Abstract
Background
Prolonged ileus is one of the most common postoperative complications after colorectal surgery. We sought to investigate the predictors of prolonged ileus following elective colon resections procedures.
Methods
The national participant user files of NSQIP databases were utilized to examine the clinical outcomes of patients undergoing elective colon resection during 2012–2013. Multivariate regression analysis was performed to investigate predictors of prolonged ileus. Prolonged ileus was defined as no return of bowel function in 7 days.
Results
We sampled a total of 27,560 patients who underwent colon resections; of these, 3497 (12.7 %) patients had prolonged ileus. Patients with ileocolonic anastomosis (ICA) had a significantly higher rate of prolonged ileus compared to patients with colorectal anastomosis (CRA) (15 vs. 11.5 %, AOR 1.25, P < 0.01). Prolonged ileus was significantly associated with intra-abdominal infections (13 vs. 2.8 %, AOR 2.56, P < 0.01) and anastomotic leakage (12 vs. 2.4 %, AOR 2.50, P < 0.01). Factors such as preoperative sepsis (AOR 1.63, P < 0.01), disseminated cancer (AOR 1.24, P = 0.01), and chronic obstructive pulmonary disease (AOR 1.27, P = 0.02) were associated with an increased risk of prolonged ileus, whereas oral antibiotic bowel preparation (AOR 0.77, P < 0.01) and laparoscopic surgery (AOR 0.51, P < 0.01) are associated with decreased prolonged ileus risk.
Conclusions
Prolonged ileus is a common condition following colon resection, with an incidence of 12.7 %. Among colon surgeries, colectomy with ICA resulted in the highest rate of postoperative prolonged ileus. Prolonged ileus is positively associated with anastomotic leak and intra-abdominal infections; thus, a high index of suspicion must be had in all patients with prolonged postoperative ileus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prolonged ileus in the postoperative period has an incidence of 10–17 % and is one of the most common complications following colorectal surgery [1–3]. Paralytic ileus is an important cause of prolonged hospitalization and readmission [4, 5]. It is estimated that prolonged ileus costs $750 million annually in the USA [5]. Therefore, it is important to recognize the risk factors prior to operation in order to decrease the rate in this patient population.
Several pathways have been proposed to mitigate postoperative ileus [6]. Unlike ileus, which is a normal phenomenon after intra-abdominal surgery, prolonged ileus may be a sign of an underlying severe complication [1, 2, 7]. Inhibitory gastrointestinal tract reflexes, local inflammatory responses, and pharmacologic interactions have all been reported as triggers of postoperative ileus [6, 8–10]. A number of patient characteristics and perioperative risk factors for prolonged ileus have been identified, such as chronic pulmonary disease, male sex, smoking status, prolonged total surgical time, and total opiate dose [3, 11]. Use of opioid-sparing analgesic techniques and non-steroidal anti-inflammatory agents has been suggested as some ways to decrease the duration of postoperative ileus [6]. Although a number of studies have reported that the highest rates of postoperative prolonged ileus rate occur after colorectal surgery, a nationwide study investigating the predictors of prolonged ileus in colorectal operations is lacking [6, 12]. Using the American College of Surgeons’ National Surgical Quality Program database, this study aims to investigate the rate of paralytic ileus in elective colon resections and report the predictors of paralytic ileus in colon surgery.
Materials and methods
A retrospective cohort study was conducted using national participant user files and colectomy target files of the American College of Surgeons’ National Surgical Quality Improvement Program (ACS NSQIP) database during 2012–2013. ACS NSQIP is a nationwide surgical outcome-based database which provides preoperative through 30-day postoperative information based on clinical data in the USA [13]. We analyzed the available data on adult patients who underwent elective partial colon resection. The appropriate procedure codes as specified by the Current Procedural Terminology (CPT) codes were utilized: 44140 and 44202 for partial colectomy with colocolonic anastomosis (CCA), 44145 and 44207 for partial colectomy with colorectal anastomosis (CRA), and 44160 and 44205 for partial colectomy with ileocolonic anastomosis (ICA). Patients’ diagnoses were defined based on the International Classification of Diseases, Ninth Revision, clinical modifications (ICD-9-CM) codes of 153, 153.0–154.0 for colon cancer, 211.3 for benign tumors, 562.10–562.13 for diverticular disease, 564.7 and 564.00–564.09 for constipation, 555.0–555.9 for Crohn’s disease, 569.1 for rectal prolapse, and 556.0–556.9 for ulcerative colitis. We excluded all patients who underwent stoma creation as a part of the procedure. Also, patients who underwent total colectomy were excluded from the study because the CPT code for total colectomy does not indicate which patients had an end ileostomy versus an ileorectal anastomosis. Paralytic ileus was defined as no return of bowel function within 7 days of operation.
Patient variables that were analyzed are as follows: demographic data (age, sex, and race); comorbid conditions such as congestive heart failure, renal failure with need for dialysis, disseminated cancer, diabetes mellitus, preoperative sepsis (systemic inflammatory response syndrome, sepsis, or septic shock within 48 h prior to surgery), chronic obstructive pulmonary disease (COPD), ascites, and hypertension requiring medication. Other factors include American Society of Anesthesiologists (ASA) class score, mechanical bowel preparation, oral antibiotic bowel preparation, body mass index (BMI), preoperative serum albumin level, and preoperative white blood cell count (WBC). Operative factors analyzed included: surgical approach (open vs. minimally invasive approaches), operation time, and type of anastomosis performed. The primary endpoints investigated were the rate and predictors of paralytic ileus. Patients with paralytic ileus were identified. Risk-adjusted analysis was performed to identify the independent predictors of paralytic ileus.
Statistical analysis
The SPSS software statistical package version 22 (SPSS Inc., Chicago, IL) was utilized to perform statistical analysis. Multivariate statistical analysis using logistic regression was conducted to eliminate confounding variables and estimate the association between preoperative factors and paralytic ileus. The adjusted odds ratio (AOR) with a 95 % confidence interval was calculated, and P values <0.05 indicate statistical significance. Adjustment was made for all variables of the study. In order to report performance measures of the regression analysis model, Cox and Snell R Square of the regression analysis model is reported, which was 0.079.
Results
We identified a total of 27,560 patients who underwent partial colectomy. The median age was 63 years old, and the majority of the patients were Caucasian (86.7 %) and female (52.4 %). The most common comorbidities included hypertension (48.7 %) and diabetes mellitus (14.5 %). Demographics and other clinical variables of the patient population based on the types of colon resection are described in Table 1.
Among patients who underwent colon resection, 3497 (12.7 %) had prolonged ileus within 30 days of operation. Following multivariate adjustment analysis, patients with prolonged ileus had a significantly higher mortality risk (3.7 vs. 0.9 %, AOR 1.55, CI 1.11–2.13, P < 0.01).
Overall, 25.5 % of patients with unplanned readmission to hospitals had the complication of ileus. Following multivariate adjustment analysis, prolonged ileus following colon resection was significantly associated with unplanned readmission to hospitals (18.2 vs. 7.7 %, AOR 1.51, CI 1.30–1.76, P < 0.01). Also, patients with prolonged ileus were three times more likely to undergo unplanned reoperation compared to patients without prolonged ileus (AOR 3.20, CI 2.62–3.92, P < 0.01). The median length of stay after surgery was 9 days in patients with prolonged ileus, while patients without prolonged ileus remained hospitalized for 4 days after surgery (the adjusted mean difference was 5 days, CI 4.7–5.2, P < 0.01).
Table 2 describes the associations between perioperative variables and postoperative prolonged ileus. Cox and Snell R Square of the regression analysis model was 0.079. Among comorbid conditions, COPD and disseminated cancer were significantly associated with prolonged ileus. Among the type of anastomoses performed, ICA had a significantly higher risk of prolonged ileus compared to CRA. Factors such as oral antibiotic colon preparation and minimally invasive approaches to colectomy were associated with a decreased risk of prolonged ileus. Also, prolonged ileus was observed more frequently in patients with postoperative intra-abdominal infections and anastomosis leakage.
There is an association between patients’ age and postoperative prolonged ileus (Fig. 1). Patients older than 60 years had a significantly higher rate of prolonged ileus compared to patients younger than 50 years (14.1 vs. 10.9 %, AOR 1.31, CI 1.16–1.47, P < 0.01).
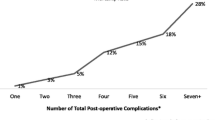
Figure 2 reports the associations between the operation length and postoperative prolonged ileus. With increasing operation time, the risk of prolonged ileus increased significantly (P < 0.01).
Discussion
Prolonged ileus is a common complication in colon surgery. However, ileus persisting for more than 1 week is associated with poor outcomes in colon surgery. Our study results show that patients with prolonged ileus lasting more than 1 week have a higher mortality rate, longer postoperative hospitalization, and higher risk of unplanned reoperation and readmission to hospitals. Also, in line with the literature, we found that patients with prolonged ileus have a significantly higher risk of postoperative complications such as intra-abdominal infections and anastomosis leakage, which emphasizes the need to consider such postoperative events in any patient with prolonged ileus after colon surgery [1, 2]. Although there are numerous preoperative and operative factors that can lead to postoperative ileus, in patients with ileus lasting for more than 1 week, it is crucial to rule out postoperative complications as the underlying causes of prolonged ileus.
This study reinforces the importance of prolonged ileus in colon surgery. We have found that 25.5 % of readmitted patients following colectomy had complication of ileus. In addition, prolonged ileus increases the risk of unplanned reoperation by more than three times. Previous studies have reported similar results [1, 2, 4]. Postoperative ileus usually resolves spontaneously in 2–3 days and reflects inhibition of colonic motility with alpha II adrenergic reflexes, release of hormones, neurotransmitters, and an inflammatory reaction. However, prolonged ileus frequently lasts more than 1 week and is a severe condition which may reflect an underlying severe postoperative complication [5, 9]. Intensive postoperative care, including a thorough workup with regard to the underlying cause of prolonged ileus, is strongly encouraged in patients with ileus lasting more than 1 week after operation.
This study introduces the predictors of prolonged ileus in colon surgery which can assist surgeons in identifying high-risk patients. To our knowledge, this is one of the first national studies to report the predictors of prolonged ileus in the USA. Our analyses show that advance age (Fig. 1), preoperative ASA score more than two, long operation length (Fig. 2), preoperative sepsis, disseminated cancer, and COPD significantly increase the risk of postoperative prolonged ileus. Factors of ASA score more than two, long operation time, and male gender have been previously reported as risk factors for prolonged ileus [3, 16]. In addition, we have found that laparoscopic surgery and oral antibiotic bowel preparation can significantly decrease the risk of postoperative prolonged ileus. Although the introduced predictors of prolonged ileus in this study are usually unavoidable, utilizing minimally invasive approaches in colon surgery may decrease postoperative ileus in such patients. A lower rate of postoperative ileus in laparoscopic surgery compared to open surgery has been noted in numerous studies [6, 14, 15]. The lower rate of postoperative ileus with laparoscopy is likely related to multiple factors such as the minimization of the stimulation of bowel inhibitory reflexes, intestinal manipulation and surgical trauma, decreased narcotic use, as well as early feeding and mobilization [6, 15]. However, the lower rate of postoperative ileus associated with laparoscopy may be related to a bias due to differences in patient selection of laparoscopic surgery and open surgery. Surprisingly, we found a lower rate of prolonged ileus in patients who received preoperative oral antibiotic bowel preparation, confirming previous reports [16]. However, further studies are needed to compare the benefits and adverse effects of oral antibiotic bowel preparation in colon surgery.
Our study results show that the rate of prolonged ileus is highest in colon resections with ICA. The rate decreases in colon resection with CCA, and the lowest rate of prolonged ileus in colon resection was observed with CRA. Following multivariate analysis, ICA was associated with a significantly higher rate of prolonged ileus compared to CRA. Other studies report a higher rate of prolonged ileus after small bowel resection compared to colorectal resection (19.9 vs. 14.9 %) [2]. The high rate of prolonged ileus in colonic resection with ICA in our study may be attributed to resection and anastomosis of small bowel with ICA in concert with the literature [2]. Another explanation is the manipulation around the duodenum which occurs with a right colectomy. However, there are limited published data in this topic and further clinical studies are indicated to confirm and explain these correlations.
Preoperative infection and inflammation have been associated with postoperative prolonged ileus. This study shows that there are significant associations between prolonged ileus and preoperative sepsis, septic shock, and SIRS in colon surgery. This reinforces the role of infection and local inflammatory response as important factors in the pathogeneses of prolonged ileus [6, 17]. Inflammation or manipulation of bowel with inhibitory alpha II adrenergic reflexes contributes to postoperative ileus [5]. However, trials of adrenergic blockade, cholinergic stimulation, and prokinetic drugs have met with limited success [5]. Recent studies reported an improvement in postoperative ileus with vasoactive intestinal peptide and substance P receptor antagonists [17–19]. However, there are limited data in this topic and further studies are needed. Also, investigation of postoperative complications as the underlying causes of prolonged ileus before symptomatic treatment is essential.
Patients who underwent colectomy for chronic constipation and Crohn’s disease have a significantly higher risk of prolonged ileus. We have found that preoperative chronic constipation increases the risk of prolonged ileus by more than three times. It may be related to the underlying pathology of patients with chronic constipation. Such patients may benefit from prokinetic drugs. Also, we have found a significant risk of prolonged ileus in patients with Crohn’s disease compared to colon cancer patients. High rates of prolonged ileus in patients with Crohn’s disease have been previously reported [7]. Nutritional support, correcting fluid, and electrolyte disorders in Crohn’s patients undergoing bowel resection may decrease postoperative ileus [7].
Study limitations
This study is a large retrospective review and, as with such studies, is limited in its ability to produce cause–effect relationships as well as control for all possible confounders. Data in this study were extracted from the discharge data, and coding errors could potentially have occurred [20]. The study’s data were collected from over 500 hospitals across the USA, and the wide variation in hospital setting, hospital quality, surgical strategy, and surgeons’ expertise may confound the study. NSQIP did not collect some important information such as opioid dosage administration, mobilization after surgery, use of prokinetic agents, insertion of nasogastric tube, previous abdominal surgery, and chronic preoperative use of narcotics which may impact risk of prolonged ileus [1, 6]. Also, patients who underwent total colectomy were excluded from the study due to the lack of a reliable CPT code for total colectomy without a stoma creation. Despite these limitations, this study provides a large sample size to report predictors of prolonged ileus in colon surgery and compare the risk of prolonged ileus by the types of colon resections.
Conclusions
Postoperative prolonged ileus is a common complication in colon surgery. However, ileus persisting for more than 1 week is associated with longer hospitalization, higher mortality, and higher risk of unplanned reoperation and readmission. In addition, there are significant associations between complications of anastomosis leakage and intra-abdominal infections and postoperative ileus lasting more than 1 week. Investigation of postoperative complications as the underlying causes of prolonged ileus before symptomatic treatment is essential. A number of preoperative factors have been associated with prolonged ileus. Preoperative infectious conditions, such as sepsis, septic shock, and SIRS, increase the risk of prolonged ileus. Comorbid conditions, such as ASA score more than two and disseminated cancer, increase the risk of prolonged ileus. However, laparoscopic surgery and preoperative oral antibiotic bowel preparation appear to decrease the risk of prolonged ileus. Among colonic resection/anastomosis, the highest risk of prolonged ileus is seen after colectomy with ICA. The risk of prolonged ileus decreases after colectomy with CCA and the lowest risk of prolonged ileus exists in colectomy with CRA. Also, patients with chronic constipation who underwent bowel resection have a significantly higher risk of postoperative prolonged ileus.
References
Kronberg U, Kiran RP, Soliman MS, Hammel JP, Galway U, Coffey JC et al (2011) A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg 253:78–81
Iyer S, Saunders WB, Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15:485–494
Millan M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E (2012) Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg 36:179–185
Delaney C, Kehlet H, Senagore AJ, Bauer AJ, Beart R, Billingham R et al (2006) (eds) Clinical consensus update in general surgery [Internet] Roswell: pharmatecture, LLC; [cited 2015 Feb 1]. http://www.clinicalwebcasts.com/pdfs/GenSurg_WEB.pdf
Livingston EH, Passaro EP (1990) Postoperative ileus. Dig Dis Sci 35:121–132
Holte K, Kehlet H (2000) Postoperative ileus: a preventable event. Br J Surg 87:1480–1493
Forbes A (2014) Crohn’s disease: rehabilitation after resection. Dig Dis 32:395–398
Bueno L, Fioramonti J, Delvaux M, Frexinos J (1997) Mediators and pharmacology of visceral sensitivity: from basic to clinical investigations. Gastroenterology 112:1714–1743
Luckey A, Livingston E, Taché Y (2003) Mechanisms and treatment of postoperative ileus. Arch Surg 138:206–214
Köninger J, Gutt CN, Wente MN, Friess H, Martin E, Büchler MW (2006) Postoperative ileus. Pathophysiology and prevention. Chirurg 77:904–912
Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C et al (2008) Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg 32:1495–1500
Shibata Y, Toyoda S, Nimura Y, Miyati M (1997) Patterns of intestinal motility recovery during the early stage following abdominal surgery: clinical and manometric study. World J Surg 21:806–809 (discussion 809–810)
National Surgical Quality Improvement Program (2005) [home page on the Internet] Chicago, IL: American College of Surgeons. [cited 2015 Jan 17]. www.acsnsqip.org
Böhm B, Milsom JW, Fazio VW (1995) Postoperative intestinal motility following conventional and laparoscopic intestinal surgery. Arch Surg 130:415–419
Holte K, Kehlet H (2002) Prevention of postoperative ileus. Minerva Anestesiol 68:152–156
Polacek MA, Close AS (1963) The effect of antibiotic bowel preparation and peritoneal irrigation on the duration of post-operative ileus. Am J Surg 105:768–770
Kalff JC, Carlos TM, Schraut WH, Billiar TR, Simmons RL, Bauer AJ (1999) Surgically induced leukocytic infiltrates within the rat intestinal muscularis mediate postoperative ileus. Gastroenterology 117:378–387
Espat NJ, Cheng G, Kelley MC, Vogel SB, Sninsky CA, Hocking MP (1995) Vasoactive intestinal peptide and substance P receptor antagonists improve postoperative ileus. J Surg Res 58:719–723
De Winter BY, Robberecht P, Boeckxstaens GE, De Man JG, Moreels TG, Herman AG et al (1998) Role of VIP1/PACAP receptors in postoperative ileus in rats. Br J Pharmacol 124:1181–1186
Lorence DP, Ibrahim IA (2003) Benchmarking variation in coding accuracy across the United States. J Health Care Finance 29:29–42
Disclosures
Dr. Stamos has received educational grants and speaker fees paid to the Department of Surgery, University of California, Irvine, from Ethicon, Gore, Covidien, and Olympus. Dr. Mills and Dr. Carmichael received Ethicon educational grants paid to the Department of Surgery, University of California, Irvine. Dr. Pigazzi is a consultant for Intuitive Surgical and has also received consultancy fees and educational grants paid to the Department of Surgery, University of California, Irvine. Dr. Moghadamyeghaneh, Dr. Phelan, Dr. Hwang, and Dr. Hanna have no disclosures. Dr. Moghadamyeghaneh had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moghadamyeghaneh, Z., Hwang, G.S., Hanna, M.H. et al. Risk factors for prolonged ileus following colon surgery. Surg Endosc 30, 603–609 (2016). https://doi.org/10.1007/s00464-015-4247-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4247-1