Abstract
Background
Incisional hernia repair is one of the most common general surgery operations being performed today. With the advancement of laparoscopy since the 1990s, we have seen vast improvements in faster return to normal activity, shorter hospital stays and less post-operative narcotic use, to name a few.
Objective
The key aims of this review were to measure the impact of minimally invasive surgery versus open surgery on health care utilization, cost, and work place absenteeism in the patients undergoing inpatient incisional/ventral hernia (IVH) repair.
Methods
We analyzed data from the Truven Health Analytics MarketScan® Commercial Claims and Encounters Database. Total of 2557 patients were included in the analysis.
Results
Of the patient that underwent IVH surgery, 24.5% (n = 626) were done utilizing minimally invasive surgical (MIS) techniques and 75.5% (n = 1931) were done open. Ninety-day post-surgery outcomes were significantly lower in the MIS group compared to the open group for total payment ($19,288.97 vs. $21,708.12), inpatient length of stay (3.12 vs. 4.24 days), number of outpatient visit (5.48 vs. 7.35), and estimated days off (11.3 vs. 14.64), respectively. At 365 days post-surgery, the total payment ($27,497.96 vs. $30,157.29), inpatient length of stay (3.70 vs. 5.04 days), outpatient visits (19.75 vs. 23.42), and estimated days off (35.71 vs. 41.58) were significantly lower for MIS group versus the open group, respectively.
Conclusion
When surgical repair of IVH is performed, there is a clear advantage in the MIS approach versus the open approach in regard to cost, length of stay, number of outpatient visits, and estimated days off.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Approximately, 2 million laparotomies are done each year in the US [1]. Even with meticulous closure techniques, the rate of incisional hernia at 3 years has been reported to be as high as 22% [2]. In the US, we spend more than three billion dollars annually on inpatient and outpatient incisional/ventral hernia (IVH) repairs [3]. In the early 1990s, IVH were repaired mainly in an open fashion. With the advancement of minimally invasive surgery (MIS) techniques during that time period, we began to see the advantages in the field of IVH repair. One of the first described MIS techniques and studies was done by LeBlanc in 1993, which has paved the way for further studies on the benefits of MIS for IVH repairs [4].
Over the past decade, many studies have compared laparoscopic ventral hernia repair to open repair. Most studies have shown a consistent advantage of laparoscopic approaches versus open to have shorter lengths of stay, lower complication rates, decreased costs, comparable operating times, and lower hernia recurrence rates [3, 5–9]. Still, the rate of adoption of laparoscopic IVH repair in the US remains low [10].
The key aims of this study were to measure the impact of inpatient MIS versus open IVH repair on health care utilization, cost, and work place absenteeism.
Methods
Data source
Data for this study were obtained from the Truven Health Analytics MarketScan® Commercial Claims and Encounters Database. This commercial database contains the enrollment and health care (medical and drug) claims of multi-million employees and their dependents that are covered annually under a variety of health plans offered by medium-sized or large firms. Specifically, this commercial database includes inpatient, outpatient, emergency room, and outpatient prescription drug claims, linked by a unique patient identifier. The three years (2009–2011) of the commercial database contains de-identified claims data for approximately 70 million enrollees from more the 300 self-insured employers, 25 health plans, and 350 unique carriers in the United States. The data conformed to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) confidentiality requirements, so neither informed consent nor Institutional Review Board (IRB) approval were required for this study. The HPM Database is linkable via a unique enrollee identifier to the medical and pharmacy experience of a subset of employees in the Commercial database whose employers contribute their short-term disability claims experience.
Sample selection
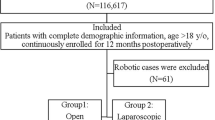
Step-wise sample selection is presented in Fig. 1. All adults between the ages of 18 and 64, admitted as inpatients, with ICD-9-CM primary diagnosis code for IVH (ICD-9-CM diagnosis code: 551.20, 551.21, 552.20, 552.21, 553.20, 553.21; code descriptions provided in Fig. 2) in calendar year (CY) 2010 were selected. These patients were investigated for any incidence hernia repair post-diagnosis in the same calendar year. ICD-9-CM procedure codes and/or CPT codes used to define surgical treatment are provided in Fig. 3. For the surgical patients the date of surgery was defined as the index date. To keep the follow-up time consistent for all patients, only patients with continuous enrollment of 12-month pre- and post-index date were retained in the final sample. A surgery was considered as a recurrent surgery if the patients had any incidence of IVH repair surgery within past 12 months to the index date. Only patients with complete demographic information were included in the final analysis. To control for outlier costs and utilization, only patients with total one-year cost between 5th and 95th percentile were included in the final analysis. The codes to identify MIS and open groups are provided in Appendix 2.
Outcome measures and statistical analysis
We compared the outcomes between MIS and Open surgical patients.
-
1.
Patient characteristics:
Patient characteristics as of index date were compared between the two groups using t test for continuous variables (age and Charlson Comorbidity Index (CCI)) and Chi-square test for the categorical variables (gender, region).
-
2.
Pre- and post-index date cost and utilization:
The 1-year pre-index date costs and utilization were compared between the two groups. The reimbursements are being considered as costs for this study. If patients did not have utilization or costs over long-term follow-up then those parameters were coded as zero to ensure complete view of long-term utilization and costs. Mean total cost and mean inpatient length of stay (LOS) were compared between the two groups. We also compared the mean number of hospital outpatient, physician office, and emergency room (ER) visits, respectively. The pre-index cost and utilization data were compared using the t test method.
The cost and utilization outcome measures were compared for 90-days as well as 365-days post-index date. The post-index period included the index procedure data. Regression model adjusting for age, gender, CCI score (pre-index period) and region was used to compare utilization and cost between two groups.
-
3.
Pre- and post-index estimated days off from work
In the absence of sufficient sample size from the linked HPM database, we defined a proxy estimate for number of days off from work based on utilization data. For an office visit, an ER visit, or an Ambulatory surgery center (ASC) visit claim, we estimated half a day of utilization. If a patient had a claim for an outpatient visit, we estimated as full-day utilization. For inpatient service claim, the length of stay was converted directly to days of utilization. T test was used to compare mean number of days off between the two groups. For 90-day post-index as well as 365-day post-index analysis regression models adjusting for age, gender, CCI score (pre-index period), and region were used to compare estimated days off from work between two groups.
The MIS versus open comparison samples were very similar in the pre-index data for the inpatient population; thus to assess the outcomes post-surgery, we also performed a difference-in-difference approach. This analysis was adjusted for patient’s prior health care utilization. Outcomes were modeled using generalized linear model. Within individuals, correlation was adjusted using generalized estimating equation (GEE). Office and hospital outpatient utilization and estimated days off from work were modeled using negative binominal distribution. Costs were estimated using gamma distribution. ER and inpatient services were modeled only for the post-period with logit link and binomial distribution. Independent variables in the regression model included age, region, procedure type, CCI (pre and post), index hospital cost, and index hospital LOS. For difference-in-difference analysis, the index procedure data were excluded from this analysis. Cross-sectional comparison of index procedure cost and utilization data for the index procedure was performed separately using regression model adjusting for age, gender, CCI score (pre-index period), and region.
All the analysis was performed using SAS 9.2 software. The differences between the groups were considered significant at p < 0.05.
Results
A total of 3012 patients were included in the final analysis. The sample attrition is presented in Fig. 1. Approximately, 85% of the patients with a primary diagnosis code of IVH underwent surgery. Of these surgery patients, MIS and open surgery was performed in 24.5 and 75.5% patients, respectively.
MIS versus open
Demographic characteristics (Table 1): The open patients were slightly older than the MIS patients (51.3 vs. 50.3 years, p value = 0.0084). All the other index date demographic characteristics were similar between the two groups.
365-day Pre-index cost, utilization, estimated days off (Table 2): The MIS and open groups were similar for 365-day pre-index cost, utilization, and estimated days off (all p < 0.05).
90-day Post -index cost, utilization, estimated days off (Table 3): Total 90-day post-index date cost for MIS surgical patients was $2419.15 less compared to open surgical patients ($19,288.97 vs. $21,708.12, p < 0.0001). Compared to open patients, MIS patients also had a lower mean inpatient LOS (3.12 vs. 4.24, p < 0.0001), lower mean number of hospital outpatient visits (5.48 vs. 7.35, p < 0.0001), and lower number of ER visits (0.37 vs. 0.46, p = 0.0472). The estimated days off was 3.3 days less as compared to open group (p < 0.0001).
365-day Post-index cost, utilization, estimated days off (Table 4): Total 365-day post-index date cost for MIS patients was $2659.33 less compared to open patients ($27,497.96 vs. 30,157.29, p = 0.0012). The post-index date cost was inclusive of index surgery data. Compared to open patients, MIS patients also had a lower mean inpatient LOS (3.7 vs. 5.04, p < 0.0001), lower mean number of hospital outpatient visits (19.75 vs. 23.42, p = 0.0018), and lower number of ER visits (1.39 vs. 1.74, p = 0.0161). The estimated days off remained significant even at 365-day post-index date; MIS patients had approximately 6 days less days off work due to healthcare utilization compared to open patients (p = 0.0001).
MIS versus open index surgery costs (Table 5): Adjusted mean total cost for index procedure for MIS group was $1834 (p < 0.0001). Patients undergoing MIS procedure on average stayed one day less in the hospital as compared to open patients (p < 0.0001).
MIS versus open 90-day and 365-day cost, utilization, estimated days off using difference-in-difference method (excluding index procedure data) (Table 6): Table 6 compares 90-day and 365-day pre- and post-healthcare utilization. Open patients were significantly associated with 137% (95% CI 112–167%) increase in number of days off compared to MIS patients. In addition, the open patient group also showed significantly higher drug expenditure than MIS in the post-surgery period. The results were not significant for 365-day comparison. For the 90- and 365-day adjusted comparisons that are provided in Table 6, MIS group was used as a reference category.
Discussion
Incisional hernia repair is one of the most common operations a general surgeon will perform today. Quality of life measurements have also been shown to improve after ventral hernia repair which is an important factor to consider [11]. When comparing our MIS versus open hernia repair group, we found significant advantages at the 90- and 365-day time points in the MIS group regarding length of stay, fewer outpatient visits and emergency room visits and fewer days off work. This phenomenon is seen in many open versus laparoscopic comparisons [12–14]. Total payment at the 90- and 365-day time points is significantly greater in the open group which most likely represents an increase in payment secondary to the longer length of stay and increase in office and emergency room visits. Drug expenditure was higher for the open group at 90 days which is probably related an increase in pain medication use seen in other open versus laparoscopic studies [15, 16].
The power of using such a large data base is clearly evident with the Truven Health Analytics MarketScan® Commercial Claims and Encounters Database. When comparing the over 2500 cases of Open versus MIS patients, there was a 3:1 ratio of patient having open surgery. This trend was also observed in a previous study by Funk et al. looking at national practice patterns for inpatient management of ventral abdominal wall hernias in the United States [17]. In Funk’s study, which analyzed 112,000 ventral hernia repairs, only 26% of the cases were being performed laparoscopically. With the advent of more laparoscopic fellowships and the increasing exposure of trainees to minimally invasive surgery, the numbers of minimally invasive hernia repairs should rise.
When looking at the adjusted mean total cost for index procedure for MIS group as compared to the open group, the MIS procedure was $1,834 less expensive. Patients undergoing MIS procedure on average stayed one day less in the hospital as compared to open patients and the inpatient cost was $1748.23 less. Unfortunately, reimbursements to physicians performing MIS hernia procedures were on average, $565.66 less.
Ninety-day pre- and post-healthcare utilization demonstrated that open patients were significantly associated with 137% increase in number of days off and 125% higher drug expenditures as compared to MIS patients. These two variables are most likely related to the higher pain issues associated open hernia surgery and the prolonged use of narcotics after surgery.
Conclusion
There is a clear advantage with the MIS versus open surgical repair of incisional/ventral hernias in regard to cost, length of stay, number of outpatient and emergency room visits, and days off work. The main conclusion of this study is that minimally invasive techniques in hernia repair can offer advantages over an open approach, but a case by case analysis should be done on each patient to determine the best clinical outcome for the patient.
References
Wechter ME, Pearlman MD, Hartmann KE (2005) Reclosure of the disrupted laparotomy wound: a systematic review. Obstet Gynecol 106(2):376–383
Fink C, Baumann P, Wente MN, Knebel P, Bruckner T, Ulrich A, Werner J, Buchler MW, Diener MK (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101(2):51–54
Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, Beck W, Holzman MD (2012) Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 16:179–183
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Holman MD, Purut CM, Reintgen S, Eubanks S, Pappas TN (1997) Laparoscopic ventral and incisional hernioplasty. Surg Endosc 11:32–35
Kaoutzanis C, Leichtle SW, Mouawad NJ, Welch KB, Lampman RM, Cleary RK (2013) Postoperative surgical site infections after ventral/incisional hernia repair: a comparison of open and laparoscopic outcomes. Surg Endosc. doi:10.1007/s00464-012-2743-0
Goodney PP, Birkmeyer CM, Birkmeyer JD (2002) Short-term outcomes of laparoscopic and open ventral hernia repair. Arch Surg 137:1161–1165
Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK (2009) Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg 197:64–72
Mason RJ, Moazzez A, Sohn HJ, Berne TV, Katkhouda N (2011) Laparoscopic versus open anterior abdominal wall hernia repair: 30-day morbidity and mortality using the ACS-NSQIP database. Ann Surg 254:641–652
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. doi:10.1002/14651858.CD007781.pub2
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642
Kouhia ST, Heiskanen JT, Huttunen R, Ahtola HI, Kiviniemi VV, Hakala T (2010) Long-term follow-up of a randomized clinical trial of open versus laparoscopic appendectomy. Br J Surg 97(9):1395–1400
Nguyen NT, Ho HS, Palmer LS et al (2000) A comparison study of laparoscopic versus open gastric bypass for morbid obesity. J Am Coll Surg 191:149–155
Qiu S, Doyon LM, Divino CM (2014) The safety of laparoscopic versus open ventral hernia repair in 23,327 morbidly obese patients. J Surg Res 186(2):538–538
Holzer A, Jirecek ST, Illievich UM, Huber J, Wenzl RJ (2006) Laparoscopic versus open myomectomy: a double-blind study to evaluate postoperative pain. Anesth Analg 102(5):1480–1484
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827
Funk LM, Perry KA, Narula VK, Mikami DJ, Melvin WS (2013) Current national practice patterns for inpatient management of ventral abdominal wall hernia in the United States. Surg Endosc 27(11):4112
Author information
Authors and Affiliations
Ethics declarations
Disclosures
Dean Mikami is a consultant for Medtronic, W.L. Gore and BD. W. Scott Melvin is a consultant for Stryker. Kenric Murayama and Michael Murayama have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mikami, D.J., Melvin, W.S., Murayama, M.J. et al. Impact of minimally invasive surgery on healthcare utilization, cost, and workplace absenteeism in patients with Incisional/Ventral Hernia (IVH). Surg Endosc 31, 4412–4418 (2017). https://doi.org/10.1007/s00464-017-5488-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5488-y