Abstract
Background
This study retrospectively compared the safety and efficacy of two endoscopic techniques for treating newly diagnosed achalasia, pneumatic dilation (PD), and peroral endoscopic myotomy (POEM).
Methods
Demographics, clinical and manometric data, and outcomes were collected from the medical records of patients who received POEM or PD as the primary therapy for achalasia at our hospital from January 2012 to August 2015.
Results
Of 72 patients, 32 and 40 received POEM and PD, respectively. The two groups had similar preoperative features. On short-term follow-up, improvements in high-resolution esophageal manometry and barium esophagogram parameters were similar. For PD, the success rates at 3, 6, 12, 24, and 36 months were 95, 88, 75, 72, and 60%, respectively. For POEM, these were 96, 96, 96, 93, and 93% (P = 0.013, log-rank test). On subgroup analysis, the success rate was higher with POEM than that with PD in all 3 manometric subtypes, but only that of type III was statistically significant. POEM required significantly longer operative time and hospitalization than did PD (P < 0.001). Four POEM patients experienced subcutaneous emphysema. The rate of gastroesophageal reflux was higher in patients treated by POEM (18.8%) than that in PD (10%; P = 0.286).
Conclusions
In the intermediate term, the remission rate of symptoms associated with POEM therapy was better than that with PD for newly diagnosed achalasia, especially in patients with type III achalasia. The short-term outcomes of the two therapies were similar.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achalasia is a rare motility disorder of the esophagus, with an estimated annual incidence of one in every 100,000 people [1] with substantial impairment of health-related quality of life [2]. Achalasia is characterized by the absence of peristalsis and a defective relaxation of the lower esophageal sphincter (LES), resulting in impaired bolus transport and stasis of food in the esophagus. The main clinical features of achalasia include dysphagia, regurgitation, retrosternal pain, and weight loss.
Since the pathogenesis of achalasia is not well understood, the main goal of treatment is palliative and aimed at improving esophageal outlet obstruction. Therapeutic options include medical treatment, endoscopic pneumatic dilation (PD), botulinum toxin injection, and laparoscopic Heller myotomy (LHM). The effect of pharmacotherapy and botulinum toxin injection is short-lived. LHM provides the most long lasting improvement in symptoms, but elderly patients and patients with multiple comorbidities are not suitable [3, 4]. PD is a simple, low-cost treatment, but is associated with a higher relapse rate [4, 5].
Peroral endoscopic myotomy (POEM) is the latest breakthrough in minimally invasive endoscopic therapy for achalasia and has been rapidly accepted worldwide [6, 7]. POEM has the advantages: inherent in an endoscopic procedure, the precision of a surgical myotomy [8, 9], and its safety and effectiveness for treating achalasia have been demonstrated [10, 11]. Several studies have shown that the short-term outcomes of POEM are comparable to LHM [12,13,14]. In addition, previous studies have suggested that the manometric subtypes of achalasia may predict the results of treatment and help in determining the appropriate treatment modality [15, 16].
The most suitable treatment for achalasia with good long-term results remains undecided. While POEM and PD are both endoscopic therapies, very few studies have compared their safety and efficacy, and it is still unknown to what extent the choice of treatment can be guided by the manometric subtype [17]. We conducted this retrospective study to compare the efficacy and safety of PD and POEM for newly diagnosed achalasia and to assess whether the manometric subtype can dictate the choice of treatment.
Materials and methods
The Institutional Review Board of Beijing Friendship Hospital, Capital Medical University, approved this study.
Subjects
All achalasia patients who underwent endoscopic treatment in our department between January 2012 and August 2015 were retrospectively identified. Patients were counseled regarding the existing treatment options (PD, POEM, and LHM), after which they decided whether to undergo PD or POEM. Each patient provided signed written consent for the procedure and data collection.
Demographics and clinical data of the patients were prospectively collected. The diagnosis and disease subtype was based on clinical symptoms, upper gastrointestinal endoscopy, barium esophagogram, and high-resolution esophageal manometry (HREM). All the patients underwent computed tomography (CT) and endoscopic ultrasonography for exclusion of secondary achalasia. The inclusion criteria were: age between 18 and 75 years and receiving POEM or PD as an initial treatment. Patients with any of the following were excluded: previous endoscopic treatment or surgery for achalasia; esophageal diameter more than 7 cm; esophageal diverticulum in the distal esophagus; and duration of follow-up less than 12 months.
Evaluation of symptoms
The Eckardt score was used for objective evaluation of the patient’s symptoms [18]. The Eckardt score is the sum of the symptom scores for dysphagia, regurgitation, chest pain, and weight loss, each on a scale of 0–3, resulting in a total scale of 0–12 with higher scores indicating more severe disease.
Barium esophagogram
Every patient had a barium esophagogram before PD or POEM, to measure the diameter of the esophagus. The height of the residual barium column was not determined, as the ingestion of the same volume of contrast to a specific dilution was not predetermined in all the patients.
HREM
HREM was performed by using the following protocol: a 36-channel, solid-state catheter system with high-fidelity circumferential sensors at 1-cm intervals was advanced through the nose (Given Scientific Instruments, Los Angeles, CA, United States). The pressure data of ten, 5 mL swallows of water were recorded and analyzed using Mano View software (Given Scientific Instruments, Los Angeles, CA, United States). All relevant parameters were analyzed in accordance with the Chicago classification [19]. Basal LES pressure was assessed before all wet swallows, using the LES markers. Impaired LES relaxation was determined using the 4-s integrated relaxation pressure (4-s IRP). LES parameters were determined as the mean pressures for 10 wet swallows of 5 mL each. Diagnostic criteria for achalasia were: incomplete relaxation of the LES (IRP > 15 mmHg, as for I type IRP > 10 mmHg) and absence of peristalsis of the esophageal body [20].
Achalasia was classified as Type I, II, or III. Type I was defined as 100% absence of peristalsis without esophageal pressurization. Type II was assigned for pan-esophageal pressurization >30 mmHg in ≥20% of swallows. Type III was designated for premature contractions in ≥20% of swallows [20].
PD
PD was performed under conscious sedation. A standard upper endoscopy was performed, and the esophagus was cleared of any residual food debris. A guidewire was placed into the antrum and, under fluoroscopic guidance, a Wilson-Cook achalasia balloon (COOK Medical, United States) was passed and positioned across the gastroesophageal junction and inflated for a few seconds until the “waist” was obliterated.
The Wilson-Cook achalasia balloon is available in 2 sizes; 3 and 3.5 cm according to the diameter of the dilators, with a length of 8 cm. For most Chinese patients, the 3.0-cm diameter dilator is the most appropriate. The balloon was then inflated to 3 atmospheres, until the obliteration of the waist was achieved and the pressure was maintained for 60 s.
Finally, the inspection was performed through the endoscope, and the bleeding from the mucosa of gastric cardia, if any was managed. Post-procedure, patients were observed for abdominal pain, shortness of breath, or other abnormal phenomena.
The patients were allowed a liquid diet at normal or low temperature, 2–3 h after the operation, and a semiliquid diet at 24 h. The patients were gradually returned to a normal diet over the next few days. Antacids were prescribed to the patients after the treatment. If symptoms were not relieved after the first PD, we performed a second treatment using a 3.5-cm balloon within 4 weeks of the first PD.
POEM
POEM was performed in a fashion similar to that described by Inoue and colleagues [6]. All POEM procedures were performed under general anesthesia in an endoscopy unit. To reduce the risk of air embolism, pneumothorax, and subcutaneous emphysema, carbon dioxide insufflation was used. First, a submucosal injection with normal saline and indigo carmine was made, 10 cm above the esophagogastric junction and then a 2-cm longitudinal incision. The initial mucosal incision was done in the 5–6 o’clock position on the posterior esophagus.
A submucosal tunnel was created, starting ~10 cm proximal to the LES and extending distally to ~2–4 cm into the stomach side. The myotomy was started 2 cm below the tunnel entrance and extended 2 cm into the proximal stomach. The circular muscle fibers were divided, and the longitudinal muscle fibers were preserved. The submucosal entry was closed by metal clips. After the procedure, a nasogastric tube was placed for gastric decompression.
Patients received intravenous antibiotics for 3 days, after which they began to take a liquid diet and were gradually switched to soft diet.
Patients’ follow-up
All the patients included in the study were monitored for at least 1 year to evaluate the effectiveness of treatment. At 3 months after treatment, all patients underwent HREM. Barium esophagogram was performed at 6 months after treatment. All patients were contacted via telephone every 3 months postoperatively to look for complications and to obtain the Eckardt score. An Eckardt score ≤3 was considered a therapeutic success. Symptomatic gastroesophageal reflux was assessed in patients every 3 months postoperatively using the GerdQ questionnaire. A score ≥7 (scale 0–18) was considered positive for gastroesophageal reflux.
Statistical analysis
Data regarding HREM, age, esophageal width, total Eckardt score, myotomy length, and follow-ups are described as mean ± standard deviation. Each symptom score, duration of symptoms, length of hospital stay, and procedure time are reported as the median value (interquartile range). Categorical variables were compared with the Chi-squared test or Fisher’s exact test. Means were analyzed by Student’s t test, and medians by the Wilcoxon rank sum test (Mann–Whitney U test). Paired variables in the same patient before and after treatment were compared using a paired t test or Wilcoxon signed-rank test. The cumulative symptom remission rate was estimated using the Kaplan–Meier method, and symptom remission rate distributions between the two groups were compared using the log-rank test. A two-tailed P value <0.05 was considered statistically significant. All the analyses were performed using SPSS version 20.0 software (IBM, Somers, NY, USA).
Results
Patient characteristics
From January 2012 to August 2015, 130 patients with achalasia received treatment in our hospital. Twenty-six patients received LHM and 104 patients received PD or POEM. Thirty-two patients who underwent PD or POEM were excluded from this analysis, because they had a history of prior treatment for achalasia. Seventy-two patients were enrolled in this study; that is, 32 patients who received POEM and 40 who underwent PD.
There was no significant difference between the 2 groups with regard to gender, age, body mass index, duration of symptoms, Eckardt score of symptoms, or achalasia subtypes (Table 1). On preoperative HREM, basal LES pressure and 4-s IRP were similar between the PD and POEM groups (Table 2), as was the width of the esophagus.
Short-term outcomes
After treatment, both basal LES pressure and 4-s IRP significantly improved in both groups (Table 2). At 3 months, the 4-s IRP decreased to <10 mmHg in 32/40 patients (80%) in the PD group and in 28/32 patients (87.5%) in the POEM group. The esophageal width also was reduced at 6 months after treatment. The improvement of Eckardt symptom scores was significantly higher in the POEM group (1.1 ± 1.0) than that in the PD group (1.7 ± 1.5; P = 0.042). However, the degree of improvement in the HREM and width of esophagus of the 2 groups were similar.
Subsequently, we compared the HREM parameters and esophageal widths of the PD and POEM groups according to the 3 manometric subtypes (Fig. 1). In type I, before treatment the basal LES pressure was higher in the PD group (28.45 ± 10.15 mmHg) than that in the POEM group (17.72 ± 2.67 mmHg; P = 0.007); the 4-s IRP and esophageal widths were similar (P = 0.188; P = 0.292, respectively). After treatment, the PD and POEM groups were similar in basal LES pressure (P = 0.592), 4-s IRP (P = 0.731), and esophageal widths (P = 0.613).
In patients with type II, the HREM parameters (basal LES pressure and 4-s IRP) and esophageal widths of the PD and POEM groups before treatment were similar to these parameters after treatment.
In type III patients, before treatment, the HREM parameters of the PD and POEM groups were similar (P = 0.388 for basal LES pressure, P = 0.233 for 4-s IRP), as were the esophageal widths (P = 0.613). After treatment, the basal LES pressure was higher in the PD group (20.13 ± 12.61 mmHg) than that in the POEM group (14.02 ± 7.19 mmHg) but the difference was not statistically significant (P = 0.439), and the 4-s IRP and esophageal widths were similar (P = 0.882; P = 0.70, respectively).
Intermediate-term outcomes
The mean follow-up period in the PD (30 ± 14 months) and POEM (25 ± 11 months) groups were comparable (P = 0.13). The Eckardt scores were available for all patients during the initial assessment and for all patients during the last assessment at the mean follow-up of 27 months. Overall, irrespective of manometric subtypes, the success rate as assessed by symptom remission was significantly higher in the POEM than that in the PD group (P = 0.013; Fig. 2). After the primary treatment, the success rates of PD at 3, 6, 12, 24, and 36 months were 95, 88, 75, 72, and 60%, respectively. However, after the primary treatment, the success rates of POEM at 3, 6, and 12 months were 96% at each time point and at 24 and 36 months were 93%.
Kaplan–Meier curves for success rate. Success rate is higher in POEM than in PD at mean follow-up of 27 months (P = 0.013). POEM has a higher success rate in type I, but the difference is not statistically significant (P = 0.09). Success rates are comparable in type II achalasia (P = 0.298). In type III patients, the difference is statistically significant (P = 0.038)
Subsequently, we compared the success rates of PD with that of POEM for each manometric subtype. There were 14 and 5 patients in the POEM and PD groups, respectively, with type I. At 1 year, for patients with type I the success rate in the POEM group was 100%, while that of the PD group was 63%, although the difference was not statistically significant (P = 0.09).
There were 18 and 22 patients in the POEM and PD groups, respectively, with type II. At 1 year, for patients with type II the success rate in the POEM group was 94% and that of the PD group was 82% (P = 0.298).
There were 9 and 4 patients in the POEM and PD groups, respectively, with type III. At 1 year, the success rates in the POEM and PD groups were 100 and 50%, respectively (P = 0.038).
In the PD group, 14 (35%) patients experienced recurrence at the mean follow-up of 30 months. Three of these received LHM, 4 received POEM, 5 patients received additional PD, and 2 did not receive further treatment since their symptoms were tolerable. In the POEM group, 2 (6%) patients were found to have recurrence at 6 and 15 months after the procedure. These patients were managed with repeat POEM and LHM, respectively.
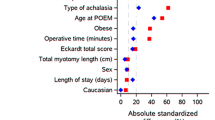
Procedural details and complications
The median operative time and length of stay of the PD group (20 [13–30] min and 3 [3–5] day, respectively) were significantly shorter than those of the POEM group (72.5 [40–180] min and 8 [6–10] day; P < 0.001 for both). In the POEM group, the median length of the myotomy was 8 (7–8) cm. No intraoperative mortality or major complication occurred in either of the 2 groups.
Four POEM patients developed subcutaneous emphysema, which recovered within 2–4 days and needed no further treatment (Table 3). Ten patients in the POEM group experienced chest pain which persisted for less than 2–3 days and did not require the use of narcotics.
In the follow-up period, 4/40 (10%) PD patients and 6/32 (18.8%) POEM patients had a GerdQ score ≥7, indicating symptomatic gastroesophageal reflux (P = 0.286). Their symptoms were relieved after oral proton pump inhibitor therapy.
Discussion
The present study showed that both PD and POEM were effective in improving the esophageal function evaluated at 3 months after treatment. This was suggested by the changes in LES pressures on HREM and symptom remission on short-term follow-up. However, POEM led to a better intermediate-term success rate compared with PD. The success rate for POEM was higher than that for PD in all 3 manometric subtypes, but statistically significant only in patients with type III achalasia.
To the best of our knowledge, this is the first study to compare PD with POEM for newly diagnosed achalasia with an intermediate-term follow-up. On short-term follow-up, both basal LES pressure and IRP were significantly reduced at 3 months, after either PD or POEM. Esophageal width also improved after either of the 2 treatments. However, after a high initial treatment success rate, the relapse rate of PD was higher than that of POEM. Our results are similar to that of previous studies, in which the short-term efficacy of PD was favorable (62–90%) [5, 21], but a third of patients were likely to relapse within 4–6 years, requiring repeat dilation [22]. In addition, repeated PD procedures increase the risk of perforation [23] and can lead to development of scar tissue at the gastroesophageal junction [24]. This makes future myotomy much more difficult and may decrease the clinical effect.
In the present study, PD was performed in only one series within 4 weeks, and re-dilation after the first series was considered a PD failure. The initial remission rate of PD was good, but after the first PD treatment the recurrence rate was 35% within 3 years, and further treatments were required. This is most likely because of incomplete disruption of the circular muscle fibers of the LES during PD, unlike POEM in which all the circular muscle fibers are divided under vision.
Several studies have shown that symptomatic outcomes in achalasia differ among the manometric subtypes [16, 19, 25] and may be useful in guiding the choice of treatment. In the present study, the success rates of PD and POEM were similar in patients with type II achalasia, on short- and medium-term follow-up. However, in types I and III, the success rates of POEM were higher than those of PD (although statistically significant only in type III). As shown by Pandolfino et al. [19], type III patients have a functional obstruction that encompasses not only the esophagogastric junction, but also the distal smooth muscle segment of the esophagus [16]. In the PD group, the dilator only disrupted the esophagogastric junction, whereas in the POEM group myotomy was extended 7–8 cm above the esophagogastric junction. The latter resulted in better relief of the esophageal outlet obstruction, and this may account for the higher success rates of POEM compared with PD.
Rohof et al. [15] reported that after treatment, type III patients treated by PD had significantly more esophageal stasis and a higher LES pressure compared with type III patients treated by LHM. This finding is consistent with our study. However, our small sample of type III patients may have prevented the demonstration of a statistical difference. Therefore, considering the large difference in success rates in our study, we suggest that patients with type III achalasia may be best treated with POEM.
The reported complication rate of POEM ranges from 3.3% [10, 26] to 16.7% [27]. In the present study, there was no major complication observed, as none of the patients had received prior endoscopic or surgical treatment and patients with sigmoid esophagus were excluded. The reported complications were inherent to POEM and were self-limiting and could be managed conservatively; no patient required conversion to another procedure. Of note, POEM is relatively complicated to perform, resulting in a longer procedure time and hospital stay compared with PD.
Both PD and POEM have their own advantages and disadvantages in the treatment of achalasia. Patient characteristics, patient’s attitude toward the procedure, desire to avoid subsequent interventions, and local expertise should be taken into consideration when selecting a procedure. In the present study, patients in both groups (PD or POEM) with type II achalasia responded well. Therefore, either procedure could be selected, depending on the patient’s attitude and the availability of local expertise to perform the procedures. Patients with type III achalasia may best be primarily treated by POEM, thus avoiding unsuccessful and repetitive dilation.
The present study is limited in that it is retrospective, and the number of patients involved was small. Although patients with types I or III achalasia treated by POEM had a better short- and intermediate-term effect compared with patients treated by PD, the number of type I and type III patients was rather small and larger studies are needed to confirm this finding. Another limitation is that pH measurement was not performed routinely after PD or POEM in these patients.
Conclusions
Both PD and POEM are effective and safe for the primary treatment for achalasia. The intermediate-term success rate of POEM seems to be higher than that of PD without increasing severe complications. Patients with types I and II achalasia could be treated by either PDs or POEM according to the experience of each individual center. Patients with type III achalasia are probably best treated by POEM. Future prospective multicenter large sample randomized trials with long-term follow-ups are required to validate the findings of this study.
References
Podas T, Eaden J, Mayberry M, Mayberry J (1998) Achalasia: a critical review of epidemiological studies. Am J Gastroenterol 93:2345–2347
Ben-Meir A, Urbach DR, Khajanchee YS, Hansen PD, Swanstrom LL (2001) Quality of life before and after laparoscopic Heller myotomy for achalasia. Am J Surg 181:471–474
Zarate N, Mearin F, Baldovino F, Armengol JR, Malagelada JR (2002) Achalasia treatment in the elderly: Is botulinum toxin injection the best option? Eur J Gastroenterol Hepatol 14:285–290
Richter JE, Boeckxstaens GE (2011) Management of achalasia: surgery or pneumatic dilation. Gut 60:869–876
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, Swanstrom LL, Vassiliou MC (2014) Per-oral endoscopic myotomy white paper summary. Surg Endosc 28:2005–2019
Bechara R, Ikeda H, Inoue H (2015) Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol 12:410–426
Teitelbaum EN, Soper NJ, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Hirano I, Hungness ES (2014) Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc 28:3359–3365
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264
Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rosch T, Fockens P (2013) Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 78:39–44
Chan SM, Wu JC, Teoh AY, Yip HC, Ng EK, Lau JY, Chiu PW (2016) Comparison of early outcomes and quality of life after laparoscopic Heller’s cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig Endosc 28:27–32
Marano L, Pallabazzer G, Solito B, Santi S, Pigazzi A, De Luca R, Biondo FG, Spaziani A, Longaroni M, Di Martino N, Boccardi V, Patriti A (2016) Surgery or peroral esophageal myotomy for achalasia: A systematic review and meta-analysis. Medicine (Baltimore) 95:e3001
Schneider AM, Louie BE, Warren HF, Farivar AS, Schembre DB, Aye RW (2016) A matched comparison of per oral endoscopic myotomy to laparoscopic heller myotomy in the treatment of achalasia. J Gastrointest Surg 20:1789–1796
Rohof WO, Salvador R, Annese V, des Varannes SB, Chaussade S, Costantini M, Elizalde JI, Gaudric M, Smout AJ, Tack J, Busch OR, Zaninotto G, Boeckxstaens GE (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144:718–725 (quiz e13–e14)
Salvador R, Costantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta L, Ceolin M, Finotti E, Nicoletti L, Da Dalt G, Cavallin F, Ancona E (2010) The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointest Surg 14:1635–1645
Zerbib F, Roman S (2015) Current therapeutic options for esophageal motor disorders as defined by the Chicago Classification. J Clin Gastroenterol 49:451–460
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ (2008) Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526–1533
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39:713–720
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313:1841–1852
Katzka DA, Castell DO (2011) Review article: an analysis of the efficacy, perforation rates and methods used in pneumatic dilation for achalasia. Aliment Pharmacol Ther 34:832–839
Smith CD, Stival A, Howell DL, Swafford V (2006) Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than heller myotomy alone. Ann Surg 243:579–584 (discussion 584–576)
Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, Banerjee R, Lakhtakia S, Gupta R, Tandan M, Rao GV, Reddy DN (2011) Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil 17:48–53
Zhang XC, Li QL, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ, Hu JW, Cai MY, Yao LQ, Zhou PH (2016) Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy 48:967–978
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256:659–667
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Fandong Meng, Peng Li, Yongjun Wang, Ming Ji, Yongdong Wu, Li Yu, Yinglin Niu, Fujing Lv, Wei Li, Wenyan Li, Huihong Zhai, Shanshan Wu, and Shutian Zhang have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Meng, F., Li, P., Wang, Y. et al. Peroral endoscopic myotomy compared with pneumatic dilation for newly diagnosed achalasia. Surg Endosc 31, 4665–4672 (2017). https://doi.org/10.1007/s00464-017-5530-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5530-0