Abstract
Background
Acute appendicitis is the second most common gastrointestinal diagnosis mandating urgent operation in the U.S. The current state of adult appendectomy, including patient and hospital characteristics, complications, and predictors for complications, are unknown.
Methods
Retrospective review of U.S. Nationwide Inpatient Sample 2003–2011 for appendectomy in ≥18-year-olds was performed. Primary outcomes measures included postoperative complications, length of stay, and patient mortality. Categorical variables were analyzed by χ2, trend analyses by Cochran–Armitage. Multivariable logistic regression was performed to adjust for predictors of developing complications.
Results
1,663,238 weighted appendectomy discharges occurred. Over the study period, complications increased from 3.2 to 3.8 % (p < 0.0001), but the overall mortality decreased from 0.14 to 0.09 % (p < 0.0001) and mean LOS decreased from 3.1 to 2.6 days (p < 0.0001). The proportion of laparoscopic appendectomy increased over time, 41.7–80.1 % (p < 0.0001). Patients were increasingly older (≥65 years: 9.4–11.6 %, p < 0.0001), more obese (3.8–8.9 %, p < 0.0001), and with more comorbidities (Elixhauser score ≥3: 4.7–9.8 %, p < 0.0001). After adjustment, independent predictors for postoperative complications included: open surgery (OR 1.5, 95 % C.I. 1.4–1.5), male sex (OR 1.6, 95 % CI 1.5–1.6), black race (vs. white: OR 1.5, 95 % CI 1.4–1.6), perforated appendix (OR 2.8, 95 % CI 2.7–3.0), greater comorbidity (Elixhauser ≥3 vs. 0, OR 11.3, 95 % CI 10.5–12.1), non-private insurance status (vs. private: Medicaid OR 1.3, 95 % CI 1.2–1.4; Medicare OR 1.7, 95 % CI 1.6–1.8), increasing age (>52 years vs. ≤27: OR 1.3; 95 % CI 1.2–1.4), and hospital volume (vs. high: low OR 1.2; 95 % CI 1.1–1.3). Predictors of laparoscopic appendectomy were age, ethnicity, insurance status, comorbidities, and hospital location.
Conclusions
Laparoscopic appendectomy is increasing but is unevenly deployed across patient groups. Appendectomy patients were increasingly older, with more comorbidities and with increasing rates of obesity. Black patients and patients with public insurance had less utilization of laparoscopy and inferior outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute appendicitis is the second most common gastrointestinal diagnosis mandating urgent operation in the United States [1]. Surgical removal of the appendix has long been the gold standard of treatment because of its efficacy and low mortality [2]. Research has suggested superiority of laparoscopic appendectomy for reduced complication rate, length of stay (LOS), and reduced cost [3, 4]. However, current nationwide rates of use of laparoscopic appendectomy and postoperative complications are unknown.
The aims of this study were to use a large, population-based database to describe trends in appendectomy for acute appendicitis, estimate the incidence of postoperative complications, and to identify predictors of these complications.
Materials and methods
This was a retrospective review of the U.S. Nationwide Inpatient Sample (NIS) for the years 2003–2011. NIS is the largest, all-payer hospital inpatient database in the United States [5]. It is supported by the Healthcare Cost and Utilization Project (HCUP). It is an administrative database, which contains both clinical and non-clinical information for nearly 8 million discharges per year, from a stratified sample of 20 % of non-federal hospitals. Data can be weighted to give nationwide estimates. To facilitate this, NIS publishes annual weighting elements which are independently validated to ensure accuracy [6]. All data presented are weighted frequencies, and analyses were performed on weighted data.
Study population
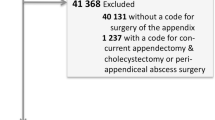
Open and laparoscopic appendectomies were identified using ICD-9 codes: 47.01 or 47.09. Only those with a concurrent diagnosis of acute appendicitis (ICD-9 codes 540.0, 540.1, 540.9) and those aged 18 years or older were included. Perforated appendix was determined by the ICD-9 codes 540.0 (with peritonitis) and 540.1 (peritoneal abscess). Conversion from laparoscopy to open appendectomy was identified using ICD-9 codes V64.4 and V64.41.
Data
Hospital surgical volume was calculated as low (1–82/year), medium (82–181/year), and high (>181/year) based on tertiles from the dataset. Age groups were divided by quartiles into 18–27, 28–38, 39–52, and >52 years. Elective procedures were excluded to focus on management of acute appendicitis. Complications were defined as those recorded within the same admission as the appendectomy. Complications were calculated by querying the dataset for secondary diagnostic or procedural ICD-9 codes. The complications captured were postoperative infection, aspiration pneumonia or respiratory failure, genitourinary complication including acute renal failure, myocardial infarction, venous thromboembolic events including deep venous thrombus and pulmonary embolus, gastrointestinal hemorrhage, perforation or ulceration, and wound disruption. They were queried for within the database using ICD-9 codes from a previously validated and published system [7]. HCUP Comorbidity Software version 3.7 was used to determine Elixhauser comorbidity scores [8]. Elixhauser comorbidity scale is an algorithm to classify a comprehensive set of comorbidities, specifically designed for use with large datasets such as the NIS [9].
Statistical analysis
All data were analyzed using SAS version 9.3 (SAS Institute, Cary, NC). Univariate analysis of categorical variables was performed using χ2 tests. Trend analyses were performed using Cochran–Armitage. Multivariable logistic regression was performed with complications as the dependent variable. Independent variables were chosen through a method of manually adding significant covariates from univariate analysis in order of decreasing significance, and assessing changes in the estimate and p value. This yielded a conservative estimate which gave priority to confounding over collinearity. All p values are two-sided. A p value of less than 0.05 was considered significant. Odds ratios and confidence intervals excluding 1 were considered significant.
Annual incidence was calculated per 100,000 persons using annual estimated population data published by the United States Census bureau [10]. This method has been previously published [11].
Results
Overall, 1,734,023 non-elective inpatient admissions for acute appendicitis and 1,663,238 appendectomies were performed during the study period. 95.92 % of acute appendicitis inpatient admissions involved appendectomy, and the annual incidence of appendectomy for acute appendicitis was 61.8/100,000 persons. Crude mortality rate for appendectomies was 0.1 % (n = 2,282) and crude complication rate was 3.5 % (n = 57,945).
Trends over time
The volume of appendectomy performed over the study period remained stable. However, the proportion of laparoscopic appendectomy increased over time, from 41.7 to 80.1 % (p < 0.0001) (Fig. 1). The rates of conversion to open increased from 0.13 to 0.17 % of total laparoscopic appendectomy (p < 0.0001). The rate of complications increased from 3.2 to 3.8 % (p < 0.0001). In contrast, the overall mortality decreased from 0.14 to 0.09 % (p < 0.0001) and the mean LOS also decreased from 3.1 to 2.6 days (p < 0.0001).
Demographic characteristics of patients changed over the study period. Patients were increasingly older (≥65 years: 9.4–11.6 %, p < 0.0001), more obese (3.8–8.9 %, p < 0.0001), and with more comorbidities (Elixhauser score ≥3: 4.7–9.8 %, p < 0.0001).
Predictors of complications
Table 1 shows unadjusted demographic characteristics of those who had postoperative complications compared with those who did not. Those with postoperative complications were more likely to be male, older, with more comorbidities, have had their appendectomy at a non-teaching hospital, in a rural location, and had open surgery or conversion to open surgery. They were also less likely to identify as white race and less likely to have private health insurance.
Table 2 reports the unadjusted and adjusted odds ratios of complications. After adjustment, independent predictors for postoperative complications included male sex, black race, surgical modality, greater comorbidity, non-private insurance status, increasing age, surgery at hospital with low surgical volume, and open surgery.
Predictors of laparoscopy
Figure 2 shows adjusted predictors of laparoscopic appendectomy. After adjustment, those receiving laparoscopy were more likely to be younger (18–27 years), identify as being of white race, have private or other/missing insurance status, have no comorbidities, and have had their surgery at an urban hospital.
Discussion
In this paper, we have performed a nationwide analysis of appendectomy as deployed in the early 21st century. The complication rate in this series, while small, increased significantly through the study period. Several factors may contribute to this apparent increase. Patients were increasingly older and more obese, with more comorbidities. Although the overall rate of laparoscopy increased over time with lower complications rates, there were disparities in access to laparoscopic appendectomy by ethnicity, insurance status, and surgical volume of the hospital.
Older patients and those with higher Elixhauser comorbidity scores were less likely to receive laparoscopy. A study examining disparities in access to laparoscopic appendectomy and laparoscopic cholecystectomy at the University of California health care consortium showed that Medicare patients were significantly less likely to receive either of these minimally invasive procedures [12]. Clinician reluctance to perform laparoscopy on older patients should be dissuaded, as numerous studies have now demonstrated the efficacy and safety of laparoscopic appendectomy in older adults [13, 14]. With an aging population, this issue will become increasingly significant.
Black race and public insurance status were associated with higher postoperative complication rates and lower likelihood of laparoscopic treatment. Racial disparities in access to laparoscopy have been noted in several smaller studies [13, 15]. In this series, black race was associated with higher postoperative complications, even after adjusting for surgical approach and appendiceal perforation. Further studies are needed in order to identify the cause of and address these apparent inequalities.
Having surgery at a hospital with low surgical volume was associated with lower likelihood of having laparoscopic surgery and with higher complications rate. The benefits of having surgery at high-volume centers have been well-established, supporting regionalization [16]. Having appendectomy performed by a surgeon experienced with minimally invasive surgery has been shown to be associated with fewer postoperative intra-abdominal collections [3]. Although appendectomy is a relatively common procedure, laparoscopic appendectomy can be complex and multifaceted [17]. An early study of surgeon learning curve advocated for performance of over 120 laparoscopic appendectomies in order to become proficient [18]. The number and type of appendectomies required in the more recent era of training remains unknown.
This study has several limitations. The NIS is a database primarily kept for administrative purposes and lacks clinical granularity, such as the severity of complications or reasons why an individual patient received laparoscopy over open surgery. We were unable to look at pathology reports from patients, although the strict inclusion criteria mandated only non-elective procedures for acute appendicitis. Patients with acute appendicitis who required more extensive resection, including but not limited to cecectomy or partial colectomy, may not have been captured in this inclusion criteria, unless the appendectomy portion of the procedure was coded separately.
Further, data entry and code selection are subject to both errors and biases the retrospective, and observational nature of this review prevents us from determining causal relationships, only correlations. As the NIS is a discharge database, we were unable to trace these patients to outcomes beyond their hospital admission and patients may have been readmitted with complications.
This study used nationwide data to describe postoperative complication rates for appendectomy and predictors for these complications. We found an increasingly older, more obese, and sicker population of patients with growing postoperative complication rates. Disparities in access to laparoscopic treatment and a gap in postoperative complications by race and insurance type were identified. Future studies must identify and address reasons behind these disparities in order to minimize these inequalities and reduce overall complications.
References
Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, Stamos MJ (2011) Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006-2008. J Gastrointest Surg 15:2226–2231
Hilli ZA, Prichard RS, Roche-Nagle G, Leader M, McNamara DA, Deasy J (2009) Emergency appendicectomy in the era of laparoscopy: a one-year audit. Ir J Med Sci 178:473–477
Wilson DG, Bond AK, Ladwa N, Sajid MS, Baig MK, Sains P (2013) Intra-abdominal collections following laparoscopic versus open appendicectomy: an experience of 516 consecutive cases at a district general hospital. Surg Endosc 27:2351–2356
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 6:CD001546. doi:10.1002/14651858
HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2007-2009. Agency for Healthcare Research and Quality, Rockville. www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 17 April 2014
Houchens RL, Elixhauser A. (2006) Using the HCUP Nationwide Inpatient Sample to Estimate Trends. (Updated for 1988–2004). HCUP Methods Series Report #2006-05 Online. U.S. Agency for Healthcare Research and Quality
Lawthers AG, McCarthy EP, Davis RB, Peterson LE, Palmer RH, Iezzoni LI (2000) Identification of in-hospital complications from claims data. Is it valid? Med Care 38:785–795
HCUP Comorbidity Software. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed 17 April 2014
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27
American Census Bureau. (2014) Fact Finder. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed on 17 April 2014
Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, Jacobs E, Nanchal R (2011) Nationwide trends of severe sepsis in the 21st century (2000–2007). Chest 140:1223–1231
Varela JE, Nguyen NT (2011) Disparities in access to basic laparoscopic surgery at U.S. academic medical centers. Surg Endosc 25:1209–1214
Moazzez A, Mason RJ, Katkhouda N (2013) Thirty-day outcomes of laparoscopic versus open appendectomy in elderly using ACS/NSQIP database. Surg Endosc 27:1061–1071
Southgate E, Vousden N, Karthikesalingam A, Markar SR, Black S, Zaidi A (2012) Laparoscopic vs open appendectomy in older patients. Arch Surg 147:557–562
Scarborough JE, Bennett KM, Pappas TN (2012) Racial disparities in outcomes after appendectomy for acute appendicitis. Am J Surg 204:11–17
Bliss LA, Yang CJ, Chau Z, Ng SC, McFadden DW, Kent TS, Moser AJ, Callery MP, Tseng JF (2014) Patient selection and the volume effect in pancreatic surgery: unequal benefits? HPB 16:899–906. doi:10.1111/hpb.12283
Ferranti F, Corona F, Siani LM, Stefanuto A, Aguzzi D, Santoro E (2012) Laparoscopic versus open appendectomy for the treatment of complicated appendicitis. G Chir 33:263–267
Alvarez C, Voitk AJ (2000) The road to ambulatory laparoscopic management of perforated appendicitis. Am J Surg 179:63–66
Disclosure
Drs. Bliss, Yang, Kent, Critchlow and Tseng and Ms. Ng have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bliss, L.A., Yang, C.J., Kent, T.S. et al. Appendicitis in the modern era: universal problem and variable treatment. Surg Endosc 29, 1897–1902 (2015). https://doi.org/10.1007/s00464-014-3882-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3882-2