcomes in a well-equipped modern endoscopy suite under general anesthesia. The items listed in the check list could be used as an important guide in training POEM. More studies, especially multiple center studies, are needed to establish a standard protocol for trainees to learn how to perform POEM.
References
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1249 (quiz 1250)
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR, European Achalasia Trial Investigation (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia Lancet 383:83–93
Khashab MA, Saxena P, Kumbhari V, Nandwani M, Roland BC, Stein E, Clarke JO, Stavropoulos S, Inoue H, Pasricha PJ (2014) Peroral endoscopic myotomy as a platform for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc 79:136–139
Rohof WO, Salvador R, Annese V, Bruley des Varannes S, Chaussade S, Costantini M, Elizalde JI, Gaudric M, Smout AJ, Tack J, Busch OR, Zaninotto G, Boeckxstaens GE (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144:718–725 (quiz e713–e714)
Vaezi MF, Baker ME, Achkar E, Richter JE (2002) Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 50:765–770
Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, Baker ME, Rice TW (2006) The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 4:580–587
Khashab MA, El Zein M, Kumbhari V, Besharati S, Ngamruengphong S, Messallam A, Abdelgalil A, Saxena P, Tieu AH, Raja S, Stein E, Dhalla S, Garcia P, Singh VK, Pasricha PJ, Kalloo AN, Clarke JO (2016) Comprehensive analysis of efficacy and safety of peroral endoscopic myotomy performed by a gastroenterologist in the endoscopy unit: a single-center experience. Gastrointest Endosc 83:117–125
Stavropoulos SN, Modayil RJ, Friedel D, Savides T (2013) The international per oral endoscopic myotomy survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc 27:3322–3338
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264
Ramchandani M, Nageshwar Reddy D, Darisetty S, Kotla R, Chavan R, Kalpala R, Galasso D, Lakhtakia S, Rao GV (2016) Peroral endoscopic myotomy for achalasia cardia: treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc 28:19–26
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256:659–667
Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G (2016) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg 263:82–87
Yang D, Pannu D, Zhang Q, White JD, Draganov PV (2015) Evaluation of anesthesia management, feasibility and efficacy of peroral endoscopic myotomy (POEM) for achalasia performed in the endoscopy unit. Endosc Int Open 3::E289–E295
Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39:761–764
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ (2008) Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526–1533
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Philips GM, Dacha S, Keilin SA, Willingham FF, Cai Q (2016) Concurrent myotomy and tunneling after establishment of a half tunnel instead of myotomy after establishment of a full tunnel: a more efficient method of peroral endoscopic myotomy. Endosc Int Open 4::E403–E408
Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, Swanstrom LL, Vassiliou MC (2014) Per-oral endoscopic myotomy white paper summary. Surg Endosc 28:2005–2019
Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, Maselli R, Kudo SE (2012) Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag 8:329–342
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77:719–725
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES (2014) Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 18:92–98 (discussion 98–99)
Patel KS, Calixte R, Modayil RJ, Friedel D, Brathwaite CE, Stavropoulos SN (2015) The light at the end of the tunnel: a single-operator learning curve analysis for per oral endoscopic myotomy. Gastrointest Endosc 81:1181–1187
Vigneswaran Y, Tanaka R, Gitelis M, Carbray J, Ujiki MB (2015) Quality of life assessment after peroral endoscopic myotomy. Surg Endosc 29:1198–1202
Liu XJ, Tan YY, Yang RQ, Duan TY, Zhou JF, Zhou XL, Liu DL (2015) The outcomes and quality of life of patients with achalasia after peroral endoscopic myotomy in the short-term. Ann Thorac Cardiovasc Surg 21:507–512
Youssef Y, Richards WO, Sharp K, Holzman M, Sekhar N, Kaiser J, Torquati A (2007) Relief of dysphagia after laparoscopic Heller myotomy improves long-term quality of life. J Gastrointest Surg 11:309–313
Katilius M, Velanovich V (2001) Heller myotomy for achalasia: quality of life comparison of laparoscopic and open approaches. JSLS 5:227–231
Author information
Authors and Affiliations
Contributions
SD: obtaining IRB approval, collection and interpretation of data, drafting and revision of the article; LW: conception and revision of the article; GP: collection of data and revision of the article; XL, YJ, SAK, FFW: revision of the article; QC: Performing all procedures, obtaining IRB approval, conception and the design of the study, revision of the article.
Corresponding author
Ethics declarations
Disclosures
Sunil Dacha, Lei Wang, Xaioyu Li, Yueping Jiang, George Philips, Steven A Keilin, Field F Willingham, Qiang Cai have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Dacha, S., Wang, L., Li, X. et al. Outcomes and quality of life assessment after per oral endoscopic myotomy (POEM) performed in the endoscopy unit with trainees. Surg Endosc 32, 3046–3054 (2018). https://doi.org/10.1007/s00464-017-6015-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-6015-x