Abstract
Background
Patients with Barrett’s esophagus (BE) and high-grade dysplasia (HGD) or intramucosal cancer (IMC) on endoscopic forceps biopsies are referred to endoscopic therapy even though forceps biopsies do not reflect the disease extent accurately. Endoscopic mucosal resection (EMR) and endoscopic ultrasound (EUS) are frequently used for staging prior to endoscopic therapy. Our aims were to evaluate: (1) if endoscopic forceps biopsies correlated with EMR histology in these patients; (2) the utility of EUS compared to EMR; and (3) if accuracy of EUS varied based on grade of differentiation of tumor.
Methods
This is a retrospective review of patients referred to endoscopic therapy of BE with HGD or early esophageal adenocarcinoma (EAC) who underwent EMR from 2006 to 2011. Age, race, sex, length of Barrett’s segment, hiatal hernia size, number of endoscopies and biopsy results and EUS findings were abstracted.
Results
A total of 151 patients underwent EMR. In 50 % (75/151) of patients, EMR histology was consistent with endoscopic forceps biopsy findings. EMR resulted in change in diagnosis with upstaging in 21 % (32/151) and downstaging in 29 % (44/151). In patients with HGD on EMR, EUS staging was T0 in 74.1 % (23/31) but upstaged in 25.8 % (8/31). In patients with IMC on EMR, EUS findings were T1a in 23.6 % (9/38), upstaged in 18.4 % (7/38) and downstaged in 57.8 % (22/38). EUS accurately identified EMR histology in all submucosal cancers. Grade of differentiation was reported in 24 cancers on EMR histology. There was no correlation between grade and EUS staging.
Conclusions
EUS is of limited utility in accurate staging of BE patients with HGD or early EAC. Endoscopic forceps biopsy correlated with EMR findings in only 50 % of patients. Irrespective of the endoscopic forceps biopsy results, all BE patients with visible lesions should be referred to EMR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As late as 2009, the standard of treatment for Barrett’s esophagus (BE) with high-grade dysplasia (HGD) or intramucosal cancer (IMC) was esophagectomy with lymph node dissection [1]. This approach was based on reports of occult cancer in 30–40 % of cases of HGD and concern for lymph node metastases in early esophageal adenocarcinoma (EAC). Esophagectomy is a life-changing surgery with morbidity of 55 %, lengthy hospital stay and mortality of 1–3 % even in the hands of skilled thoracic surgeons [2, 3]. The outpatient endoscopic treatments for BE and early EAC eradication have led to a drastic change in the management in the past decade [4–6]. In addition, a recent systematic review of 1874 patients who underwent esophagectomy for HGD or IMC found no lymph node involvement in all cases of HGD and only 1.9 % had positive lymph node involvement in IMC [7]. This led to the recommendation of endoscopic therapy in BE with HGD, IMC and selected cases with early submucosal cancers.
Prior to embarking on curative endoscopic therapy, careful patient selection by accurate staging is essential. Patients with HGD, IMC or superficial well-differentiated submucosal cancers without lymphovascular invasion are considered as suitable candidates for endoscopic therapy. Patients with more advanced disease have a higher risk of lymph node involvement and hence are best treated by esophagectomy. Patients are referred to endoscopic therapy based on endoscopic forceps biopsy findings in day-to-day practice. However, forceps biopsies do not accurately reflect the true lateral extent and depth of visible lesions within BE segment. Hence, endoscopic ultrasound (EUS) and endoscopic mucosal resection (EMR) are often incorporated for assessing the stage of the disease. EMR not only serves as a therapeutic modality but also provides tissue for histologic diagnosis in the management of dysplasia and early EAC. EMR will change the diagnosis in a significant proportion of patients when compared with endoscopic biopsies, given the larger tissue sample [8] and greater inter-observer agreement among pathologists [9].
In addition, EUS is routinely performed in academic institutions in patients referred to endoscopic therapy to rule out submucosal invasion or lymph node involvement. The utility of EUS in HGD and early EAC is uncertain. A recently published meta-analysis reported that EUS detected advanced disease in only a minority of patients with HGD or early EAC and therefore was considered of limited utility [10]. However, guidelines from surgical societies recommend EUS to improve the accuracy of clinical staging in the absence of metastatic disease, and to consider EMR as a diagnostic/staging tool for small, discrete nodules or areas of dysplasia when the disease appears limited to the mucosa or submucosa as assessed by EUS [11]. Given this controversy, the utility of EMR and EUS in patients with dysplastic BE and early EAC needs further clarification. Therefore, our aims were to assess:
-
1.
If there was any change in final diagnosis with EMR compared to pre-EMR endoscopic forceps biopsies in BE patients with dysplasia or early EAC.
-
2.
Whether EUS findings correlate with EMR in cases of HGD or cancer.
-
3.
The frequency of lymph node metastases detected with EUS in this group of patients.
-
4.
If accuracy of EUS varied based on grade of differentiation of early EAC.
Methods
Patient population
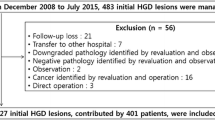
We performed a retrospective cohort analysis of BE patients with a diagnosis of HGD or early EAC referred to endoscopic therapy from January 1, 2006 to December 31, 2011 at our institution. Patients with visible lesions within BE segment who underwent EMR were included. Patients who underwent EUS more than 6 months prior to EMR and patients who received prior endoscopic therapy were excluded. Data were abstracted from the electronic medical records. Variables such as age, race, sex and body mass index (BMI) were analyzed. Endoscopic data such as the length of Barrett’s segment, hiatal hernia size, EUS and histologic findings were obtained. This study was approved by Cleveland Clinic Institutional Review Board.
Patient evaluation
Patients referred to endoscopic therapy had a repeat diagnostic esophagogastroduodenoscopy (EGD) performed and any subtle abnormalities were carefully noted. Patients underwent EUS and four quadrant biopsies every 1–2 cm in BE segment, depending on the endoscopists’ discretion. If the patients already had four quadrant biopsies done every 1–2 cm during the endoscopy which led to referral, then a repeat biopsy was typically not performed. All EUS procedures were performed by endosonographers who received additional year of training in advanced endoscopy procedures. EUS was performed with a radial echoendoscope, and fine-needle aspiration of any abnormal lymph nodes was performed with a curvilinear echoendoscope (Olympus America, Center Valley, PA). EUS classification of T was determined using either 10 mHz frequency on the radial echoendoscope and/or 20 mHz frequency via a through-the-scope EUS probe, based on the endosonographers’ preference. No visualization of tumor was staged as T0, T1a was tumor invasion limited to second layer (deep mucosa), T1b was tumor extension into third layer (submucosa), T2 was invasion to fourth ultrasound layer (muscularis propria), T3 was tumor invading into adventitia and T4 was tumor extension into surrounding structures. EUS classification of lymph node status was determined with 7.5 mHz frequency on the radial echoendoscope. Any lymph node width greater than 10 mm, round shape, echo-poor pattern or smooth lymph node border was considered suspicious for malignancy. FNA was performed if any peritumoral lymph node was visualized irrespective of the size.
EMR
Most EMRs were performed using multiband ligation technique as described elsewhere (Duette Multiband Mucosectomy Kit, Wilson–Cook, Winston–Salem, North Carolina) [12]. In a minority of cases, cap-assisted (Olympus America, PA) or free snare EMR technique was used. This consisted of lifting the target lesion with submucosal saline injection followed by snare cautery (Fig. 1).
Histologic confirmation
All external pathology specimens were reviewed by a gastrointestinal pathologist at the Cleveland Clinic, and the histologic diagnosis was confirmed. All EMR specimens and endoscopic forceps biopsies were evaluated by a gastrointestinal pathologist at our institution. In cases of dysplasia or cancer, they were confirmed by a second gastrointestinal pathologist or presented at consensus conference. Biopsies were graded as: no dysplasia, indefinite for dysplasia, low-grade dysplasia (LGD), HGD, IMC and submucosal cancer [13]. In cases of EMR specimens, depth of invasion, grade of differentiation, the presence or absence of tumor involved margins and lymphovascular invasion were routinely reported.
Subsequent management of patients included endoscopic therapy using radiofrequency ablation, cryotherapy or esophagectomy. In poor surgical candidates, brachytherapy was also utilized.
Statistical analysis
Data are presented as mean ± standard deviation, median (25th, 75th ‰) or N (%). Bowker’s test of symmetry was used to assess differences between endoscopic forceps biopsies and EMR histologic findings. EMR results were correlated with worst histologic grade on endoscopic forceps biopsy of visible lesions or biopsies from BE segment. In addition, Fisher’s exact test was used to compare EUS N stage and EUS T stage and EMR histology. A p < 0.05 was considered statistically significant. SAS version 9.2 (The SAS Institute, Cary, NC) and R version 3.0.1 (The R Foundation for Statistical Computing, Vienna, Austria) were used for all analyses.
Results
Patient characteristics
A total of 151 patients underwent EMR during the study period. Mean age was 67 ± 11 years, and 131 patients (87 %) were male. Racial distribution was: Caucasian 128, African-American 2, Hispanic 1 and unknown race 18. Mean BMI was 31 ± 6.6 kg/m2. Average BE segment length was 4 ± 3.2 cm, and hiatal hernia size was 2.8 ± 2 cm. Six patients had prior fundoplication. The mean time between endoscopic forceps biopsy and EMR is 2.1 ± 2.9 months. Seventy-six patients had one EMR session only during the course of endoscopic therapy. Seventy-five patients had additional EMR sessions––45 had 2 sessions, 20 had 3 sessions, 6 had 4 sessions and 4 had 5 sessions during the course of endoscopic therapy. Sixty-one (40.4 %) patients subsequently underwent RFA, and 43 (28.5 %) patients had cryotherapy. Three (2 %) patients went for brachytherapy, and 17 (11 %) patients had esophagectomy.
Endoscopic biopsy findings versus EMR findings
Among patients referred to endoscopic therapy, the endoscopic forceps biopsy results were LGD in 17 (11.3 %), HGD in 81(53.6 %), IMC in 47 (31.1 %) and invasive cancer in 5 (3.3 %) patients. One patient had BE with no dysplasia but was referred to endoscopic therapy in view of a polypoid lesion at the gastro esophageal junction. EMR histologic findings were normal mucosa in 6 patients (4 %), no dysplasia in 9 (6 %), LGD in 22 (14.6 %), HGD in 56(37.1 %), IMC in 50 (33.1 %) and submucosal cancer in 8 patients (5.3 %).
In 50 % (75/151) of patients, EMR histology was consistent with the endoscopic forceps biopsy findings. Overall, EMR histology and endoscopic forceps biopsy findings were discordant in 76 cases with upstaging in 21 % (32/151) and downstaging in 29 % (44/151). In patients with HGD on endoscopic forceps biopsy, diagnosis did not change in 50.6 % (41/81) and was upstaged in 25.9 % (21/81) and downstaged in 23.4 % (19/81). In patients with IMC who subsequently underwent EMR, the diagnosis did not change in 51 % (24/47), upstaged in 8.5 % (4/47) and downstaged in 40.4 % (19/47). In patients with invasive cancer on endoscopic forceps biopsies, diagnosis did not change in 20 % (1/5) and was downstaged in 80 % (4/5). These results are summarized in Table 1. Grade of differentiation was reported in 9 of the 52 cancers. Tumors were well to moderately differentiated in 8 cancers and poorly differentiated in one cancer. EMR histologic grade of differentiation was consistent in 5/9 cancers (well to moderately differentiated in 4/9, poorly differentiated in one and not graded in 4).
EMR histology versus EUS findings
Among the 114 patients with HGD, IMC or invasive carcinoma on EMR biopsies, 73 patients underwent EUS prior to EMR. In 31 patients with HGD on EMR, EUS tumor staging was T0 in 23 (74.2 %), T1a in 4(12.9 %), T1b in 3 (9.7 %) and T2 in one (3.2 %) patient. Abnormal lymph node was seen in one patient with HGD on EMR; FNA was not done in view of coagulopathy. He did not follow up and presented with invasive carcinoma 4 years after the EMR. Among patients with IMC on EMR (n = 50), 38 underwent EUS. EUS staging was T0 in 22, T1a in 9 and T1b in 7. There were 8 patients with submucosal cancer on EMR. Three patients did not have EUS: one patient was treated with brachytherapy, one did not follow up and died a year later and the third patient had metastatic renal cell carcinoma and was treated with definitive radiation therapy. One patient had EUS after EMR. T1sm was reported on EUS in all 4 patients with submucosal tumors on EMR who underwent prior EUS. In patients with HGD on EMR, no tumor was seen in 74.1 % (23/31) on EUS but upstaged in 25.8 % (8/31). For patients with IMC, EUS findings were consistent with the histologic diagnosis in 23.6 % (9/38), upstaged in 18.4 % (7/38) and downstaged 57.8 % (22/38). EUS accurately predicted EMR histology in all submucosal cancers. Overall EUS staging was inaccurate in 50 % of patients (37/73). Table 2 summarizes the EUS findings by EMR diagnosis. Grade of differentiation was reported in 24 cancers on EMR histology. Among well-differentiated cancers (n = 6), 5 had EUS and staging was T0 in 3, T1a in one and T1b in one. Among the moderately differentiated tumors (n = 17), 13 had EUS and staging was T0 in 6, T1a in 3 and T1 b in 4. One patient with poorly differentiated tumor on EMR histology had T1b disease on EUS.
Discussion
Endoscopic eradication therapy of BE achieves high success rates with very few complications [3]. The cornerstone of endoscopic management is the accurate staging of lesions and patient selection. EMR and EUS are widely used endoscopic diagnostic tools in the staging of patients with BE-related dysplasia or early EAC [6]. Our study demonstrated two important findings: EUS staging was inaccurate in a significant percentage of patients with HGD and early EAC, and endoscopic forceps biopsies of visible lesions differ from EMR findings in over half of patients. Therefore, all BE patients with visible lesions should be referred to EMR regardless of endoscopic forceps biopsy findings.
EMR provides an accurate histologic staging of BE-related lesions in addition to its potential curative role in IMC when the risk of lymph node metastasis or hematogenous dissemination is very low [14]. It is a safe and effective technique with low morbidity and mortality and low risk of recurrence [6, 15]. Even though endoscopic forceps biopsies provide useful information for diagnosing patients with BE, they do not always correlate with EMR findings. In 2008, Peters et al. [16] reported that EMR changed BE diagnosis in 49 % of the focal lesions and led to a change in the treatment in 30 %. This diagnostic superiority of EMR compared to endoscopic forceps biopsy is related to the larger tissue sample in EMR, and the ability to accurately determine the depth of invasion [17]. In BE patients diagnosed with HGD or IMC, other techniques used to stage include EUS and CT/PET scans. Studies showed superiority of EUS compared to CT scan and PET scan in T staging of EAC [18, 19]. However, the accuracy of EUS for early-stage cancer T1 and T2 is still unsatisfactory [20].
The results of this study are consistent with prior studies. In a study of 266 patients who underwent EUS and esophagectomy without preoperative chemoradiotherapy, EUS misclassified T stage in 119 patients (45 %) and erroneously predicted N classification in 67 patients (25 %). EUS classification was accurate only in T3 lesions (83 %) and it tended to overclassify T1 and T2 lesions [20]. When comparing EUS to EMR findings in our study, EUS underclassified IMC in majority of cases (57.8 %) and overclassified in 25.8 % of HGD patients. There are several possible explanations for EUS misclassification in BE-related dysplasia and EAC. One explanation is the inability to discriminate between microscopic tumor invasion and peritumoral inflammatory changes [21]. Many studies report alterations in morphologic factors in BE histology that might led to EUS misclassification including duplication of the muscularis mucosa and musculofibrous anomaly [22, 23]. Mandal et al. [22] reported that duplication of the muscularis mucosa resulted in overstaging as submucosal cancer by EUS. Another possible explanation for EUS misclassification is endoscopists’ experience. Catalano et al. compared intra- and inter-observer variation of EUS findings between experienced and inexperienced endosonographers [24]. Inexperienced endosonographer agreement was poor for all T stages but was good for lymph node metastasis. However, inter-observer agreement among experienced endosonographers was excellent for all T stages, except T2 (κ = .46). In a recently published meta-analysis, EUS resulted in a change in therapeutic approach in a minority of patients. In patients referred to endoscopic therapy, EUS identified advanced disease in 14 % (95 % CI 8–22 %; p < .001). In the absence of nodular disease, the proportion went down to 4 %. The pooled sensitivity for detecting ≥T1sm among BE patients with HGD or EAC was 56 % (95 % CI 47–65 %), and pooled specificity was 89 % (95 % CI 85–92 %) with positive predictive value of 63 % (95 % CI 53–72 %). The authors concluded that EUS tends to overstage patients with submucosal disease and EUS findings alone should not be considered in deciding final treatment plan [10].
The main strength of the study is that it is performed in a tertiary care center with specialized expertise in evaluation and treatment of BE-associated neoplasia. All pathology specimens were reviewed by experienced gastrointestinal pathologists at our institution. All endosonographers had an additional year of training in EUS and other advanced endoscopic procedures. There are also limitations to this study. It is a retrospective study and is carried out at a tertiary center which might have resulted in referral bias. Paris classification for the visible lesions is not consistently reported for all patients. An explanation for our study findings is the inter-observer variability in the endosonographers’ interpretation. EUS procedures were performed by 8 different endosonographers with varying levels of experience which may have had an impact on EUS findings. The grade of differentiation is not reported in all cancers in this series due to small tumor size on histology. Hence, our study is underpowered to assess whether accuracy of EUS varied by degree of differentiation of tumors.
In summary, there are diagnostic discrepancies when comparing endoscopic forceps biopsies to EMR specimens in patients with BE-related dysplasia or EAC. EUS staging was inaccurate in half of these patients. Therefore, we recommend the following: All BE patients with visible lesions should be referred to EMR irrespective of the endoscopic forceps biopsy results. In patients with BE with flat mucosa, four quadrant biopsies should be done every 2 cm or 1 cm in cases of known or suspected dysplasia. All biopsies and EMR specimens should be reviewed by a gastrointestinal pathologist and confirmed by a second pathologist. If HGD is found on EMR or endoscopic forceps biopsy of flat BE mucosa, EUS is not necessary. If IMC is found in a visible lesion and especially if poorly differentiated or has lymphovascular invasion, an EUS should be performed to look for lymph node involvement prior to proceeding with further endoscopic eradication therapy. These patients are best served by management in tertiary care centers with expertise in management of BE and EAC.
References
Fernando HC, Murthy SC, Hofstetter Shrager JB, Bridges C, Mitchell JD, Landreneau RJ, Clough ER, Watson TJ (2009) The society of thoracic surgeons practice guideline series: guidelines for the management of Barrett’s esophagus with high-grade dysplasia. Ann Thorac Surg 87:1993–2002
Swisher SG, DeFord L, Merriman KW, Walsh GL, Smythe R, Vaporicyan A, Ajani JA, Brown T, Komaki R, Roth JA, Putnam JB (2000) Effect of operative volume on morbidity, mortality, and hospital use after esophagectomy for cancer. J Thorac Cardiovasc Surg 119(6):1126–1134
Chang AC, Ji H, Birkmeyer NJ, Orringer MB, Birkmeyer JD (2008) Outcomes after transhiatal and transthoracic esophagectomy for cancer. Ann Thorac Surg 85(2):424–429
Guarner-Argente C, Buoncristiano T, Furth EE, Falk GW, Ginsberg GG (2013) Long-term outcomes of patients with Barrett’s esophagus and high-grade dysplasia or early cancer treated with endoluminal therapies with intention to complete eradication. Gastrointest Endosc 77(2):190–199
Orman ES, Li N, Shaheen NJ (2013) Efficacy and durability of radiofrequency ablation for Barrett’s esophagus: systematic review and meta-analysis. Clin Gastroenterol Hepatol 11(10):1245–1255
Ell C, May A, Gossner L, Pech O, Günter E, Mayer G, Henrich R, Vieth M, Müller H, Seitz G, Stolte M (2000) Endoscopic mucosal resection of early cancer and high-grade dysplasia in Barrett’s esophagus. Gastroenterology 118(4):670–677
Dunbar KB, Spechler SJ (2012) The risk of lymph-node metastases in patients with high-grade dysplasia or intramucosal carcinoma in Barrett’s esophagus: a systematic review. Am J Gastroenterol 107:850–862
Wani S, Abrams J, Edmundowicz SA, Gaddam S, Hovis CE, Green D, Gupta N, Higbee A, Bansal A, Rastogi A, Early D, Lightdale CJ, Sharma P (2013) Endoscopic mucosal resection results in change of histologic diagnosis in Barrett’s esophagus patients with visible and flat neoplasia: a multicenter cohort study. Dig Dis Sci 58(6):1703–1709
Wani S, Mathur SC, Curvers WL, Singh V, Alvarez Herrero L, Hall SB, Ulusarac O, Cherian R, McGregor DH, Bansal A, Rastogi A, Ahmed B, Singh M, Gaddam S, Ten Kate FJ, Bergman J, Sharma P (2010) Greater interobserver agreement by enodoscopic mucosal resection than biopsy samples in Barrett’s dysplasia. Clin Gastroenterol Hepatol 8:73–788
Qumseya BJ, Brown J, Abraham M, White D, Wolfsen H, Gupta N, Vennalaganti P, Sharma P, Wallace MB (2015) Diagnostic performance of EUS in predicting advanced cancer among patients with Barrett’s esophagus and high-grade dysplasia/early adenocarcinoma: systematic review and meta-analysis. Gastrointest Endosc 81(4):865–874
Varghese TK, Hofstetter WL, Rizk NP, Low DE, Darling GE, Watson TJ, Mitchell JD, Krasna MJ (2013) The society of thoracic surgeons guidelines on the diagnosis and staging of patients with esophageal cancer. Ann Thorac Surg 96:346–356
Soehendra N, Seewald S, Groth S, Omar S, Seitz U, Zhong Y, de Weerth A, Thonke F, Schroeder S (2006) Use of modified multiband ligator facilitates circumferential EMR in Barrett’s esophagus. Gastrointest Endosc 63(6):847–852
Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, Dixon MF, Fenoglio-Preiser CM, Fléjou JF, Geboes K, Hattori T, Hirota T, Itabashi M, Iwafuchi M, Iwashita A, Kim YI, Kirchner T, Klimpfinger M, Koike M, Lauwers GY, Lewin KJ, Oberhuber G, Offner F, Price AB, Rubio CA, Shimizu M, Shimoda T, Sipponen P, Solcia E, Stolte M, Watanabe H, Yamabe H (2000) The Vienna classification of gastrointestinal epithelial neoplasia. Gut 47:251–255
Soetikno RM, Gotoda T, Nakanishi Y, Soehendra N (2003) Endoscopic mucosal resection. Gastrointest Endosc 57(4):567–579
Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, Gossner L, Rabenstein T, Manner H, Guenter E, Huijsmans J, Vieth M, Stolte M, Ell C (2008) Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut 57(9):1200–1206
Peters FP, Brakenhoff KP, Curvers WL, Rosmolen WD, Fockens P, ten Kate FJ, Krishnadath KK, Bergman JJ (2008) Histologic evaluation of resection specimens obtained at 293 endoscopic resections in Barrett’s esophagus. Gastrointest Endosc 67(4):604–609
Mino-Kenudson M, Hull MJ, Brown I, Muzikansky A, Srivastava A, Glickman J (2007) EMR for Barrett’s esophagus—related superficial neoplasms offers better diagnostic reproducibility than mucosal biopsy. Gastrointest Endosc 66(4):660–666
Rice TW (2000) Clinical staging of esophageal carcinoma. CT, EUS, and PET. Chest Surg Clin N Am 10(3):471–485
Scotiniotis IA, Kochman ML, Lewis JD, Furth EE, Rosato EF, Ginsberg GG (2001) Accuracy of EUS in the evaluation of Barrett’s esophagus and high-grade dysplasia or intramucosal carcinoma. Gastrointest Endosc 54(6):689–696
Zuccaro G, Rice TW, Vargo JJ, Goldblum JR, Dumot JA, Adelstein DJ (2005) Endoscopic ultrasound errors in esophageal cancer. Am J Gastroenterol 100(3):601–606
Grimm H, Binmoeller K, Hamper K, Koch J, Henne-Bruns D, Soehendra N (1993) Endosonography for preoperative locoregional staging of esophageal and gastric cancer. Endoscopy 25(3):224–230
Mandal RV, Forcione DG, Brugge WR, Nishioka NS, Mino-Kenudson M, Lauwers GY (2009) Effect of tumor characteristics and duplication of the muscularis mucosae on the endoscopic staging of superficial Barrett esophagus-related neoplasia. Am J Surg Path 33(4):620–625
Pech O, Günter E, Dusemund F, Origer J, Lorenz D, Ell C (2010) Accuracy of endoscopic ultrasound in preoperative staging of esophageal cancer: results from a referral center for early esophageal cancer. Endoscopy 42(6):456–461
Catalano MF, Sivak MV, Bedford RA, Falk GW, van Stolk R, Presa F (1995) Observer variation and reproducibility of endoscopic ultrasonography. Gastrointest Endosc 41(2):115–120
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Prashanthi N. Thota, Alaa Saada, Madhusudhan R. Sanaka, Sunguk Jang, Rocio Lopez, John R. Goldblum, Xiuli Liu, John A. Dumot, John Vargo and Gregory Zuccarro have no conflict of interest.
Rights and permissions
About this article
Cite this article
Thota, P.N., Sada, A., Sanaka, M.R. et al. Correlation between endoscopic forceps biopsies and endoscopic mucosal resection with endoscopic ultrasound in patients with Barrett’s esophagus with high-grade dysplasia and early cancer. Surg Endosc 31, 1336–1341 (2017). https://doi.org/10.1007/s00464-016-5117-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5117-1