Abstract
Background
Laparoscopic (laparoscopy-assisted) gastrectomy (LG) has several short-term benefits as compared with open distal gastrectomy (OG) in patients with advanced gastric cancer (AGC). Survival rates did not differ significantly between LG and OG in retrospective studies of AGC, although some studies included unmatched groups of patients or patients with AGC who had a preoperative diagnosis of early gastric cancer. The aim of present study was to compare the short- and long-term outcomes of patients with AGC who underwent LG with those of patients with AGC who underwent OG using a propensity-score matching analysis.
Methods
The study group comprised patients with a preoperative and pathologically confirmed diagnosis of AGC who underwent LG or OG with lymphadenectomy between January 2001 and December 2012 in our hospital. To minimize bias between the LG and OG groups, propensity scores were calculated using a logistic regression model and the following variables: sex, age, body-mass index, American Society of Anesthesiologists physical status class, type of gastrectomy, and clinical and pathological tumor stage. After propensity-score matching, 104 patients (52 who underwent LG and 52 who underwent OG) were studied.
Results
LG was associated with significantly earlier initiation of food intake (p <0.01) and a significantly shorter period of postoperative hospitalization (p <0.01). The incidence of all-grade overall, surgical, and medical complications did not differ significantly between the LG group and OG group (p = 0.24, p = 0.12, and p >0.99). Overall and relapse-free survival also did not differ between the LG group and OG group (p = 0.96, p = 0.91). In each tumor stage, overall and relapse-free survival did not differ significantly between the LG group and OG group.
Conclusion
LG can be a feasible treatment that is beneficial in terms of earlier recovery after operation and can be expected to result in similar survival as OG in patients with AGC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic (laparoscopy-assisted) gastrectomy (LG) is an established minimally invasive treatment for gastric cancer (GC), especially early-stage GC. The short-term benefits of LG, such as less operative bleeding, less pain, earlier bowel movement, and shorter hospitalization, have also been demonstrated in large randomized controlled trials (RCT) comparing laparoscopic distal gastrectomy (LDG) with open distal gastrectomy (ODG) [1, 2]. Similar advantages of laparoscopic total gastrectomy (LTG) were also shown by retrospective studies comparing LTG with open total gastrectomy (OTG), although definitive evidence supporting the usefulness of LTG is still lacking; prospective studies are ongoing [3,4,5]. As for the evaluation of postoperative complications, large RCTs of LDG versus ODG in early-stage GC obtained somewhat different outcomes. One study reported similar incidences of complications after LDG and ODG, while another study showed that LDG is associated with significantly lower incidences of overall postoperative complications and wound problems [1, 6]. LTG decreased wound-related problems in case-matched studies or an updated meta-analysis, although anastomotic problems were more common in LTG than in OTG [7,8,9]. In patients with advanced GC (AGC), the aforementioned short-term benefits of LG were shown in RCTs, meta-analyses including retrospective comparative studies, and case-matched studies [2, 10,11,12,13,14]. RCTs reported similar incidences of postoperative complications for LG and OG [2, 10]. However, one RCT showed that anastomotic leakage was slightly more frequent in LDG than in ODG [2]. As for long-term outcomes, a small RCT and meta-analyses in patients with AGC revealed that overall survival did not differ between LG and OG [10,11,12]. However, some studies included in the meta-analyses compared unmatched groups of patients [11, 12]. Similar results were also obtained in case-matched studies [14, 15]. Ongoing RCTs of AGC will most likely clarify survival after LDG, but definitive evidence on survival has yet to be obtained [2, 16].
As for another issue, patients who have pathological AGC with a preoperative diagnosis of early GC might not be treated by D2 lymphadenectomy. Nonetheless, such patients have favorable survival [17, 18]. Patients with such AGCs were most likely included in some retrospective studies of pathological AGC. On the other hand, RCTs of AGC had included some patients with pathological early GC, because the clinical diagnosis of advanced or early disease is not always certain. Therefore, clinical and pathological AGC should be evaluated in a study of AGC.
The aim of present study was to evaluate short-term benefits and long-term survival in patients with clinical and pathological AGC who underwent LG, as compared with a matched group of patients who underwent OG.
Patients and methods
We initially screened our prospective database of gastric cancer and identified patients with preoperative and pathological diagnoses of AGC who underwent LG or OG with lymphadenectomy between January 2001 and December 2012 in our hospital. All patients were given a sufficient explanation, and written, informed consent was obtained. This study was approved by the Ethics Committee of Tokyo Medical and Dental University. We have performed LG in patients with AGC since 2001. Patients who met any of the following criteria were excluded from the study: (1) a type 4 or large type 3 tumor (more than 8 cm in diameter on preoperative examination); (2) bulky lymphatic metastases (more than 3 cm in diameter) along the celiac, splenic, common hepatic, or proper hepatic artery; (3) neoadjuvant chemotherapy; (4) stage IV disease; (5) non-curative resection (R1/R2); (6) other advanced malignancy; (7) emergency operation; (8) concurrent resection of the pancreas or colon; or (9) pathologically special types. A total of 73 patients who underwent LG and 196 patients who underwent OG were identified. Whether to perform LG or OG was based on the tumor stage in principle, because Japanese treatment guidelines [19] or community consensus had recommended that LG should be used to treat clinical stage I gastric cancer. However, some patients with a clinical diagnosis of AGC underwent LG because they directly requested a laparoscopic approach or were enrolled in clinical trials after obtaining well-informed consent. Therefore, LG was used to treat early-stage gastric cancer, while OG was mainly done in patients with advanced disease. We performed propensity-score matching to minimize bias between the two groups of patients. Propensity scores were calculated using a logistic regression model and the following variables: sex, age (younger than 65 years or not), body-mass index (BMI, less than 30 or not), ASA-PS class, type of gastrectomy (distal gastrectomy, total gastrectomy, or total gastrectomy with splenectomy), clinical stage (IB, II, or III), and pathological tumor stage (IB, IIA, IIIA, IIIB, or IIIC). Patients were individually matched between the LG and OG groups using the nearest-neighbor-matching method. This method consists of randomly ordering the case and control subjects, selecting the first case subject, and then finding the control subject with the closest propensity score rounded to two decimal places. Finally, 104 patients (52 who underwent LG and 52 who underwent OG) were matched by this method.
The following variables were obtained from our prospective gastric cancer database: patient age and gender; comorbidities; American Society of Anesthesiologists physical status (ASA-PS); tumor characteristics; operation time; estimated blood loss; extent of lymph-node dissection; number of harvested lymph nodes; and postoperative outcomes. Clinical pathways for perioperative management were applied to various types of gastrectomy in our institution since 2004. Postoperative schedules were slightly revised three times during the period of this study. Oral intake was started after confirmation of flatus until 2003, and it was scheduled earlier regardless of flatus status after application of the clinical pathways. However, oral intake was always scheduled 1 day earlier in LG than in OG, based on the results of an initial study comparing LDG with ODG [20]. Discharge from the hospital was scheduled 1 day earlier in LG than in OG. Postoperative complications that occurred within 30 days after gastrectomy were defined by the Clavien-Dindo classification [21]. Moreover, postoperative complications were classified into either surgical (abdominal) or medical (non-abdominal) complications. Tumors were pathologically classified in accordance with the Japanese Classification of Gastric Carcinoma, 3rd English edition [22]. Papillary or tubular adenocarcinomas were classified as differentiated adenocarcinomas, and poorly differentiated, signet-ring cell, or mucinous adenocarcinomas were classified as undifferentiated adenocarcinomas in accordance with the histological classification of the World Health Organization. D2 lymphadenectomy was performed in patients who had AGC diagnosed preoperatively in accordance with the treatment guidelines of the Japanese Gastric Cancer Association [21]. However, splenectomy or No. 10 lymphadenectomy was omitted in patients who had proximal gastric cancer (except for tumors that invaded the greater curvature, or tumors accompanied by metastasis to the No. 10 or 11 lymph nodes). Both LG and OG were performed by the same 6 surgeons, who were certified by both the Japan Society for Endoscopic Surgery (from 2005) and the Japanese Society of Gastroenterological Surgery and served as operators or instructive assistants.
The following short-term outcomes after gastrectomy were compared between the LG group and OG group: operative time, estimated blood loss, number of harvested lymph nodes, time to food intake, postoperative hospital stay, and postoperative complications. To assess long-term outcomes, overall and disease-free survival rates were evaluated in the LG group and OG group and compared between the groups.
Statistical analysis
Categorical data were compared with the use of the χ2 test or Fisher’s exact test, as appropriate. The Mann–Whitney test was used to compare continuous variables. Survival was assessed on the basis of the length of overall survival (OS) and relapse-free survival (RFS). Survival curves were plotted by the Kaplan–Meier method and were compared by means of the log-rank test. Values of p <0.05 were considered to indicate statistical significance. All analyses were performed with the statistical software package SPSS 24 (SPSS Japan Inc., Tokyo, Japan).
Results
The clinical characteristics and tumor status of the patients are summarized in Table 1. No statistically significant differences were found between the LG group and OG group in any background characteristic, including age, sex, BMI, ASA physical status classification, and clinical or pathological stage according to the TNM classification. Surgical outcomes are shown in Table 2. The number of harvested lymph nodes did not differ significantly between the two groups. The operating time was significantly longer in the LG group than in the OG group (median time: 316 vs. 242 min, p <0.01), whereas the estimated blood loss was significantly lower in the LG group than in the OG group (median volume: 115 vs. 420 ml, p <0.01). LG significantly hastened the time to starting food intake (median postoperative day 2 vs. 4, p <0.01) and shortened the postoperative hospital stay as compared with OG (median, 9 days vs. 12 days, p <0.01). Postoperative complications are summarized in Table 3. The incidences of all-grade overall, surgical, and medical complications did not differ significantly between the LG group and OG group (17 vs. 27%, p = 0.24; 12 vs. 24%, p = 0.12; 8 vs. 10%, p >0.99; respectively). Severe overall, surgical, and medical complications were similar in the two groups (15 vs. 12%, p = 0.57; 12 vs. 12%, p >0.99; 4 vs. 4%, p >0.99; respectively). Individual complications, such as anastomotic leakage, abdominal abscess, cardiac complications, and pulmonary complications, also did not differ significantly between the groups.
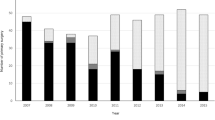
The median follow-up was 62.2 months (range 1.2–149.4) in the study group as a whole and 62.2 months in each group (range 2.8–149.4 in the LG group; 4.4–130.4 in the OG group). The survival curves are shown in Fig. 1. OS and RFS did not differ significantly between the LG group and OG group (p = 0.96, p = 0.91, respectively). The 5-year OS rate was 70% in the LG group and 73% in the OG group, and the 5-year RFS rate was 69% in the LG group and 71% in the OG group. OS and RFS did not differ significantly between the LG group and OG group in stage II disease (5-year OS, 80 vs. 75%, p >0.99; 5-year RFS, 76 vs. 76%, p = 0.90) or stage III disease (63 vs. 58%, p = 0.40; 64 vs. 58%, p = 0.42, respectively). In stage IB disease, only 1 of 6 patients had recurrent disease in the LG group, while none of 6 patients had recurrent disease in the OG group.
Discussion
The results of this retrospective study suggest that LG might be a promising treatment for clinical and pathological AGC in terms of short-term and long-term outcomes. The survival of patients with AGC who undergo LDG is expected to be accurately evaluated by ongoing RCTs, although survival after LTG will remain unclear. OS and RFS did not differ significantly between LG and OG in meta-analyses of retrospective studies of patients with AGC, although such analyses included unmatched studies, stage IV disease, insufficient lymphadenectomy, or insufficient follow-up periods [11, 12]. One small RCT and two retrospective case-matched studies of AGC showed no significant difference in overall survival between LG and OG [10, 14, 15]. Similar survival was also reported by retrospective studies in patients with AGC who underwent gastrectomy [23,24,25,26,27]. Our results are consistent with the findings of previous studies, although the present study included only patients who had clinical and pathological diagnoses of locally AGC, as well as some patients who underwent concurrent splenectomy. No specific recurrence pattern was reported by a previous multi-institutional case-series [28]. In a Western study comparing LG with OG, overall and recurrence-free survival did not differ significantly, although early-stage cancers were partly included [29]. As compared with our study, the Western study had higher proportions of female patients (48 vs. 27%), patients who underwent total gastrectomy (32 vs. 17%), and patients who received neoadjuvant treatment (30 vs. 0%).
Our study showed earlier resumption of oral intake and earlier discharge in LG than in OG, and these results are supported by the findings of previous studies of AGC [10,11,12,13,14]. However, enhanced recovery after surgery (ERAS) was not applied in the present study, and the postoperative schedule, including oral intake and discharge, differed between LG and OG, based on an earlier study comparing LDG with ODG [20]. The initiation of oral intake was delayed more frequently in OG than in LG in the present study, and the main reason was that the attending surgeons were concerned about poor bowel movement after OG. In addition to postoperative complications, another reason for delayed discharge after OG was anxiety or requests by the patients or their families. Postoperative complications did not differ significantly between LG and OG in our study, while the outcomes differed somewhat from those in other studies of AGC. Postoperative complications did not differ between LG an OG in a previous RCT, although LG significantly reduced the incidence of pneumonia or wound infection [10, 13]. The incidences of both major and minor complications were similar after LG and OG in one case-matched study [14]. In meta-analyses of LG and OG that included retrospective studies, overall postoperative complications were significantly reduced by LG [11, 12]. As for specific complications, wound-related problems and pneumonia were significantly decreased by LG in a meta-analysis [12]. However, these meta-analyses included studies in which the LG and OG groups were unmatched. In a RCT of distal gastrectomy for AGC, there were no significant differences in overall, surgical, or medical complications between LDG and ODG, although LDG was associated with increased anastomotic leakage [2].
Although the present study compared LG with OG in case-matched groups of patients, it was small and performed in a single institution. In addition, we generally complied with the treatment guidelines of the Japanese Gastric Cancer Association, in which LG is considered an experimental treatment for clinical stage I GC. Because tumor-related bias most likely affected the characteristics of patients who underwent LG or OG in our hospital, propensity-score matching was essential to ensure that matched groups of patients were compared. Instead of minimizing bias between the two groups, many patients who underwent OG were excluded from the present study after matching. Patients who had type 4 or large type 3 GC or GC with bulky lymphatic metastases, characteristics associated with very poor prognoses, were excluded from the present study because such patients would receive intensive neoadjuvant chemotherapy in the Japanese medical community. Large diffuse-type GC is probably a risk factor for tumor-positive surgical margins; therefore, the exclusion of patients with large diffuse-type GC most likely resulted in the exclusion of patients with tumor-positive surgical margins from the present study. Intraoperative pathological investigations were performed in patients with short surgical margins in our institution. Only one patient in the OG group was excluded from the present study solely because of tumor-positive surgical margins, and no patient was excluded because of this reason in the LG group. However, a previous study reported a higher rate of tumor-positive margins after LG than after OG [29]. The operative era could also have a considerable impact on survival after gastrectomy, because patients have routinely received postoperative adjuvant therapy with S-1 as standard treatment since the end of 2006. Therefore, we matched the study groups according to whether they were treated before or after 2007. Severe postoperative complications, comorbidity, or an advanced age had an impact on whether or not patients received postoperative adjuvant chemotherapy. Postoperative adjuvant chemotherapy was not included as an adjustment factor for the propensity scores in the present study, although the proportions of patients who received adjuvant chemotherapy were nearly the same in the LG group and OG group. Another problem was that the experience of the surgeon who performed the operation might have had an impact on surgical outcomes. Anastomotic complications are likely to be affected by the surgeon’s experience with LTG (i.e., the numbers of such operations performed) [30]. However, operator-related bias might have been minimal in our study because both LG and OG were performed by board-certificated surgeons who had adequate experience as operators or instructive assistants. Accomplishment of LDG with D2 lymphadenectomy in about 40 patients was required to achieve significant effects on most of the important surgical and short-term recovery outcomes in a meta-analysis [31]. Experience with 45 patients was required to reduce postoperative complications in a LTG study [30], whereas experience with 100 patients was required to stabilize operative time or estimated bleeding in another LTG study [32].
As mentioned above, different postoperative schedules between LG and OG were a critical problem in the present study, although such differences would be irrelevant to long-term survival. ERAS was not applied in the present study because it was recommended as a beneficial procedure after gastrectomy in 2014 [33].
In conclusion, as compared with OG, LG can be a feasible treatment that is beneficial in terms of earlier recovery after operation and is expected to result in similar survival in patients with AGC.
References
Katai H, Mizusawa J, Katayama H, Takagi M, Yoshikawa T, Fukagawa T, Terashima M, Misawa K, Teshima S, Koeda K, Nunobe S, Fukushima N, Yasuda T, Asao Y, Fujiwara Y, Sasako M (2016) Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer 20:699–708
Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, Xue Y, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Chen P, Liu H, Zheng C, Liu F, Yu J, Li Z, Zhao G, Chen X, Wang K, Li P, Xing J, Li G (2016) Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol 34:1350–1357
Chen K, Xu XW, Zhang RC, Pan Y, Wu D, Mou YP (2013) Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World J Gastroenterol 19:5365–5376
Wang W, Zhang X, Shen C, Zhi X, Wang B, Xu Z (2014) Laparoscopic versus open total gastrectomy for gastric cancer: an updated meta-analysis. PLoS ONE 18:e88753
Kataoka K, Katai H, Mizusawa J, Katayama H, Nakamura K, Morita S, Yoshikawa T, Ito S, Kinoshita T, Fukagawa T, Sasako M, Stomach Cancer Study Group/Japan Clinical Oncology Group (2016) Non-randomized confirmatory trial of laparoscopy-assisted total gastrectomy and proximal gastrectomy with nodal dissection for clinical stage i gastric cancer: Japan Clinical Oncology Group Study JCOG1401. J Gastric Cancer 16:93–97
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee HJ, Korean Laparo-endoscopic Gastrointestinal Surgery Study (KLASS) Group (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg 263:28–35
Jeong O, Jung MR, Kim GY, Kim HS, Ryu SY, Park YK (2013) Comparison of short-term surgical outcomes between laparoscopic and open total gastrectomy for gastric carcinoma: case-control study using propensity score matching method. J Am Coll Surg 216:184–191
Lee JH, Nam BH, Ryu KW, Ryu SY, Park YK, Kim S, Kim YW (2015) Comparison of outcomes after laparoscopy-assisted and open total gastrectomy for early gastric cancer. Br J Surg 102:1500–1505
Inokuchi M, Otsuki S, Ogawa N, Tanioka T, Okuno K, Gokita K, Kawano T, Kojima K (2016) Postoperative complications of laparoscopic total gastrectomy versus open total gastrectomy for gastric cancer in a meta-analysis of high-quality case-controlled studies. Gastroenterol Res Pract 2016:2617903
Cai J, Wei D, Gao CF, Zhang CS, Zhang H, Zhao T (2011) A prospective randomized study comparing open versus laparoscopy-assisted D2 radical gastrectomy in advanced gastric cancer. Dig Surg 28:331–337
Quan Y, Huang A, Ye M, Xu M, Zhuang B, Zhang P, Yu B, Min Z (2016) Comparison of laparoscopic versus open gastrectomy for advanced gastric cancer: an updated meta-analysis. Gastric Cancer 19:939–950
Zou ZH, Zhao LY, Mou TY, Hu YF, Yu J, Liu H, Chen H, Wu JM, An SL, Li GX (2014) Laparoscopic vs open D2 gastrectomy for locally advanced gastric cancer: a meta-analysis. World J Gastroenterol 20:16750–16764
Li Q, Wang J, Zhang G, Wang J, Yang B, Zhang Z (2016) Feasibility and safety comparison of laparoscopy-assisted versus open gastrectomy for advanced gastric carcinoma with D2 lymphadenectomy. Jpn J Clin Oncol 46:323–328
Kim KH, Kim YM, Kim MC, Jung GJ (2013) Is laparoscopy-assisted total gastrectomy feasible for the treatment of gastric cancer? A case-matched study. Dig Surg 30:348–354
Lin JX, Huang CM, Zheng CH, Li P, Xie JW, Wang JB, Jun L, Chen QY, Cao LL, Lin M (2016) Is all advanced gastric cancer suitable for laparoscopy-assisted gastrectomy with extended lymphadenectomy? A case-control study using a propensity score method. Ann Surg Oncol 23:1252–1260
Inaki N, Etoh T, Ohyama T, Uchiyama K, Katada N, Koeda K, Yoshida K, Takagane A, Kojima K, Sakuramoto S, Shiraishi N, Kitano S (2015) A multi-institutional, prospective, phase ii feasibility study of laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for locally advanced gastric cancer (JLSSG0901). World J Surg 39:2734–2741
Kimura A, Ogata K, Kogure N, Yanoma T, Suzuki M, Toyomasu Y, Ohno T, Mochiki E, Kuwano H (2016) Outcome of laparoscopic gastrectomy with D1 plus lymph node dissection in gastric cancer patients postoperatively diagnosed with locally advanced disease or lymph node metastasis. Surg Endosc 30:2090–2096
Tokunaga M, Hiki N, Fukunaga T, Ohyama S, Yamada K, Yamaguchi T (2009) Better prognosis of T2 gastric cancer with preoperative diagnosis of early gastric cancer. Ann Surg Oncol 16:1514–1519
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S (2000) Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg 135:806–810
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd english edition. Gastric Cancer 14:101–112
Hao Y, Yu P, Qian F, Zhao Y, Shi Y, Tang B, Zeng D, Zhang C (2016) Comparison of laparoscopy-assisted and open radical gastrectomy for advanced gastric cancer: a retrospective study in a single minimally invasive surgery center. Medicine 95:e3936
Hur H, Jeon HM, Kim W (2008) Laparoscopy-assisted distal gastrectomy with D2 lymphadenectomy for T2b advanced gastric cancers: three years’ experience. J Surg Oncol 98:515–519
Scatizzi M, Kröning KC, Lenzi E, Moraldi L, Cantafio S, Feroci F (2011) Laparoscopic versus open distal gastrectomy for locally advanced gastric cancer: a case-control study. Updates Surg 63:17–23
Zhao Y, Yu P, Hao Y, Qian F, Tang B, Shi Y, Luo H, Zhang Y (2011) Comparison of outcomes for laparoscopically assisted and open radical distal gastrectomy with lymphadenectomy for advanced gastric cancer. Surg Endosc 25:2960–2966
Zhang Y, Qi F, Jiang Y, Zhai H, Ji Y (2015) Long-term follow-up after laparoscopic versus open distal gastrectomy for advanced gastric cancer. Int J Clin Exp Med 8:13564–13570
Park DJ, Han SU, Hyung WJ, Kim MC, Kim W, Ryu SY, Ryu SW, Song KY, Lee HJ, Cho GS, Kim HH, Korean Laparoscopic Gastrointestinal Surgery Study (KLASS) Group (2012) Long-term outcomes after laparoscopy-assisted gastrectomy for advanced gastric cancer: a large-scale multicenter retrospective study. Surg Endosc 26:1548–1553
Kelly KJ, Selby L, Chou JF, Dukleska K, Capanu M, Coit DG, Brennan MF, Strong VE (2015) Laparoscopic versus open gastrectomy for gastric adenocarcinoma in the west: a case-control study. Ann Surg Oncol 22:3590–3596
Jeong O, Ryu SY, Choi WY, Piao Z, Park YK (2014) Risk factors and learning curve associated with postoperative morbidity of laparoscopic total gastrectomy for gastric carcinoma. Ann Surg Oncol 21:2994–3001
Zhou D, Quan Z, Wang J, Zhao M, Yang Y (2014) Laparoscopic-assisted versus open distal gastrectomy with D2 lymph node resection for advanced gastric cancer: effect of learning curve on short-term outcomes. a meta-analysis. J Laparoendosc Adv Surg Tech A 24:139–150
Jung DH, Son SY, Park YS, Shin DJ, Ahn HS, Ahn SH, Park DJ, Kim HH (2016) The learning curve associated with laparoscopic total gastrectomy. Gastric Cancer 19:264–272
Mortensen K, Nilsson M, Slim K, Schäfer M, Mariette C, Braga M, Carli F, Demartines N, Griffin SM, Lassen K (2014) Consensus guidelines for enhanced recovery after gastrectomy: enhanced recovery after surgery (ERAS®) society recommendations. Br J Surg 101:1209–1229
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mikito Inokuchi, Masatoshi Nakagawa, Toshiro Tanioka, Keisuke Okuno, Kentaro Gokita, and Kazuyuki Kojima have declared no conflicts of interest or financial ties to disclosure.
Rights and permissions
About this article
Cite this article
Inokuchi, M., Nakagawa, M., Tanioka, T. et al. Long- and short-term outcomes of laparoscopic gastrectomy versus open gastrectomy in patients with clinically and pathological locally advanced gastric cancer: a propensity-score matching analysis. Surg Endosc 32, 735–742 (2018). https://doi.org/10.1007/s00464-017-5730-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5730-7