Abstract
Background
Endoscopic placement of fully covered self-expanding metal stents (FCSEMS) to treat malignant dysphagia in patients with esophageal cancer significantly improves dysphagia; however, these stents have a high migration rate.
Aim
To determine whether FCSEMS fixation using an endoscopic suturing device treated malignant dysphagia and prevented stent migration in patients with locally advanced esophageal cancer receiving neoadjuvant therapy when compared to patients with FCSEMS placement alone.
Method
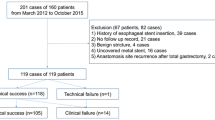
A review of patients with locally advanced esophageal cancer who underwent FCSEMS placement at 3 centers was performed. Patients were divided into two groups: Group A (n = 26) was composed of patients who underwent FCSEMS placement with suture placement, and Group B (n = 67) was composed of patients with FCSEMS placement alone.
Results
There were no significant differences between Groups A and B in demographics, and tumor characteristics. The technical success rate for stent placement was 100 %. There was no difference between Groups A and B in the median stent diameter and stent lengths. Mean dysphagia score obtained at 1 week after stent placement had improved significantly from baseline (2.4 and 1, respectively, p < 0.001). Patients had a median follow-up of 4 months. Immediate adverse events were mild chest discomfort in 4 patients in Group A and 2 patients in Group B (p = 0.05), and significant acid reflux in 3 patient in Group A compared to 2 patients in Group B (p = 0.1). The stent migration rate was significantly lower in Group A compared to compared to Group B (7.7 vs 26.9 %, respectively, p = 0.004). There was a delayed perforation in 1 patient and 1 death due to aspiration pneumonia in Group B.
Conclusion
Fixation of esophageal FCSEMSs by using an endoscopic suturing device in patients receiving neoadjuvant therapy was shown to be feasible, safe, and relatively effective at preventing stent migration compared to those who had stent placed alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Patients with locally advanced esophageal malignancy are frequently diagnosed at advance stages with symptoms of dysphagia that leads to poor quality of life, prevents adequate oral intake, and renders surgical resection and/or chemo-radiation therapy challenging [1–3]. Endoscopic stent placement using uncovered, partially covered, and fully covered stents offers immediate resolution of the dysphagia symptoms; however, these stents have its own set of challenges.
In general, uncovered and partially covered stents have lower migration rates compared to fully covered stents but are very challenging to remove. On the other hand, covered stents have higher migration rates but are easier to remove [4, 5].
In patients with locally advanced esophageal cancer, the current standard of care is to offer neoadjuvant therapy prior to undergoing definitive surgical resection of the cancer [6, 7]. However, this often leads to acute inflammation and edema in the oropharyngeal and esophageal mucosa, thereby often initially increasing swallowing difficulties. Siddiqui et al. [1] have demonstrated that placement of fully covered esophageal SEMS (FCSEMS) in patients with locally advanced esophageal cancer during neoadjuvant therapy significantly improves dysphagia and allows for oral nutrition during neoadjuvant therapy. The distinct advantage of using FCSEMS is that they can be easily removed before surgery. One major disadvantage of these FCSEMS is that they are associated with high migration rate (26–60 %), therefore requiring repeat endoscopic interventions and possible stenting [8]. Through-the-scope clips have proven to be ineffective in anchoring esophageal stents in place and preventing migration. While over-the-scope clips (OTSC) are proven to be efficacious for anchoring the esophageal stent in these situations, they are very difficult to remove when needed [9].
It seems intuitive to use a direct endoscopic suturing technique, with its potential for accuracy and simplicity of function for anchorage of a FCSEMS esophageal stent in patients with locally advanced esophageal cancer during neoadjuvant therapy. This technique allows for direct endoscopic visualization in order to anchor the stent, decrease its migration rate, and also allows the ease of removal of FCSEMS prior to surgery.
The OverStitch Endoscopic Suturing System (Apollo Endosurgery Inc., Austin, TX) was approved by FDA in 2008 and was initially designed for closure of gastrointestinal wall during NOTES procedures [9]. Over the years, this technique has been applied in human mainly in isolated specific cases or small case series. In Sharaiha et al., endoscopic suturing proved to be safe and effective for the management of GI defects (fistulas, leaks, perforations) and stent anchorage in 26 patients with esophageal leaks and benign strictures [8, 10].
The aim of this multicenter retrospective study was to determine whether FCSEMS fixation using an endoscopic suturing device (Overstitch, Apollo Endosurgical) effectively treated malignant dysphagia and prevented stent migration in patients with locally advanced esophageal cancer receiving neoadjuvant therapy when compared to patients with FCSEMS placement alone.
Materials and methods
A retrospective review of patients with locally advanced esophageal cancer that underwent endoscopic FCSEMS placement across a malignant stricture prior to receiving neoadjuvant chemo-radiation at three tertiary referral centers between June 2011 and May 2015. Patients were identified using endoscopic database at each institution. All data were compiled into a central database. Inclusion criteria for our study are the following: (1) biopsy-proven esophageal cancer (squamous and adenocarcinoma); (2) locally advanced disease found on imaging (CT and/or EUS), and (3) symptoms of dysphagia. Dysphagia grading prior to the procedure as the follows: 0 = no dysphagia, 1 = dysphagia to normal solid foods, 2 = dysphagia to semisolid foods, 3 = dysphagia to liquids, and 4 = complete dysphagia. Metastatic diseases found on initial study were excluded.
The patients evaluated were divided into two groups: Group A (n = 26) composed of patients who underwent FCSEMS placement followed by suture placement using the OverStitch suturing device at the proximal portion of the stent, and Group B (n = 67) composed of patients with FCSEMS placement alone without sutures.
Endoscopic procedure, stent insertion, and suturing
The fully covered esophageal SEMS used in the present study included the EndoMAXX stent (Merit Medical, South Jordan UT), the WallFlex® stent (Boston Scientific Endoscopy, Natick, MA), the Bonastent™ (Endochoice, Atlanta, GA), or the Evolution® stent (Cook Endoscopy, Winston-Salem, NC). All of these metal stents have a silicone covering that extends their entire length and thus prevents tumor ingrowth. Stents were deployed in the standard manner over guidewires and with the aid of fluoroscopy. Stents were sized based on the location and size of the tumor, the length and severity of the stricture, and the diameter of the proximal and distal esophagus. Endoscopic and fluoroscopic confirmation of adequate stent position was obtained in all patients.
Stent suturing was performed using the OverStitch device that was inserted onto a double-channel endoscope. A suture anchor was inserted through the accessory channel and coupled to the suturing arm of the device. The handle portion of the device allowed the transfer of the needle and thus the suture through the stent. A cinch was then used to tighten and deploy the suture. Bites were sequentially taken through the stent and mucosa separately to ensure proper anchoring. One–three sutures were placed in separate locations at the endoscopist’s discretion to help anchor the proximal end of the stent to the esophageal wall.
Data acquisition included: patient demographics, stricture location, technical success (successful SEMS transverse the stricture), dysphagia scores, stent migration, stent-related adverse events (AEs), and follow-up duration. The study was approved by the institutional review board at each institution and patient consented to the use of related medical information.
Definitions
Technical success was defined as placement of a stent in the desired position as determined endoscopically and/or radiographically. In cases (Group A), this was also defined by successful placement of the suture. Early and late AEs were defined as complications that occurred <=24 and >24 h after stent placement, respectively. AEs were further categorized into mild, moderate, severe, and fatal, according to the current ASGE guidelines [11]. Migration was defined as displacement of the stent proximally or distally from the original location of deployment on follow-up endoscopy or imaging.
Statistical analysis
All quantitative data were summarized by mean and standard deviation (SD), “mean ± SD”, and count data were given their corresponding percentage “%”. The collected quantitative and count data were then subgrouped and analyzed using Student t test or Chi-square test (X 2). P value less than or equal to 0.05 was considered to be statistical significant. All statistical analyses were performed using Sigma Stat v3.5 software (Richmond, California, USA).
Results
Patient demographics and tumor characteristics
A total of 93 patients (mean age = 67.7 ± 11.2 years, male = 73 %) with malignant dysphagia due to locally advanced malignant esophageal lesions underwent endoscopic stent placement prior to neoadjuvant therapy at 3 tertiary US medical centers. Ninety patients had a diagnosis of adenocarcinoma (96.8 %), and 3 patients (3.2 %) had squamous cell cancer. The mean (SD) length of the malignant tumor was 5.3 ± 1.85 cm (range 4–10 cm). Tumors were located in the proximal esophagus (n = 3), middle esophagus (n = 16), and distal esophagus (n = 74). Seventy-eight patients had their disease staged as T3N0, 4 had their disease staged as T3N1, and 11 patients had their disease staged as T2N1. There were no significant differences between Groups A and B in demographics, length and location of tumor, and tumor stage.
Esophageal FCSEMS characteristics
The technical success rate for stent placement in patients both with and without suturing was 100 %. The Wallflex stent (n = 48) and Bonastent (n = 8), EndoMAXX (n = 31), and Evolution® stent (n = 6) with diameters of 18–25 mm and lengths of 60–150 mm were used. One–three sutures (mean = 2 sutures) were used consecutively in patients in Group A to fix the upper flared end of the stent with the esophageal wall. Seventy-four stents (79.6 %) crossed the gastroesophageal junction. One patient in Group A underwent dilation of the malignant stricture prior to stent placement compare to 4 patients in Group B (p = 1). There was no significant difference between Groups A and B in the median stent diameter (18 vs 18 mm, respectively, p = 1) and median stent lengths (100 vs 100 mm, p = 0.8). All patients underwent neoadjuvant therapy after esophageal stenting. Patient and stent characteristics are summarized in Table 1.
Dysphagia scores
Dysphagia scores were reported for the patient’s evaluated at the time of stent placement (baseline) and 1 week after stent placement. The mean dysphagia score (SD) at baseline was 2.4 ± 0.89 (range 0–4), and the mean dysphagia score at the 1 week follow-up was 1 ± 0.81(range 0–2). Compared to baseline, the dysphagia scores at week 1 after stent placement were significantly improved (p < 0.001).
Adverse events (Table 2)
Early mild adverse events included self-limiting chest discomfort in 4 patients in Group A compared to 2 patients in Group B (p = 0.05), and significant acid reflux in 3 patient in Group A compared to 2 patients in Group B (p = 0.1). No moderate or severe early AEs were noted. In Group A, late AEs occurred in 2 patients and included one case of food impaction in the stent and one case of bleeding from the tumor that was controlled using argon plasma coagulation (APC). In Group B, late AEs occurred in 4 patients: (a) One case of tumor ingrowth requiring removal of the old stent and placement of a new one; (b) one case of bleeding from the tumor that was controlled using argon plasma coagulation (APC); (c) a delayed perforation in 1 patient while receiving chemotherapy; and (d) 1 death due to aspiration pneumonia. The one patient with perforation of the esophagus had been undergoing neoadjuvant chemo-radiotherapy. This was a non-contained perforation, and the patient underwent operative repair with creation of a cervical esophagostomy. Patient was discharged from the hospital after surgery but was found to have evidence of metastatic disease on repeat imaging studies and treated with palliative care.
Stent migration
Stent migration was noted in a total of 20 of the 93 patients (21.5 %). The stent migration rate was lower in Group A compared to compared to Group B (7.7 vs 26.9 %). Using Kaplan–Meier analysis and log-rank analysis (Fig. 1), fixation of the stent with suturing significantly reduced the risk of migration (p = 0.004). There was no significant difference between crossing the gastroesophageal junction and rate of migration (p = 0.11) or diameter of stent used (p = 0.13). In subgroup analysis, there was no difference between the number of sutures used and stent migration (p = 0.7). There was also no difference between the types of stent used and migration (p = 0.58).
Follow-up evaluation
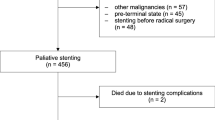
Patients had a median follow-up of 4 (range, 3–13) months. Due to disease progression or the discovery of metastasis after neoadjuvant therapy, only 18/26 patients in Group A and 22/67 patients in Group B underwent curative surgery. Patients that did not undergo curative surgical resection underwent palliative therapy. The esophageal stents were easily removed in those who proceeded to surgery at the time of the operation. During the follow-up, 7 patients in Group A and 4 patients in Group B died as a result of their esophageal cancer.
Discussion
The current standard of care is to offer neoadjuvant therapy to patients with locally advanced esophageal cancer. [7] [12] The majority of these patients will have dysphagia on presentation as a result of their tumor burden. While neoadjuvant therapy can improve symptoms of dysphagia by decreasing tumor size and increasing the esophageal luminal diameter, most patients will experience an initial worsening of their dysphagia as a result of mucositis. [13] Surgical placement of jejunostomy tubes has long been the mainstay for obtaining enteral access in patients undergoing neoadjuvant therapy and patients who are unable to consume an adequate caloric intake. Alternatively, Siddiqui et al. [1] have demonstrated that fully covered SEMS insertion can help to relieve dysphagia and maintain oral nutrition in patients with esophageal cancer who are receiving neoadjuvant therapy prior to a planned esophagectomy. However, stent migration occurred in up to one-third of their patients at some point. While placement of partially covered and uncovered stents may decrease the migration rate, subsequent removal prior to surgery can be challenging, costly and may require repeated endoscopic interventions leading to greater patient discomfort. Endoscopic suturing for mural anchoring of the FCSEMS in this scenario is an attractive option, and prior studies have shown promising outcome in fistulas, leaks, and perforations. Endoscopic suturing of self-expandable stents is also quick and technically easy with a learning curve of 10–15 cases.
In this study, we utilized a large number of patients in 3 tertiary centers to specifically evaluate the effect of endoscopic suturing in patient with malignant esophageal stricture undergoing neoadjuvant therapy. The stent migration rate was significantly lower in the sutured group as compared to the non-sutured group (7.7 vs 26.9 %, respectively, p = 0.004). This is significantly lower than the reported migration rate of 37–50 % in prior clinical studies [14–16]. Both groups showed identical percentages of cancers involving the distal esophagus (77 vs 81 %) which is a site where stent migration is higher. Additionally, stent length and diameter were similar in both groups, therefore making variation in stent measurements an unlikely culprit to account for the migration difference between the two groups. Potential reason to explain migration occurrence despite placement of suture included location of suture placement and suture depth as suture may be dislodged if placed too superficial. The rate of stent migration in patients with partially covered or uncovered SEMS is 0–10 % [5, 6, 12]. Our study demonstrates that endoscopic suturing of FCSEMS lowers the rates of stent migration so as to be comparable to uncovered and partially covered SEMS.
Immediately after stent placement, chest pain and reflux are frequent complaints. The chest pain may be explained by the radial force generated by the expansion of the stent. Smaller stent may decrease the incidence of chest pain, but this could potentially increase the rate of migration. In a study by Didden et al. [17], moderate to severe chest pain was reported in 60 % of patients after stent placement lasting around 10 days, but none of the patient required stent removal. In this study, there were reported immediate self-limiting chest pain and acid reflux in both groups without any difference. There was also one delayed perforation and 1 patient who died from complication of pneumonia in the non-sutured group (Group B).
The mean dysphagia score for patients in this study obtained at 1 week after stent placement showed statistically improvement from baseline of 2.4 to 1 (p < 0.001) with a mean follow-up of 4 months. While no formal assessment of quality of life (QOL) was made in the present trial, we believe that ability to swallow and take oral nutrition after stent placement may have resulted in an improved QOL.
Following stent placement, tissue over growth, food impaction, and stent migration are another most frequently encountered complications in patients with esophageal stents, and repeat endoscopic intervention is needed in 20–25 % of the patients [18]. Recurrent dysphagia after stent placement can occur in around one-third of the cases [19]. This said, esophageal SEMS continue to provide significant relief of dysphagia for both patients undergoing neoadjuvant therapy and palliative therapy. This is demonstrated by Conio et al. [20] who reported 100 % improvement in dysphagia score that lasted until death with mean survival of 4 months. This is comparable to our study. In addition, since a significant amount of our patients were deemed inoperable after receiving neoadjuvant therapy, FCSEMS provided a robust palliative relief of dysphagia. In patients who underwent surgical resection, the FCSEMS were easily removed endoscopically, including those that had been sutured.
In conclusion, endoscopic suturing anchoring of esophageal FCSEMS is shown to be feasible, effective, and safe at preventing stent migration in patients with malignant esophageal strictures receiving neoadjuvant therapy when compared to placement of stents alone. Most patients with locally advanced esophageal cancer will never proceed to curative resection. Patients who do not proceed to surgery can have their stent left in place as a palliative measure.
References
Siddiqui AA, Sarkar A, Beltz S, Lewis J, Loren D, Kowalski T et al (2012) Placement of fully covered self-expandable metal stents in patients with locally advanced esophageal cancer before neoadjuvant therapy. Gastrointest Endosc 76(1):44–51
Homs MY, Steyerberg EW, Eijkenboom WM, Tilanus HW, Stalpers LJ, Bartelsman JF et al (2004) Single-dose brachytherapy versus metal stent placement for the palliation of dysphagia from oesophageal cancer: multicentre randomised trial. Lancet 364(9444):1497–1504
Vlavianos P, Zabron A (2012) Clinical outcomes, quality of life, advantages and disadvantages of metal stent placement in the upper gastrointestinal tract. Curr Opin Support Palliat Care 6(1):27–32
Dua KS, Latif SU, Yang JF, Fang TC, Khan A, Oh Y (2014) Efficacy and safety of a new fully covered self-expandable non-foreshortening metal esophageal stent. Gastrointest Endosc 80(4):577–585
Song HY, Do YS, Han YM, Sung KB, Choi EK, Sohn KH et al (1994) Covered, expandable esophageal metallic stent tubes: experiences in 119 patients. Radiology 193(3):689–695
Siersema PD, van Hillegersberg R (2008) Treatment of locally advanced esophageal cancer with surgery and chemoradiation. Curr Opin Gastroenterol 24(4):535–540
Campbell NP, Villaflor VM (2010) Neoadjuvant treatment of esophageal cancer. World J Gastroenterol 16(30):3793–3803
Sharaiha RZ, Kumta NA, DeFilippis EM, Dimaio CJ, Gonzalez S, Gonda T, et al. (2016) A large multicenter experience with endoscopic suturing for Management of gastrointestinal defects and stent anchorage in 122 patients: a retrospective review. J Clin Gastroenterol 50(5):388–392
Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M et al (2014) International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc 80(4):610–622
Sharaiha RZ, Kim KJ, Singh VK, Lennon AM, Amateau SK, Shin EJ et al (2014) Endoscopic stenting for benign upper gastrointestinal strictures and leaks. Surg Endosc 28(1):178–184
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC et al (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Hyngstrom JR, Posner MC (2010) Neoadjuvant strategies for the treatment of locally advanced esophageal cancer. J Surg Oncol 101(4):299–304
Diaz R, Reynes G, Tormo A, de Juan M, Girones R, Segura A et al (2009) Long-term results of neoadjuvant chemotherapy and combined chemoradiotherapy before surgery in the management of locally advanced oesophageal cancer: a single-centre experience. Clin Transl Oncol 11(12):835–841
Bakken JC, Song LMWK, de Groen PC, Baron TH (2010) Use of a fully covered self-expandable metal stent for the treatment of benign esophageal diseases. Gastrointest Endosc 72(4):712–720
Senousy BE, Gupte AR, Draganov PV, Forsmark CE, Wagh MS (2010) Fully covered Alimaxx esophageal metal stents in the endoscopic treatment of benign esophageal diseases. Dig Dis Sci 55(12):3399–3403
Eloubeidi MA, Lopes TL (2009) Novel removable internally fully covered self-expanding metal esophageal stent: feasibility, technique of removal, and tissue response in humans. Am J Gastroenterol 104(6):1374–1381
Didden P, Spaander MC, Bruno MJ, Kuipers EJ (2013) Esophageal stents in malignant and benign disorders. Curr Gastroenterol Rep 15(4):319
Maetani I, Isayama H, Mizumoto Y (2007) Palliation in patients with malignant gastric outlet obstruction with a newly designed enteral stent: a multicenter study. Gastrointest Endosc 66(2):355–360
Homann N, Noftz MR, Klingenberg-Noftz RD, Ludwig D (2008) Delayed complications after placement of self-expanding stents in malignant esophageal obstruction: treatment strategies and survival rate. Dig Dis Sci 53(2):334–340
Conio M, Repici A, Battaglia G, De Pretis G, Ghezzo L, Bittinger M et al (2007) A randomized prospective comparison of self-expandable plastic stents and partially covered self-expandable metal stents in the palliation of malignant esophageal dysphagia. Am J Gastroenterol 102(12):2667–2677
Acknowledgments
This study was funded entirely through existing intramural funds and salary support. We would like to acknowledge Dr. Juliana Yang from the University of Texas Southwestern Medical Center for her work in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors attest that they have no commercial associations (e.g., equity ownership or interest, consultancy, patent and licensing agreement, or institutional and corporate associations) that might be a conflict of interest in relation to the submitted manuscript.
Additional information
Dr. Yang and Dr. Siddiqui are joint first authors on this manuscript.
The original version of this article was revised: Juliana Yang was misspelled as Julian Tang and should be listed as the first author.
An erratum to this article is available at http://dx.doi.org/10.1007/s00464-016-5259-1.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Placement of an esophageal FCSEMS followed by endoscopic suturing of the proximal end of the stent using the OverStitch device
Rights and permissions
About this article
Cite this article
Yang, J., Siddiqui, A.A., Kowalski, T.E. et al. Esophageal stent fixation with endoscopic suturing device improves clinical outcomes and reduces complications in patients with locally advanced esophageal cancer prior to neoadjuvant therapy: a large multicenter experience. Surg Endosc 31, 1414–1419 (2017). https://doi.org/10.1007/s00464-016-5131-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5131-3