Abstract
Background
In medical practice, the tendency to remove an inflamed gallbladder is deeply rooted. Cholecystectomy, however, is associated with relatively high complication rates, and therefore the decision whether or not to perform surgery should be well considered. For some patients, the surgical risk–benefit profile may favour conservative treatment. The objective of this study was to examine the short- and long-term outcome of conservative treatment of patients with acute calculous cholecystitis.
Methods
A systematic search of MEDLINE, Embase and Cochrane Library databases was performed. Prospective studies reporting on the success rate of conservative treatment (i.e. non-invasive treatment) of acute cholecystitis during index admission were included, as well as prospective and retrospective studies reporting on the recurrence rate of gallstone-related disease during long-term follow-up (i.e. ≥12 months) after initial non-surgical management. Study selection was undertaken independently by two reviewers using predefined criteria. The risk of bias was assessed. The pooled success and mortality rate during index admission and the pooled recurrence rate of gallstone-related disease during long-term follow-up were calculated using a random-effects model.
Results
A total of 1841 patients were included in 10 randomized controlled trials and 14 non-randomized studies. Conservative treatment during index admission was successful in 87 % of patients with acute calculous cholecystitis and in 96 % of patients with mild disease. In the long term, 22 % of the patients developed recurrent gallstone-related disease. Pooled analysis showed a success rate of 86 % (95 % CI 0.8–0.9), a mortality rate of 0.5 % (95 % CI 0.001–0.009) and a recurrence rate of 20 % (95 % CI 0.1–0.3).
Discussion
Conservative treatment of acute calculous cholecystitis during index admission seems feasible and safe, especially in patients with mild disease. During long-term follow-up, less than a quarter of the patients appear to develop recurrent gallstone-related disease, although this outcome is based on limited data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Western countries, acute calculous cholecystitis is a common disease with a high socio-economic impact. Cholecystectomy is considered the treatment of choice in patients deemed fit for surgery [1–4]. In surgical practice, cholecystectomy is one of the most frequently performed procedures, mostly performed by laparoscopy nowadays. The rationale for cholecystectomy is based on the old adage that an inflammatory focus should be eliminated immediately from the body to prevent clinical deterioration.
Even though cholecystectomy is the treatment of choice, the benefit of surgery in case of acute calculous cholecystitis has never been properly researched. Prospective, let alone randomized studies demonstrating superiority of surgical over conservative treatment are lacking. Performing cholecystectomy in case of acute cholecystitis prevents further episodes of gallstone-related disease, but the relatively high complication rate associated with both early and delayed cholecystectomy (i.e. 15 and 30 %, respectively [5]), especially in high-risk patients, should not go unnoticed. The decision to perform surgery should therefore be well considered. Conservative treatment prevents the surgical risk; however, leaving the gallbladder in situ may cause recurrent gallstone-related disease.
To assess whether it is safe (or even safer) to leave the gallbladder in situ in patients with acute calculous cholecystitis, the feasibility and safety of conservative treatment during index admission should be assessed. Subsequently, the recurrence rate of gallstone-related disease during long-term follow-up should be evaluated. It has been demonstrated that delayed cholecystectomy is associated with significant higher complication rates than early cholecystectomy [5], and therefore conservative treatment is only feasible if a delayed cholecystectomy is not required.
The aim of this study was to assess the available evidence concerning the feasibility of conservative treatment of acute calculous cholecystitis. The question for this review is thus twofold: (1) Is conservative treatment for acute calculous cholecystitis effective and safe during index admission? (2) What is the recurrence rate of gallstone-related disease during long-term follow-up?
Methods
A systematic review was conducted following the guidance of the Centre for Reviews and Dissemination concerning undertaking reviews in health care and reported in accordance with the PRISMA statement [6, 7].
Literature search
In May 2015, two authors (C. L. and J. O.) independently performed a literature search to identify studies reporting on conservative treatment for adults suffering from acute calculous cholecystitis. MEDLINE, Embase and Cochrane Library databases were searched for papers using the keywords: “acute cholecystitis” in combination with “conservative” or “antibiotic” or “anti-bacterial” or “non-invasive” or “non-surgical” or “non-operative” or “observation” or “drain” or “cholecystostomy” or “delayed/interval/planned/elective/late cholecystectomy”. The search was limited to articles published in English and Dutch and published after January 1990.
Study selection
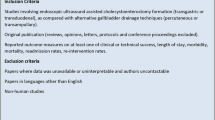
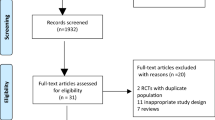
All titles and abstracts of publications were independently identified and reviewed for relevance by two authors (C. S. and J. O.), with referral to a third author (D. B.) to resolve queries in case of discordant opinions. Subsequently, full-text papers were retrieved and checked. A cross-reference search of the remaining articles was performed to identify other studies previously missed. In case of unclear methods or results, authors were contacted to seek clarification. If the same data were reported in two or more publications, the most comprehensive paper was selected. Reviews, case reports, unpublished data as well as articles of which no full text was available were excluded (Fig. 1).
Conservative treatment during index admission was defined as non-invasive management of acute calculous cholecystitis, i.e. supportive care with or without antibiotics. Uneventful resolution of symptoms without the need for intervention was considered as a successful conservative treatment. To reduce the risk of bias, only prospective studies were included.
To evaluate the long-term success of non-surgical management of acute calculous cholecystitis, the inclusion criteria were adjusted. Only studies with at least 12-month follow-up and explicit information on the recurrence of gallstone-related disease were included. Studies describing patients who initially underwent percutaneous cholecystostomy were also eligible, since these patients still have their gallbladder in situ after initial successful non-surgical treatment of acute calculous cholecystitis and may therefore develop recurrent gallstone disease. Due to the limited amount of prospective studies with long-term follow-up, retrospective studies were also included.
Data extraction
Data were extracted by two independent authors (C. S. and J. O.) with referral to a third author (D. B.) in case of any disagreements. The characteristics of the included studies are visualized in Tables 1 and 2.
Validity assessment
The methodological quality of the articles was independently assessed by both authors. The MINORS scoring scale was used to assess the risk of bias in non-randomized studies, with a global ideal score of 16 (Table 3) [8]. The Cochrane Collaboration’s tool was used to assess the risk of bias in randomized controlled trials (Table 4) [9].
Data analysis
The pooled success and mortality rate of conservative treatment during index admission and the pooled recurrence rate of gallstone-related disease during long-term follow-up were calculated with a random-effects model, using meta-analysis software version 3.1. Statistical heterogeneity among the included studies was determined by using forest plots, by performing a χ 2 (“Chi-squared”) heterogeneity test and by calculating the I 2-index. A high I 2-index represents a high suspicion of heterogeneity. All pooled event rates were shown in forest plots despite the level of heterogeneity.
Results
Figure 1 shows the article selection according to the PRISMA statement [6, 7]. A total of 1343 references were identified from medical journal databases. No new articles were identified by cross-reference search. After removing duplicates, 1169 potentially relevant studies were screened based on title and abstract, leaving 60 full manuscripts to be assessed for eligibility concerning efficacy of conservative treatment during index admission and 71 manuscripts concerning long-term outcome of non-surgical treatment of acute calculous cholecystitis. As a result of this assessment, inclusion criteria were met in 14 and 10 studies, respectively. There was total agreement among the authors regarding the inclusion of studies.
Conservative treatment of acute calculous cholecystitis during index admission
Fourteen prospective studies, either randomized [10–17] or non-randomized [18–22], were included. Seven trials [10, 12, 13, 16, 17, 21, 23] were designed to compare emergency cholecystectomy with delayed cholecystectomy. Patients assigned to delayed cholecystectomy were treated conservatively during index admission, followed by elective laparoscopic cholecystectomy several weeks after discharge. Data of these patients were used to assess the success rate of conservative treatment during index admission. Three studies [14, 15, 22] were designed to compare conservative management with another treatment for acute calculous cholecystitis (e.g. sphincterotomy or cholecystostomy), whereas in the remaining studies [11, 18–20], all patients were treated by means of conservative management.
Table 1 shows the characteristics of the included studies. A total of 1315 patients with acute calculous cholecystitis were analysed. The severity of cholecystitis was explicitly reported in three studies [10, 11, 18]; all three concerned patients with mild cholecystitis. One study [14] excluded patients that required urgent surgical or percutaneous management, thus probably severely ill patients. In the remaining studies, the severity of cholecystitis was not mentioned [12, 13, 16, 17, 19–23].
Outcome
A total of 1315 patients, included in 14 studies, were treated conservatively for acute calculous cholecystitis, of whom 1137 (87 %) showed an uneventful resolution of symptoms without the need for intervention. Conservative treatment included bowel rest and intravenous administration of broad-spectrum antibiotics and fluids. Table 1 shows specific information about the antibiotic treatment, as far as described in detail in the articles. Failure of conservative treatment was determined at the discretion of the attending surgeon based on subjective findings, such as lack of improvement, or objective findings, such as worsening of clinical signs and laboratory results. In case of failure of conservative treatment, either emergency cholecystectomy [13, 15–18, 21–23] or percutaneous cholecystostomy [11, 19, 20] was performed.
The mortality rate associated with conservative treatment during index admission was 0.8 % (11 of 1315) [10–23]. The highest mortality rate (17 %) was reported by Hatzidakis et al. [15]. This study included 42 high-surgical-risk patients with an APACHE-II score ≥12, of whom seven died during index admission.
A total of 245 patients diagnosed with explicitly mentioned mild cholecystitis were included in three studies [10, 11, 18]. In this specific group, conservative treatment was successful in 96 % (236 of 245). Only nine patients required intervention due to failure of conservative treatment, of whom seven underwent percutaneous cholecystostomy and two cholecystectomy. Mortality in this group was nil. Mean length of hospital stay was mentioned in only one study and was 4 days [11].
The pooled success rate of conservative treatment during index admission was 86 % (95 % CI 0.8–0.9) (Fig. 2). There was a strong heterogeneity among the included studies (I 2 = 95 %). A pooled analysis of only randomized controlled trials showed a success rate of 91 % (95 % CI 0.9–1.0) with an I 2-index of 82 % (forest plot not shown). The pooled mortality rate of conservative treatment during index admission was 0.5 % (95 % CI 0.001–0.009) with an I 2-index of 0 % (Fig. 3).
Long-term outcome of non-surgical treatment of acute calculous cholecystitis
To evaluate the long-term outcome of conservative treatment, ten studies were included: two randomized controlled trials [15, 24], three retrospective studies of prospectively collected data [25–27] and five retrospective studies [28–32]. The characteristics of the selected studies are summarized in Table 2. A total of 526 patients, who were initially treated conservatively for acute calculous cholecystitis, and in whom cholecystectomy was not electively planned, were analysed. Follow-up ranged from 12 months to 5 years. One randomized controlled trial [24] was specifically designed to examine the long-term efficacy of complete conservative treatment versus immediate surgery in non-high-risk patients with acute calculous cholecystitis.
Outcome
During long-term follow-up, 117 of the 526 patients (22 %) developed recurrence of gallstone-related disease after initial non-surgical treatment of acute calculous cholecystitis. The recurrence rate varied substantially across the included studies and ranged from 3 to 47 %. The definition of recurrence of gallstone disease differed between studies. Eight studies [25, 27–32] described recurrent gallstone disease only as recurrence of acute calculous cholecystitis, whereas two studies [24, 26] included all gallstone-related problems. The randomized controlled trial specifically designed to examine the long-term efficacy of complete conservative treatment included 33 patients, of whom 10 (30 %) experienced gallstone-related events during a median follow-up of 14 years [24].
The time from initial treatment to recurrence varied between the included studies, but the recurrence mainly occurred within 2 years after initial cholecystitis: three studies [15, 26, 32] reported a range from 2 to 24 months, one study reported a mean of 14 months [29], and two studies reported a median of 2 [28] and 15 months [24]. Recurrent diseases were successfully controlled by conservative medical measurements [26, 27, 32], cholecystectomy [24, 30, 31] or percutaneous cholecystostomy [25, 28].
The pooled recurrence rate of gallstone-related disease during long-term follow-up was 19.7 % (95 % CI 0.1–0.3) (Fig. 4). There was a strong heterogeneity among the included studies (I 2 = 90 %). When dividing the included studies in two groups based on duration of follow-up, a pooled recurrence rate of 22 % (95 % CI 0.06–0.04) was found for studies with a follow-up of <2 years (I 2 = 87 %) and a recurrence rate of 18 % (95 % CI 0.04–0.3) for studies with a follow-up of >2 years (I 2 = 93 %) (forest plot not shown).
Quality assessment of the included studies
The results of the methodological quality assessment of the included studies are shown in Tables 3 and 4. Ten studies [10–17, 23, 24] were randomized controlled trials, eight studies [18–22, 25–27] collected data according to a protocol established before the commencement of the study, whereas five studies [28–32] did not have such protocol and identified all patients retrospectively. None of the studies had blinded evaluation of the endpoint due to the nature of the intervention and study. Overall, the included studies were of an estimated moderate quality.
Discussion
This systematic review demonstrates that conservative treatment during index admission is successful in 87 % of all patients with acute calculous cholecystitis. Especially in mild acute cholecystitis, conservative treatment appears safe and effective: 96 % of the patients showed uneventful resolution of symptoms without the need for intervention. After initial non-surgical treatment, 22 % of the patients developed recurrent biliary symptoms, mainly within 2 years after initial cholecystitis. Pooled analysis shows comparable results. According to a randomized controlled trial [24] with a median follow-up of 14 years, the likelihood of recurrent gallstone disease was slightly higher (30 %), but this study included only 33 patients.
When comparing surgical with non-surgical treatment, and determining the feasibility of the latter, not just the likelihood of recurrence but also the surgical risk of the patient should be regarded. In patients with advanced age and/or severe comorbidities, the risk of recurrence is anyhow reduced, due to a relatively limited survival time [33]. In these patients, non-surgical management can be considered as a definitive treatment. Younger, non-high-risk patients would probably easier withstand conservative treatment compared to their older counterparts, but in the same time, are exposed to an increased risk of recurrence due to their longer life expectancy. In view of prevention of future episodes of gallstone disease, cholecystectomy might be a reasonable choice [24]. Nevertheless, the risk–benefit profile shifts towards non-operative management, considering the fact that a second episode of cholecystitis might never occur, as well as the relatively high complication rate associated with cholecystectomy [23].
In medical practice, the tendency to remove an inflamed gallbladder is deeply rooted, even though high-quality evidence is lacking. As in case of cholecystitis, in other acute gastrointestinal inflammations the benefit of surgery over conservative care is not always clearly demonstrated, and therefore, treatment algorithms (in select cases) are slowly shifting towards conservative management. In case of uncomplicated acute diverticulitis, conservative treatment seems feasible and safe [34, 35]; so surgery should be reserved for cases with significant complications, unresponsive to medical treatment [36]. Also in acute appendicitis, randomized trials have shown feasibility and safety of initial non-surgical management [37]. A comparable management algorithm for (mild) acute calculous cholecystitis is plausible [30].
Is it possible to identify patients for whom conservative treatment is most suitable? Concerning the severity of cholecystitis, it seems clear that, without any doubt, conservative treatment during index admission is feasible in mild cases. Concerning the long-term outcome of conservatively treated mild cholecystitis, no definitive conclusions could be drawn, since all (but one) studies with long-term follow-up concerned high-risk patients and none reported on the initial severity of cholecystitis. But given the fact that the overall recurrence rate of biliary symptoms never exceeded one-third of the patients, a conservative approach during follow-up is justified. From the available data of the included studies, it was not possible to identify other factors that might determine the feasibility of conservative treatment.
The success rate of conservative treatment found in this systematic review may have been influenced by several factors. Firstly, studies not reporting on the failure rate of conservative treatment were not included, since it was unclear whether failure had not been mentioned by the authors or did not occur at all. Since the latter is most likely, the success rate of conservative treatment in this review might be underestimated. Secondly, the definition of recurrent gallstone disease differed per study. Some studies described recurrent gallstone-related disease as acute cholecystitis, not reporting whether other complications (e.g. gallstone attack) did not occur or had not been reported. Therefore, the recurrence rate might have been underestimated. Lastly, the duration of follow-up varied substantially between the studies, ranging from one to 14 years. In studies with a relatively short follow-up, a recurrence after follow-up could have been developed, and therefore the recurrence rate might be underestimated. However, the majority of recurrences occur within 2 years after initial cholecystitis, and the risk of new gallstone-related disease decreases over time. Vethrus et al. [14] showed that more than 70 % of the events occurred within 20 months after acute cholecystitis. Similar results regarding the development of complications have been found in patients with symptomatic uncomplicated gallstones [38].
There was a strong heterogeneity among the included studies, demonstrated by the high I 2-values. Possible explanations include differences in sample size, patients characteristics (e.g. age, comorbidities, duration of symptoms, severity of cholecystitis) and antibiotic regimens (e.g. type of antibiotics and duration of treatment) between the included studies. The pooled mortality rate of 0.5 %, on the other hand, was associated with an I 2-index of 0 %, enabling us to conclude that during index admission, conservative treatment of acute cholecystitis is indeed associated with a low mortality.
Cancer may be present in a gallbladder complicated with acute cholecystitis. A large retrospective study of 2700 patients with acute calculous cholecystitis managed with cholecystectomy showed that malignant pathologies were found in 2.3 % of the patients [39]. Gallbladder cancer was most frequently diagnosed in women and patients with advanced age. In our hospital, 590 patients with acute calculous cholecystitis underwent laparoscopic cholecystectomy between 2002 and 2015; pathological examination of the gallbladder showed malignant pathologies in 2 patients (0.3 %). Imaging modalities such as endoscopic ultrasonography, computed tomography and magnetic resonance imaging are useful to diagnose gallbladder cancer [40, 41]. With these figures, however, it is debatable whether additional imaging studies to diagnose malignancies should be performed in all conservatively treated patients.
This systematic review implicates that conservative treatment in case of acute cholecystitis is a feasible treatment option. There is, however, insufficient evidence to demonstrate actual superiority of conservative treatment over cholecystectomy for this indication. Currently, we are designing a prospective randomized controlled trial comparing both treatment options in patients with mild acute calculous cholecystitis.
To determine superiority of one or the other treatment strategy, not only the technical aspects but also the expenditures of both strategies should be evaluated. The costs of emergency cholecystectomy have been subject to many studies, whereas studies focussing on the economic aspects of conservative treatment are lacking. When comparing early with delayed cholecystectomy for acute cholecystitis, total hospital costs are significantly lower for early cholecystectomy [23, 42, 43]. Since our study, however, shows that only 22 % of the patients need to be readmitted for recurrent gallstone-related disease, of whom only some need a surgical re-intervention, the total costs of conservative treatment may be reduced compared to emergency cholecystectomy. A randomized controlled trial and a complementary research using economic and public health approaches including assessment of quality of life, direct and indirect costs are needed.
To the best of our knowledge, this is the first systematic review examining short- and long-term outcome of conservative treatment of patients with acute calculous cholecystitis. Based on the best available evidence, conservative treatment of acute calculous cholecystitis during index admission seems feasible and safe, especially in patients with mild disease. During long-term follow-up, about a quarter of the patients seem to develop recurrent gallstone disease, although this is based on limited data.
References
Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O’Neill PJ, Chow AW, Dellinger EP, Eachempati SR, Gorbach S, Hilfiker M, May AK, Nathens AB, Sawyer RG, Bartlett JG (2010) Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Surg Infect (Larchmt) 11:79–109. doi:10.1089/sur.2009.9930
The Dutch guidelines for gallstone disease (web site). http://www.heelkunde.nl/uploads/_6/re/_6reZZkgrYUAuCG6uvcN-A/richtlijn_galsteen.pdf. Accessed July 2015
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Hata J, Gabata T, Yoshida M, Miura F, Okamoto K, Tsuyuguchi T, Itoi T, Yamashita Y, Dervenis C, Chan AC, Lau WY, Supe AN, Belli G, Hilvano SC, Liau KH, Kim MH, Kim SW, Ker CG, Committee Tokyo Guidelines Revision (2013) TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 20:35–46. doi:10.1007/s00534-012-0568-9
Mayumi T, Takada T, Kawarada Y, Nimura Y, Yoshida M, Sekimoto M, Miura F, Wada K, Hirota M, Yamashita Y, Nagino M, Tsuyuguchi T, Tanaka A, Gomi H, Pitt HA (2007) Results of the Tokyo consensus meeting Tokyo guidelines. J Hepatobiliary Pancreat Surg 14:114–121. doi:10.1007/s00534-006-1163-8
Cao AM, Eslick GD, Cox MR (2015) Early cholecystectomy is superior to delayed cholecystectomy for acute cholecystitis: a meta-analysis. J Gastrointest Surg 19:848–857. doi:10.1007/s11605-015-2747-x
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34. doi:10.1016/j.jclinepi.2009.06.006
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med 3:e123–e130
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. doi:10.1046/j.1445-2197.2003.02748.x
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi:10.1136/bmj.d5928
Agrawal R, Sood KC, Agarwal B (2015) Evaluation of early versus delayed laparoscopic cholecystectomy in acute cholecystitis. Surg Res Pract 2015:349801. doi:10.1155/2015/349801
Mazeh H, Mizrahi I, Dior U, Simanovsky N, Shapiro M, Freund HR, Eid A (2012) Role of antibiotic therapy in mild acute calculus cholecystitis: a prospective randomized controlled trial. World J Surg 36:1750–1759. doi:10.1007/s00268-012-1572-6
Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, Seenu V (2004) Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc 18:1323–1327. doi:10.1007/s00464-003-9230-6
Johansson M, Thune A, Blomqvist A, Nelvin L, Lundell L (2003) Management of acute cholecystitis in the laparoscopic era: results of a prospective, randomized clinical trial. J Gastrointest Surg 7:642–645. doi:10.1016/S1091-255X(03)00065-9
Vetrhus M, Soreide O, Nesvik I, Sondenaa K (2003) Acute cholecystitis: delayed surgery or observation. A randomized clinical trial. Scand J Gastroenterol 38:985–990
Hatzidakis AA, Prassopoulos P, Petinarakis I, Sanidas E, Chrysos E, Chalkiadakis G, Tsiftsis D, Gourtsoyiannis NC (2002) Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol 12:1778–1784. doi:10.1007/s00330-001-1247-4
Lai PB, Kwong KH, Leung KL, Kwok SP, Chan AC, Chung SC, Lau WY (1998) Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 85:764–767. doi:10.1046/j.1365-2168.1998.00708.x
Lo CM, Liu CL, Fan ST, Lai EC, Wong J (1998) Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg 227:461–467
Rodriguez-Cerrillo M, Poza-Montoro A, Fernandez-Diaz E, Inurrieta-Romero A, Matesanz-David M (2012) Home treatment of patients with acute cholecystitis. Eur J Intern Med 23:e10–e13. doi:10.1016/j.ejim.2011.07.012
Barak O, Elazary R, Appelbaum L, Rivkind A, Almogy G (2009) Conservative treatment for acute cholecystitis: clinical and radiographic predictors of failure. Isr Med Assoc J 11:739–743
Paran H, Zissin R, Rosenberg E, Griton I, Kots E, Gutman M (2006) Prospective evaluation of patients with acute cholecystitis treated with percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Int J Surg 4:101–105. doi:10.1016/j.ijsu.2006.01.001
Serralta AS, Bueno JL, Planells MR, Rodero DR (2003) Prospective evaluation of emergency versus delayed laparoscopic cholecystectomy for early cholecystitis. Surg Laparosc Endosc Percutan Tech 13:71–75
Vracko J, Markovic S, Wiechel KL (2006) Conservative treatment versus endoscopic sphincterotomy in the initial management of acute cholecystitis in elderly patients at high surgical risk. Endoscopy 38:773–778. doi:10.1055/s-2006-925448
Gutt CN, Encke J, Koninger J, Harnoss JC, Weigand K, Kipfmuller K, Schunter O, Gotze T, Golling MT, Menges M, Klar E, Feilhauer K, Zoller WG, Ridwelski K, Ackmann S, Baron A, Schon MR, Seitz HK, Daniel D, Stremmel W, Buchler MW (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg 258:385–393. doi:10.1097/SLA.0b013e3182a1599b
Schmidt M, Sondenaa K, Vetrhus M, Berhane T, Eide GE (2011) Long-term follow-up of a randomized controlled trial of observation versus surgery for acute cholecystitis: non-operative management is an option in some patients. Scand J Gastroenterol 46:1257–1262. doi:10.3109/00365521.2011.598548
Rodriguez-Sanjuan JC, Arruabarrena A, Sanchez-Moreno L, Gonzalez-Sanchez F, Herrera LA, Gomez-Fleitas M (2012) Acute cholecystitis in high surgical risk patients: percutaneous cholecystostomy or emergency cholecystectomy? Am J Surg 204:54–59. doi:10.1016/j.amjsurg.2011.05.013
Melloul E, Denys A, Demartines N, Calmes JM, Schafer M (2011) Percutaneous drainage versus emergency cholecystectomy for the treatment of acute cholecystitis in critically ill patients: does it matter? World J Surg 35:826–833. doi:10.1007/s00268-011-0985-y
Griniatsos J, Petrou A, Pappas P, Revenas K, Karavokyros I, Michail OP, Tsigris C, Giannopoulos A, Felekouras E (2008) Percutaneous cholecystostomy without interval cholecystectomy as definitive treatment of acute cholecystitis in elderly and critically ill patients. South Med J 101:586–590. doi:10.1097/SMJ.0b013e3181757b77
Horn T, Christensen SD, Kirkegard J, Larsen LP, Knudsen AR, Mortensen FV (2015) Percutaneous cholecystostomy is an effective treatment option for acute calculous cholecystitis: a 10-year experience. HPB (Oxford) 17:326–331. doi:10.1111/hpb.12360
Chang YR, Ahn YJ, Jang JY, Kang MJ, Kwon W, Jung WH, Kim SW (2014) Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and re-evaluation of treatment efficacy. Surgery 155:615–622. doi:10.1016/j.surg.2013.12.026
McGillicuddy EA, Schuster KM, Barre K, Suarez L, Hall MR, Kaml GJ, Davis KA, Longo WE (2012) Non-operative management of acute cholecystitis in the elderly. Br J Surg 99:1254–1261. doi:10.1002/bjs.8836
Andren-Sandberg A, Haugsvedt T, Larssen TB, Sondenaa K (2001) Complications and late outcome following percutaneous drainage of the gallbladder in acute calculous cholecystitis. Dig Surg 18:393–398. doi:10.1159/000050180
Hamy A, Visset J, Likholatnikov D, Lerat F, Gibaud H, Savigny B, Paineau J (1997) Percutaneous cholecystostomy for acute cholecystitis in critically ill patients. Surgery 121:398–401. doi:10.1016/S0039-6060(97)90309-3
Li M, Li N, Ji W, Quan Z, Wan X, Wu X, Li J (2013) Percutaneous cholecystostomy is a definitive treatment for acute cholecystitis in elderly high-risk patients. Am Surg 79:524–527
Beckham H, Whitlow CB (2009) The medical and nonoperative treatment of diverticulitis. Clin Colon Rectal Surg 22:156–160. doi:10.1055/s-0029-1236159
Unlu C, Gunadi PM, Gerhards MF, Boermeester MA, Vrouenraets BC (2013) Outpatient treatment for acute uncomplicated diverticulitis. Eur J Gastroenterol Hepatol 25:1038–1043. doi:10.1097/MEG.0b013e328361dd5b
Bauer VP (2009) Emergency management of diverticulitis. Clin Colon Rectal Surg 22:161–168. doi:10.1055/s-0029-1236160
Mason RJ (2008) Surgery for appendicitis: is it necessary? Surg Infect (Larchmt) 9:481–488. doi:10.1089/sur.2007.079
Friedman GD, Raviola CA, Fireman B (1989) Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol 42:127–136. doi:10.1016/0895-4356(89)90086-3
Lam CM, Yuen AW, Wai AC, Leung RM, Lee AY, Ng KK, Fan ST (2005) Gallbladder cancer presenting with acute cholecystitis: a population-based study. Surg Endosc 19:697–701. doi:10.1007/s00464-004-9116-2
Oikarinen H (2006) Diagnostic imaging of carcinomas of the gallbladder and the bile ducts. Acta Radiol 47:345–358
Andren-Sandberg A (2012) Diagnosis and management of gallbladder cancer. N Am J Med Sci 4:293–299. doi:10.4103/1947-2714.98586
Wilson E, Gurusamy K, Gluud C, Davidson BR (2010) Cost-utility and value-of-information analysis of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 97:210–219. doi:10.1002/bjs.6872
Johner A, Raymakers A, Wiseman SM (2013) Cost utility of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc 27:256–262. doi:10.1007/s00464-012-2430-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Loozen, Dr. Oor, Dr. Van Ramshorst, Dr. Van Santvoort and Dr. Boerma have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Loozen, C.S., Oor, J.E., van Ramshorst, B. et al. Conservative treatment of acute cholecystitis: a systematic review and pooled analysis. Surg Endosc 31, 504–515 (2017). https://doi.org/10.1007/s00464-016-5011-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5011-x