Abstract
Background
Repair of complex ventral hernia can be very challenging for surgeons. Closure of large defects can have serious pathophysiological consequences. Botulinum toxin A (BTA) has recently been described to provide flaccid paralysis to abdominal muscles prior to surgery, facilitating closure and repair.
Methods
This was a prospective observational study of 32 patients who underwent ultrasound-guided injections of BTA to the lateral abdominal wall muscles prior to elective repair of complex ventral hernia between January 2013 and December 2015. Serial non-contrast abdominal CT imaging was performed to measure changes in fascial defect size, abdominal wall muscle length and thickness. All hernias were repaired laparoscopically or laparoscopic-assisted with placement of intra-peritoneal mesh.
Results
Thirty-two patients received BTA injections which were well tolerated with no complications. A comparison of baseline (preBTA) CT imaging with postBTA imaging demonstrated an increase in mean baseline abdominal wall length from 16.4 to 20.4 cm per side (p < 0.0001), which translates to a gain in mean transverse length of the unstretched anterolateral abdominal wall muscles of 4.0 cm/side (range 0–11.7 cm/side). Fascial closure was achieved in all cases, with no instances of raised intra-abdominal pressures or its sequelae, and there have been no hernia recurrences to date.
Conclusions
Preoperative BTA injection to the muscles of the anterolateral abdominal wall is a safe and effective technique for the preoperative preparation of patients prior to laparoscopic mesh repair of complex ventral hernia. This technique elongates and thins the contracted and retracted musculature, enabling closure of large defects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Incisional hernia may occur in up to 20 % of midline abdominal incisions in low-risk patients, increasing up to 35 % in high-risk patients [1]. A subset of these hernias will develop into large and/or complex ventral hernia, which frequently results in impaired quality of life and repair of which is both technically challenging and time consuming [2]. The socioeconomic burden of disease associated with both the incidence and repair of incisional hernia is tremendous and can present some very unique challenges. Some patients will develop significant loss of domain, adding further difficulty to the repair. Muscle tension and chronic lateral muscle retraction reduce the volume of the peritoneal cavity over time and make fascial closure fraught with potential problems such as severe postoperative pain, wound dehiscence, abdominal hypertension, ventilatory compromise, and an elevated risk of hernia recurrence [1]. These patients will commonly have had multiple previous abdominal procedures and possibly multiple failed hernia repairs, rendering them at higher risk of recurrence with each additional repair [3]. In this population, adequate preparation prior to undergoing surgery is vital.
We present our experience with 32 patients using Botulinum toxin A (BTA) injections to the lateral abdominal oblique muscles in the preoperative preparation of patients prior to elective complex ventral hernia repair. BTA has been used successfully for delayed abdominal wall reconstruction after damage control laparotomy and open abdomen management, as well as the treatment of dystonias, spastic disorders and muscular pain syndromes, and for pain management after laparoscopic hernia repair [4–10]. Our protocol utilizes BTA’s resulting muscular (flaccid) paralysis to facilitate repair and closure of complex ventral hernia.
Methods
This is a single-center, prospective observational study of 32 patients who underwent preoperative BTA injections to the lateral abdominal wall muscles prior to elective complex ventral hernia repair between January 2013 and December 2015. All patients presented with complex ventral hernia, according to Slater et al’s [2] consensus paper on the definition of complex abdominal wall hernia.
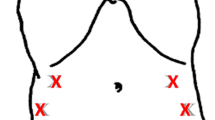
Our protocol for the preoperative preparation of patients using BTA has been previously published [11, 12]. Patients received BTA injections as an outpatient, 1–4 weeks prior to their planned operation. This time frame was chosen in order to allow the BTA to have attained full effect by the time of surgery. Most patients received a total dose of 300 units Botox® (Allergan, Australia) or equivalent dose of Dysport® (Ipsen Pharma, Australia), diluted to 2 U/ml with 0.9 % saline, and divided into six equal amounts. One patient with a laterally placed hernia received only unilateral injections, while all remaining patients received injections bilaterally. Using real-time ultrasound guidance, three sites were identified on each side of the abdomen, as identified by Smoot et al. [5] (Fig. 1), along the anterior axillary line equidistant between the costal margin at the level of the ninth rib and a point anterior to the anterior superior iliac spine (ASIS). To compensate for lateral retraction of abdominal wall muscles in patients with large fascial defects, some minor adjustments were made in the location of these injections. BTA was injected under direct (ultrasound) vision into each of the three muscle bellies of the lateral obliques (transversus abdominis, internal oblique, and external oblique). This process was repeated at each injection site.
Anatomic locations of the six injection sites for Botulinum toxin A, as determined by Smoot et al. [5]. Injection sites were subject to minor variation in patients with fascial defects causing significant lateral muscle retraction
Patients underwent either laparoscopic or laparoscopic-assisted mesh hernia repair. Routinely, an indwelling urinary catheter and nasogastric tube were inserted after induction of general anesthetic. Initial insufflation was undertaken using either Veress needle or Visiport entry. Multiple 5-, 12-, and 15-mm ports were inserted on both sides of the abdomen as required. In the total laparoscopic cases, fascial closure was obtained using transcutaneous non-absorbable sutures in a transverse shoelace pattern along the length of the defect. Intra-peritoneal onlay mesh (IPOM) repair was performed, with mesh secured both transfascially and using absorbable fixation tacks.
Laparoscopic-assisted cases were performed using laparoscopic-open-laparoscopic (LOL) techniques using 7-cm gel access ports, allowing repeated access to the abdominal cavity as required, for inspection of bowel, adhesiolysis, dissection of mesh off adherent bowel, and in some cases, assisting in closure of the fascial defect. LOL cases underwent a similar IPOM repair as the total laparoscopic cases. All surgeries were performed by the same surgeon (NI).
Postoperatively, patients were placed in an abdominal binder, in which they continued to wear for 3 months following repair. Selected patients were transferred to intensive care postoperatively, as dictated by comorbidities. Measurement of intra-abdominal pressures was not routinely undertaken. Intravenous antibiotics were continued for 72 h or longer if indicated. Patients were given an enoxaparin injection immediately postprocedure, and continued prophylactic injections while an inpatient. Patients wore calf compressors postoperatively, were given chest physiotherapy, and encouraged to mobilize.
Patients underwent non-contrast serial abdominal CT imaging at initial baseline assessment, postBTA injections (immediately preoperative), 4–8 weeks postoperative, and 6+ months postoperative. Additional scans were performed as clinically indicated. Measurements of lateral abdominal wall thickness and transverse abdominal wall length were performed using a single axial CT image at the same vertebral level on each occasion. Exact measurements of the hernia defect both before and after BTA were obtained in the same manner. Measurements were obtained in both resting and active crunching/ballooning maneuvers, with measurements taken along the deep surface of the abdominal wall muscle complex, from the lateral edge of quadratus lumborum to the medial edge of rectus abdominis on each side. Lateral abdominal wall muscle thickness measurements were measured from the deep surface of transversus abdominis to the superficial surface of external oblique at approximately the mid-axillary line. Both two dimensional images and volume rendered CT imaging were utilized in this process. Radiological assessments were all performed by the same radiologist (JR).
Statistical analysis was performed using Student’s t test and descriptive statistics using XLSTAT with significant values (p < 0.05).
Results
A total of 32 patients (15 females, 17 males) underwent preoperative abdominal wall BTA injections in preparation for repair of their complex ventral hernia. Mean age was 58 years (range 36–84), with a mean body mass index of 32.3 kg/m2 (range 22–54).
Thirty patients presented with ventral incisional hernias, with 23 midline defects and 7 lateral defects. The remaining two patients included in this study presented with laterally placed hernias of traumatic origin. Both arose from motor vehicle accidents and involved in one patient, a left lumbar hernia due to seat belt injury causing avulsion of the internal oblique and transversus abdominis from the left iliac crest, and in the other patient, a ‘thoracoabdominal wall rupture’ involving the lateral margin of left rectus sheath, disruption of left costal margin, and non-union of several fractured ribs, causing an intercostal and interparietal hernia.
Nine patients in the study were diabetic. Seven had significant cardiorespiratory comorbidities. Two patients had diagnosed Crohn’s disease, another had proven Ehlers–Danlos syndrome. One patient had undergone three previous abdominal wall resections for desmoid tumor with adjuvant radiotherapy. Three patients were current smokers or had ceased within the 6 weeks prior to surgery. The percentage of patients who were overweight or obese was 84 % (n = 27).
The smallest fascial defect was 5 cm × 9 cm, and the largest 24 cm × 27 cm (mean 12.3 cm). The smallest hernia within this cohort, at 5 × 9 cm, was a left flank and intercostal hernia with a floating 11th rib, resulting from an open partial nephrectomy performed a decade earlier. The hernia was associated with a large surrounding area of denervated muscle and eventration, with muscular atrophy through all three muscular layers of the lateral abdominal wall as well as left rectus abdominis. During repair, wiring of the left 10th and 11th ribs was required to restore anatomical continuity of bone and muscle/fascia.
Ten out of the 32 patients in our study had one previous failed repair; 15 patients had 2 or more failed repairs (one of these patients having undergone five previous failed repairs, another patient seven failed repairs).
There were no complications encountered from the administration of BTA into the lateral abdominal oblique muscles, and the injections were generally well tolerated. Most patients in our study noted a sense of bloating or distension 2–3 days after BTA injections. The relaxation of the abdominal wall musculature resulted in several patients complaining of a weak cough or sneeze. In cases where symptoms caused concern to patients, an abdominal binder was used with some benefit. These symptoms largely resolved after surgery, once the hernia defect had been closed and anatomical continuity was restored. All the patients regained normal function of their abdominal wall muscles as the BTA wore off and patients returned to normal daily activities.
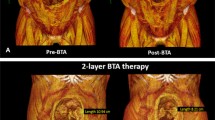
Imaging data for all 32 patients were available for comparison. Comparing baseline abdominal CT imaging with repeat imaging after BTA had taken effect-demonstrated significant elongation and thinning of the lateral abdominal wall muscles (Fig. 2). An increase in mean baseline abdominal wall length from 16.4 ± 4.0 to 20.4 ± 4.0 cm postBTA treatment per side (p < 0.0001) was seen, which translates to a gain in mean transverse length of the unstretched lateral abdominal oblique muscles of 4.0 cm/side (range 0–11.7 cm/side) (Table 1).
Patients with midline ventral hernias (n = 23) achieved the most benefit from BTA treatment. Midline hernias demonstrated a mean increase of 4.5 cm/side (p < 0.0001), and therefore a mean absolute gain of 9.0 cm in unstretched lateral abdominal wall length prior to surgery. A reduction in hernia defect size of up to 58 % was seen, as measured on axial CT imaging (Fig. 3).
All hernias were successfully repaired with intra-peritoneal onlay barrier mesh, either totally laparoscopical or LOL (Fig. 4A, B). Six patients received limited endoscopic central external oblique release (two unilateral, four bilateral) as an adjunct procedure. One patient underwent a simultaneous laparoscopic cholecystectomy for symptomatic cholelithiasis (with no complications from the added procedure).
The 30-day mortality rate was zero. There have been no hernia recurrences to date. Mean follow-up was 19 months (range 5–39 months).
Discussion
Botulinum toxin A has an ever-increasing range of clinical applications. BTA is a neurotoxin which is isolated and purified from Clostridium botulinum type A bacteria, it produces a reversible flaccid paralysis in affected muscles by blockade of the acetylcholine receptor at the neuromuscular junction [9]. BTA begins to take effect after 2–3 days and reaches maximal effect 1–2 weeks after administration, after which time there is a prolonged plateau of several months duration. Its effects then begin a slow decline, with an overall duration of effect of 4–6 months. This time course is highly reproducible [6]. BTA has a long history of documented safety and efficacy in a variety of conditions [4–10]. It has been shown to modulate pain perception and is particularly efficacious in treating pain caused by spastic muscular disorders. The effect of BTA on non-muscular pain syndromes such as migraine and amputation stump pain is promising, but still under investigation [5, 10]. Smoot et al. [5] described the first use of BTA for treating postoperative pain after ventral hernia repair in a patient intolerant of narcotic analgesics. Smoot’s group determines the anatomical locations for BTA injection that we currently use in our study (Fig. 1).
In our experience, the flaccid paralysis of the lateral abdominal wall musculature, imparted by BTA, serves multiple purposes:
-
1.
BTA is administered preoperatively so as to have achieved the desired effect by the time of surgery. In most patients, the prior relaxation of the lateral abdominal oblique muscles allows a partial or complete preoperative reduction of herniated intestine and solid viscera into the abdominal cavity (Fig. 5).
-
2.
Lateral traction forces naturally act at the midline in an intact abdomen. In patients with established fascial defects, these same forces serve to slowly enlarge the hernial defect. BTA minimizes these lateral traction forces and preoperatively decreases the size of the defect [7] (Fig. 3).
-
3.
The flaccid paralysis of lateral abdominal musculature induced by BTA allows closure of even giant hernias without excessive tension [7], and therefore avoiding postoperative abdominal hypertension, prolonged periods of ventilation, or respiratory distress. No patients in this cohort (up to a maximum defect width of 24 cm) experienced any such postoperative consequences of a repair performed under excessive tension.
-
4.
The extended period of BTA effect suggests that the repair line remains protected from physiological lateral tension forces for several months. It has been previously hypothesized that protection of the repair during the critical initial 3 months of wound healing could potentially reduce the incidence of wound dehiscence and hernia recurrence [4]. The results from this study appear to support such a statement, although a longer period of follow-up is required before conclusions can be drawn. The authors are currently investigating whether there is benefit to administering a postoperative, ‘top-up’ dose of BTA in select high-risk patients, to be administered once the initial paralysis begins to wear off. This would allow an even longer period of time for the wound to heal and strengthen.
Most patients included within this study required an extended period of preoperative workup, up to 6 months in some cases. A team approach is undertaken, with the patient actively involved in the process. A multidisciplinary team setting is utilized where the participants consist of a combination of surgeons, physicians, radiologists, research fellows, nurse educators, and microbiologists. Patients are discussed, and a management plan is formulated. Comorbidities are medically optimized with the appropriate specialists. Cessation of smoking is a prerequisite for patient inclusion in this program. Obese patients are educated about obesity and must demonstrate that they can lose some of their excess weight prior to surgery (surgery in some patients can be delayed several months while this occurs). Nutritionists and dieticians can become involved at this point. The consent process is lengthy and involves a discussion regarding the possibility of a staged procedure if required.
Six patients in this study underwent limited endoscopic central external oblique release as part of their operative procedure (four bilateral and two unilateral). Performed at the outset of each patient’s procedure, the release was performed in certain patients with exceptionally large defects to mitigate an anticipated difficulty with achieving closure, despite BTA treatment. The two unilateral releases were performed on patients with complex lateral ventral incisional hernias, measuring 10 cm × 9 cm and 13 cm × 16 cm, in order to medialize the laterally retracted rectus edge. The four bilateral releases were performed on midline ventral hernias with a mean defect width 18 cm. These patients were identified preoperatively as likely requiring an adjunct to BTA in order to provide fascial closure. The width of defect (>18–20 cm) was a substantial component of this decision making process. Further factors are number of previous abdominal procedures, number of prior repairs, and presence and amount of mesh in situ. All of these relate directly to the extent of abdominal wall scarring, fibrosis, and (lack of) tissue compliance, which may make fascial closure more difficult. The procedure described here, termed limited endoscopic ‘central external oblique release,’ is a modified version of the endoscopic component separation technique as reported by Rosen et al. [13]. The authors’ endoscopic central external oblique release involves a modified technique which does not require a dissecting balloon and commences at the tip of the 10th rib longitudinally to a point just medial to the anterior superior iliac spine. It does not require extensive disruption of tissue planes. The linea semilunaris is mapped preoperatively using ultrasound to identify relevant anatomy.
This study has several notable limitations. While this is the largest published series to date, the sample size is still relatively small, and there is a limited follow-up period.
Preoperative abdominal wall compliance was not measured, and therefore we have not directly measured the physiological effect of Botulinum toxin A. Our conclusions were derived indirectly from a measurable effect on imaging (muscle length and thickness) and clinical outcomes only.
There was no formal control arm to this study design, although patients did in essence act as their own controls. As each patient’s baseline (‘control’) abdominal CT imaging was objectively compared and measured with postBTA imaging, the difference between control and postintervention imaging demonstrates the effect of BTA in this clinical context.
A handful of patients notably had minimal measurable effect after BTA administration, as measured on serial CT imaging. During CT scanning, patients are asked to do a series of active maneuvers such as crunching and ballooning of their abdomen. Performance of these maneuvers is dependent on patients understanding the instructions given and having the ability and abdominal wall strength to perform and hold the maneuvers as requested. Other possibilities included inadequate dosage of BTA or even suboptimal injection locations of the BTA (i.e., not taking into consideration the full extent of lateral muscular retraction and adjusting injection locations accordingly), despite the fact that injections are undertaken under real-time ultrasound control.
Six patients underwent limited central external oblique release in conjunction with BTA administration due to an anticipated difficulty with closure, but which nonetheless confounds results. These patients were chosen preoperatively as likely requiring an adjunct to BTA (external oblique release), but a more scientifically robust way of testing this might be to attempt repair first, and if closure is deemed to be under excessive tension, then to deflate the abdomen and perform external oblique release.
Despite these shortcomings, our results to date are promising. Long-term follow-up is necessary to fully appreciate the potential of this technique.
Conclusions
Botulinum toxin A is a safe and effective technique, which is easy to perform and well tolerated. Its paralytic effects are prolonged and entirely reversible. Chemical component relaxation using BTA prior to complex ventral hernia repair facilitates fascial closure of hernia defects without disrupting the myofascial integrity of the abdominal wall. Hernias previously considered inoperable can become operable owing to the flaccid paralysis conferred by BTA and its ability to relax and elongate the contracted lateral oblique muscles. The vast majority of these procedures can be completed laparoscopically. Administration of BTA also has the added benefits of modulating postoperative pain and offers a prolonged reduction in lateral traction forces on the midline wound, thereby potentially protecting the healing repair for an extended period of time. This study demonstrates that BTA has significant potential as a preoperative adjunct in the laparoscopic repair of complex ventral hernia.
References
Deerenberg EB, Timmermans L, Hogerzeil DP, Slieker JC, Eilers PHC, Jeekel J, Lange JF (2015) A systematic review of the surgical treatment of large incisional hernia. Hernia 19:89–101
Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M, Kercher KW, Lammers BJ, Parra-Davilla E, Roll S, Towfigh S, van Geffen E (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18:7–17
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237(1):129–135
Zendejas B, Khasawneh MA, Srvantstyan B, Jenkins DH, Schiller HJ, Zielinksi MD (2013) Outcomes of chemical component paralysis using Botulinum toxin for incisional hernia repairs. World J Surg 37:2830–2837
Smoot D, Zielinski M, Jenkins D, Schiller H (2011) Botox A injection for pain after laparoscopic ventral hernia: a case report. Pain Med 12:1121–1123
Barwood S, Baillieu C, Boyd R, Brereton K, Low J, Nattrass G, Graham HK (2000) Analgesic effects of Botulinum toxin A: a randomized, placebo-controlled clinical trial. Dev Med Child Neurol 42:116–121
Ibarra-Hurtado TR, Nuno-Guzman CM, Echeagaray-Herrera JE, Robles-Velez E, de Jesus G-JJ (2009) Use of botulinum toxin type A before abdominal wall hernia reconstruction. World J Surg 33:2553–2556
Ibarra-Hurtado TR, Nuno-Guzman CM, Miranda-Diaz AG, Troyo-Sanroman R, Navarro-Ibarra R, Bravo-Cuellar L (2014) Effect of Botulinum toxin A in lateral abdominal wall muscles thickness and length of patients with midline incisional hernia secondary to open abdomen management. Hernia 18:647–652
Zielinski MD, Goussous N, Schiller HJ, Jenkins D (2013) Chemical components separation with Botulinum toxin A: a novel technique to improve primary fascial closure rates of the open abdomen. Hernia 17:101–107
Dressler D (2012) Clinical applications of botulinum toxin. Curr Opin Microbiol 15:325–333
Farooque F, Jacombs AS, Roussos R, Read JW, Dardano AN, Edye M, Ibrahim N (2016) Preoperative abdominal muscle elongation with Botulinum toxin A for complex incisional ventral hernia repair. ANZ J Surg 86:79–83
Elstner KE, Jacombs ASW, Read JW, Rodriguez O, Edye M, Cosman PH, Dardano AN, Zea A, Boesel T, Mikami DJ, Craft C, Ibrahim N (2016) Laparoscopic repair of complex ventral hernia facilitated by pre-operative chemical component relaxation using Botulinum toxin A. Hernia. doi:10.1007/s10029-016-1478-6
Rosen MJ, Jin J, McGee MF, Williams C, Marks J, Ponsky JL (2007) Laparoscopic component separation in the single-stage treatment of infected abdominal wall prosthetic removal. Hernia 11:435–440
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kristen E. Elstner, Omar Rodriguez-Acevedo, Peter H. Cosman, Anita S. W. Jacombs, Michael Edye, Aaron Zea, Tillman Boesel, Dean J. Mikami, and Nabeel Ibrahim declare no conflict of interest or financial ties to disclose. John W. Read declares conflict of interest related to the submitted work as he receives financial remuneration from Medicare as a radiologist. Anthony N. Dardano declares conflict of interest not directly related to the submitted work in the form of Honorarium from biomedical companies Cook, Synthes, and KCI.
Rights and permissions
About this article
Cite this article
Elstner, K.E., Read, J.W., Rodriguez-Acevedo, O. et al. Preoperative chemical component relaxation using Botulinum toxin A: enabling laparoscopic repair of complex ventral hernia. Surg Endosc 31, 761–768 (2017). https://doi.org/10.1007/s00464-016-5030-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5030-7