Abstract
Background
The detection of gastroesophageal reflux (GERD) via pH testing is the key component of the evaluation of patients considered for antireflux surgery. Two common pH testing systems exist, a multichannel, intraluminal impedance-pH monitoring (MII-pH) catheter, and wireless (Bravo®) capsule; however, discrepancies between the two systems exist. In patients with atypical symptoms, MII-pH catheter is often used preferentially. We aimed to elucidate the magnitude of this discrepancy and to assess the diagnostic value of MII-pH and the Bravo wireless capsule in a population of patients with mixed respiratory and typical symptoms.
Methods
The study population consisted of 66 patients tested with MII-pH and Bravo pH testing within 90 days between July 2009 and 2013. All patients presented with laryngo-pharyngo-respiratory (LPR) symptoms. Patient demographics, symptomatology, manometric and endoscopic findings, and pH monitoring parameters were analyzed. Patients were divided into four comparison groups: both pH tests positive, MII-pH negative/Bravo positive, MII-pH positive/Bravo negative, and both pH tests negative.
Results
Nearly half of the patients (44 %) had discordant pH test results. Of these, 90 % (26/29) had a negative MII-pH but positive Bravo study. In this group, the difference in the DeMeester score was large, a median of 29.3. These patients had a higher BMI (28.5 vs. 26.1, p = 0.0357), were more likely to complain of heartburn (50 vs. 23 %, p = 0.0110), to have a hiatal hernia, (85 vs. 53 %, p = 0.0075) and a structurally defective lower esophageal sphincter (LES, 85 vs. 58 %, p = 0.0208).
Conclusions
In patients with LPR symptoms, we found a high prevalence of discordant esophageal pH results, most commonly a negative MII-pH catheter and positive Bravo. As these patients exhibited characteristics consistent with GERD (heartburn, defective LES, hiatal hernia), the Bravo results are likely true. A 24-h MII-pH catheter study may be inadequate to diagnose GERD in this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ambulatory esophageal pH monitoring plays a critical role in the diagnosis of gastroesophageal reflux disease (GERD) [1]. It is a key component of the preoperative evaluation and should be performed in all patients who are considered for antireflux surgery, as a positive pH test is predictive of an excellent outcome [2]. Currently, a trans-nasal, multichannel, intraluminal impedance-pH monitoring catheter (MII-pH) or wireless (Bravo®) capsule is utilized depending on local availability and physician preference. However, the diagnostic accuracy and reproducibility of each method and between the two methods are far from ideal [3–8].
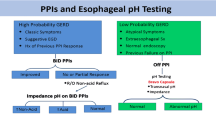
With the added ability to measure bolus transit, reflux height, non-acid reflux events, and proximal esophageal acid exposure, a dual probe, 24-hour multichannel MII-pH monitoring catheter has been preferentially used to evaluate patients with atypical GERD symptoms such as laryngo-pharyngo-respiratory (LPR) symptoms. However, controversies exist regarding the accuracy of proximal esophageal acid exposure detection [9, 10].
It can be challenging to determine whether gastroesophageal reflux is the cause of a patient’s extra-esophageal symptoms such as cough, hoarseness, or sore throat. Accurate detection of distal esophageal acid exposure is essential; however, clinically observed discrepancies between MII-pH and Bravo pH monitoring systems make obtaining a clear causal relationship difficult. With the focus on distal esophageal acid exposure detection, we aimed to elucidate the magnitude of this discrepancy and to assess the diagnostic value of MII-pH versus the Bravo capsule in a population of patients with mixed respiratory and typical gastrointestinal symptoms of GERD.
Materials and methods
Data collection
A prospectively collected database of esophageal function tests of patients seen at our esophageal diagnostic laboratory was utilized for data collection. Patients who underwent both MII-pH and Bravo pH monitoring tests between July 2009 and 2013 were identified, excluding patients with achalasia, other known esophageal motility disorders, previous antireflux operations, or gastric bypass surgery. Patient demographics, presenting symptoms, endoscopic findings, manometric data, and pH monitoring parameters were collected and analyzed. Typical reflux symptoms were defined as heartburn, regurgitation, dysphagia, chest pain, and epigastric pain. The atypical, LPR symptoms included globus sensation, cough, hoarseness, increased phlegm, sour taste, throat burning, throat clearing, throat pain or soreness, shortness of breath, excessive mucus production, and choking. All patients were queried by the clinician about their primary and secondary most troublesome symptoms driving clinical evaluation and were interviewed for the presence of other typical or atypical symptoms.
pH monitoring
All MII-pH catheters were placed trans-nasally at 5 cm above the upper border of the manometrically determined lower esophageal sphincter (LES). All Bravo capsules were placed endoscopically 6 cm above the gastroesophageal junction (GEJ) under moderate conscious sedation. Both pH studies were performed within 90 days of each other. All pH studies were done off proton pump inhibitors (PPI) for at least 7 days. A positive study was defined by a DeMeester score >14.7 for MII-pH studies. A DeMeester score >17.95 during the first 24-h of monitoring (day 1), a DeMeester score >15.76 during the second 24-h (day 1), or a DeMeester score >14.98 for days 1 and 2 combined was used to define a positive Bravo study according to the published normal reference values for the 48-h Bravo pH monitoring system [11]. MII-pH impedance results were collected and analyzed.
Patients were divided into four groups according to MII-pH and Bravo results for comparison: both positive pH tests (Cath+Bravo+), MII-pH negative but Bravo positive (Cath−Bravo+), MII-pH positive but Bravo negative (Cath+Bravo−), and both negative (Cath−Bravo−) groups.
The presence of a hiatal hernia was defined as a greater than 2 cm axial separation between the LES and the crura of the diaphragm either manometrically or endoscopically. A manometrically determined structurally defective LES was defined as a short overall length (<24 mm), a short intra-abdominal length (<9 mm), or a below normal resting pressure (<9.8 mmHg).
Equipment
All esophageal diagnostic testing was performed using ComfortTec® Z/pH Probe (single-use) catheter (ZAI-BD-31, Sandhill Scientific, Highlands Ranch, CO), Bravo®pH capsule (Given Imaging, Yokneam, Israel), and the ManoScan ESO Z Catheter system (Given Imaging, Yokneam, Israel). Catheter data were analyzed using the Sandhill ZepHr® Software (Sandhill Scientific, Highlands Ranch, CO). Capsule-based study results were automatically generated by the Bravo®pH Monitoring software (Given Imaging, Yokneam, Israel). Manometric data were analyzed using the ManoView Analysis software (Sierra Scientific Instruments, version 3.0, Los Angeles, CA, USA).
Statistical analysis
All data are expressed as medians unless specifically noted. Non-parametric test, Wilcoxon signed-rank or Kruskal–Wallis, was used for data analysis. χ 2 test and t test were used for categorical and continuous data, respectively. The data analysis was performed using SAS software, Version 9.3 of the SAS System for Windows (SAS Institute Inc., Cary, NC). A p value less than 0.05 was considered statistically significant. This study was performed with approval by the Research Subjects Review Board at the University of Rochester.
Results
Patient population
The study population consisted of 66 patients with a mean age of 52 (SD = 13) and mean BMI of 26 (SD = 5). The study population was 32 % male. All patients complained of at least one LPR symptom. Focusing on just the primary and secondary presenting complaints driving clinical evaluation, 58 % (38/66) presented with a mixed picture of a typical and a LPR symptom, 30 % (20/66) with primary and secondary LPR symptoms, and 12 % (8/66) had typical symptoms as their major primary and secondary complaint (Fig. 1).
Discordance between MII-pH and Bravo
Of the 66 patients, 9 patients had both positive catheter and Bravo pH monitoring, 26 patients had a negative catheter but positive Bravo study, 3 patients had a positive catheter but negative Bravo study, and 28 patients had both tests negative (Fig. 2). The median time interval between the two tests of our study population was one day (IQR = 2). The mean difference in MII-pH probe tip and Bravo capsule placement location, reflecting the distance from nostril to larynx, was 4.8 cm (standard deviation, SD = 1.3), 3.9 cm (SD = 2.3), 3.0 cm (SD = 2.2), and 3.4 cm (SD = 1.6) for each group, respectively. No statistical differences were found probe and capsule location between groups (p = 0.1671). The median DeMeester scores of the catheter and Bravo methods for each group are plotted in Fig. 3. Comparing the differences in DeMeester scores between the two methods showed the Cath−Bravo+ group had a difference that was statistically significant (Table 1). In the Cath−Bravo+ group, the difference in the overall score was large with a median of 29.3, suggesting that the results were truly discordant (Table 1; Fig. 4). The three patients who had a positive catheter pH monitoring but negative Bravo had comparable DeMeester scores to patients in which both tests were negative (Table 1). Overall, we found nearly half of the patients (44 %, 29/66) had discordant test results. Of these, 90 % (26/29) had a negative catheter but positive Bravo study.
When comparing the Cath−Bravo+ group with all other subjects, there were no significant differences in age, gender, smoking status, duration of GERD symptoms, or duration of PPI use. Cath−Bravo+ patients had a higher BMI (28.5 vs. 26.1, p = 0.0357, Table 2). Significant differences in all pH parameters between the two methods were found in the Cath−Bravo+ group regardless whether the patient had a single day or both days positive Bravo test (Table 3). 54 % (14/26) of patients’ Bravo tests were positive on both days, 35 % (9/26) were positive on day one, and 12 % (3/26) were positive solely on day two.
pH parameters of proximal probe between groups
The pH testing results from the proximal probe are summarized for all groups and then compared between Cath−Bravo+ group with all others in Table 4. The Cath−Bravo+ group had significantly lower proximal esophageal acid exposure among all four groups. When comparing the proximal esophageal acid exposure between the Cath−Bravo+ group with all others, the Cath−Bravo+ group had significantly lower exposure in all available pH parameters except in the percent time pH < 4 in the supine position (% supine pH < 4). Interestingly, in all groups, the median values for proximal pH parameters were below our threshold for a positive proximal pH examination.
MII-pH impedance findings of proximal and distal probes between groups
Table 5 illustrates the number of patients with positive impedance findings for each group. There were no statistical differences between the Cath−Bravo+ group with all others when comparing the number of patients with increased bolus exposure or non-acid reflux detected by the distal probe. Interestingly, the Cath−Bravo+ group had less patients (6/26, 23 %) with increased bolus exposure or non-acid reflux detected by the proximal probe compared to all others (11/40, 27.5 %, p = 0.0422).
Presenting symptoms and lower esophageal anatomy/integrity
The distribution of primary and secondary symptoms of all patients is shown in Fig. 5A. LPR symptoms were predominant in our patient population as their primary or secondary presenting symptoms. Heartburn and regurgitation were the primary or secondary presenting symptoms in 19.6 and 15.2 % of patients, respectively (Fig. 5A, B). The symptom of “heartburn” was more commonly reported as the primary or secondary presenting symptoms in the Cath−Bravo+ group (50 vs. 23 %, p = 0.0110), indicating that majority of the patients in the Cath−Bravo+ group has mixed typical and LPR symptoms (Figs. 5b, 6). Patients in the Cath−Bravo+ group were found more often to have a hiatal hernia (85 vs. 53 %, p = 0.0075) as well as a structurally defective LES (85 vs. 58 %, p = 0.0208, Table 6).
Discussion
Patients with extra-esophageal manifestations of GERD are a challenging group to diagnose and manage. The gold standard diagnostic test remains esophageal pH monitoring to establish the presence of increased esophageal acid exposure. A dual channel pH catheter-based system has traditionally been the test of choice as it can identify patients with increased distal esophageal acid exposure and also quantifies proximal esophageal reflux events that may suggest causality between GERD and LPR symptoms. Other tests are used with variable efficacy, including pharyngeal pH monitoring (Restech), salivary pepsin measurement, and simultaneous pH/O2 monitoring, as useful adjuncts in the workup of patients with atypical GERD symptoms but have not supplanted esophageal pH monitoring [12].
Wireless capsule pH monitoring with the Bravo system is being performed with increasing frequency in the preoperative evaluation of patients with GERD. Improved patient comfort from lack of an intra-nasal catheter and the ability to monitor esophageal pH beyond 24 h increases the diagnostic yield to identify patients with GERD over a catheter pH system [1, 13, 14]. Discordant results between the Bravo and catheter pH tests have been reported and the Bravo results will often vary day-to-day [5, 15]. Some centers are investigating the utility of extending the monitoring period to 96 h [14, 16]. The utility of the Bravo probe in patients with LPR symptoms, however, remains unclear.
Previous studies have suggested a discrepancy in the reproducibility of each pH testing modality and between the two methods. On repeated 24 h pH tests, 24–32 % of patients have a discrepancy in acid exposure [3, 4]. A similar degree of discrepancy has been reported between the first and second 24-h monitoring period with the wireless-based method [5]. Studies, conducting simultaneous catheter-based and Bravo pH monitoring, have shown a higher acid exposure measured by the catheter system compared to the Bravo system, and the causes are largely unclear [6, 7]. The reported concordance rate from these simultaneous studies between the two methods was 80–88 %, leading to the conclusion that the two systems might not be interchangeable in practice [8, 17].
In a select patient population undergoing evaluation for GERD with atypical symptoms, we found that nearly half (44 %) of all patients had discordant results between the catheter and wireless pH monitoring systems. Analysis of those patients with a positive Bravo study yet negative catheter pH study demonstrated an increased frequency of typical GERD symptoms including heartburn, a higher likelihood of having a hiatal hernia on endoscopy or manometry, and a greater prevalence of a mechanically defective LES on manometry. These features are common in patients with GERD suggesting the Bravo results rather than the MII-pH catheter results represent the true positive and establish the diagnosis of GERD. In our study, 1/3 of patients may not have been considered for antireflux surgery based on the negative catheter pH result alone. As most patients in this study had a negative proximal pH acid exposure and a negative bolus or non-acid reflux exposure, it would seem the added benefit to detect proximal reflux events in the MII-pH impedance catheter was outweighed by the decreased diagnostic sensitivity to detect GERD [9]. Interestingly, patients with discordant pH results between the two methods had less bolus exposure detected by the MII-pH proximal probe, arguing against the diagnostic usefulness of impedance for the evaluation of LPR.
Dual probe 24-h catheter pH monitoring has been preferentially used to evaluate patients with atypical reflux symptoms; however, the sensitivity of proximal pH recording was only 55 % in a previous study [10]. While the distal probe is placed 5 cm above the upper border of the manometrically determined LES, the proximal probe is located 15 cm above the distal probe which was misplaced in 45 % of 661 patients according to McCollough et al. in their prospective study [9]. Besides the unreliable probe placement, other factors such as artifacts from saliva and swallowed air also make the results obtained from the proximal probe potentially less reliable. pH drift secondary to probe drying can significantly affect the diagnostic accuracy of proximal pH monitoring [1]. Criteria have been formulated to optimize its accuracy but further investigation and validation are still needed for proximal pH monitoring to be utilized clinically [18]. In general, the routine use of proximal pH monitoring is not recommended by the 2007 American College of Gastroenterology practice guidelines for esophageal reflux testing [1]. The presence of almost uniformly low proximal esophageal acid exposure in all groups in our study population likely was secondary to the limitations mentioned above. In our patient population with mixed LPR and typical reflux symptoms, the proximal pH recordings did not provide useful discriminatory data.
Controversy exists when it comes to the placement location of trans-nasal pH catheter tip and wireless capsule. Conventionally, distal esophageal acid exposure is detected by the catheter tip placed at 5 cm above the upper border of the LES or the Bravo capsule located at 6 cm above the GEJ. Both the catheter and capsule position have been areas of investigation. Pandolfino and Kahrilas et al. compared wireless and catheter-based systems, measuring the tip and the capsule position via fluoroscopy immediately after placement. The mean absolute difference in position between the two systems was 1.0 cm. The two placement methods resulted in similar tip and capsule positions. More importantly, they showed the difference in acid exposure between the two systems was not due to electrode position [6]. In our patient population, we did not find statistically significant differences in the locations of the catheter tip and Bravo between patients with concordant and discordant pH findings although fluoroscopic confirmation was not performed for this study.
Day-to-day variation in reflux is a known phenomenon and it adds complexity to the evaluation of GERD. Methods, such as prolonged monitoring time, have been proposed to overcome this issue in order to increase the diagnostic accuracy of pH monitoring. Previous studies have shown that prolonged pH monitoring to 48 h or even 96 h increases the diagnostic sensitivity compared to only 24-h of recording [11, 14–16, 19]. However, the reported 10 % improvement in sensitivity would not completely explain the 44 % discrepancy we observed in our patient population. Day-to-day variation was evaluated in our patient population. Our data showed that only half (14/26, 54 %) of the patients with discordant pH results between the two systems were positive on both days of Bravo monitoring. Only 35 % (9/26) were positive on day one, and 12 % (3/26) were positive only on day two. Bravo results from each day were compared individually with previously published normal reference values for the Bravo system, which would explain at least partially for some of the effects that day-to-day variation has on our analysis.
Unfortunately, a positive pH test does not necessarily indicate causality of extra-esophageal symptoms. While the efficacy of antireflux surgery in patients with typical symptoms of heartburn and regurgitation is excellent, the results for LPR symptom control after antireflux surgery are less successful [20, 21]. Multiple case series report control of LPR symptoms ranging from 50 to 70 % after antireflux surgery [20–23]. This significant difference in symptom control after antireflux surgery reflects the limitations of our diagnostic testing modalities as we are able to identify patients with GERD but not necessarily demonstrate causality of atypical symptoms. In this observational study, 44 % (4/9) of patients who had both positive catheter and Bravo pH monitoring underwent antireflux surgery, and all reported complete resolution of their atypical symptoms. 54 % (14/26) of patients who had a negative catheter but positive Bravo study underwent antireflux surgery with 71 % (10/14) of them reporting complete resolution of LPR symptoms, while three patients reported moderate improvement and one patient did not follow-up. One out of three patients who had a positive catheter but negative Bravo study underwent surgery with complete resolution of LPR symptoms. The median follow-up time for this population was short, only 24 days (IQR = 34). Overall, only 19 patients in the entire cohort underwent Nissen fundoplication. 14 of these 19 patients were catheter negative and Bravo positive. Of those patients with a catheter negative/Bravo positive, 10/14 (71 %) had complete resolution of LPR symptoms. These 10 patients would likely have not been considered for antireflux surgery if only a catheter-based pH study was performed. However, given the small sample size, short follow-up and our single institute experience, no conclusion could be made regarding whether Bravo pH monitoring better predicts symptomatic improvement of LPR after antireflux surgery.
Conclusion
In summary, we found high frequency of discordance between 24-h trans-nasal pH catheter and 48-h Bravo esophageal pH testing in patients with mixed atypical and typical symptoms. Patients with a pH positive Bravo and negative catheter study were more likely to have clinical findings consistent with the presence of GERD including typical symptoms, a hiatal hernia and a structurally defective LES suggesting false negative catheter studies. A single 24-h catheter study may not be an adequate test to evaluate gastroesophageal reflux in patients with atypical reflux symptoms. A prolonged period of monitoring as offered by the Bravo wireless system may be a better initial test of choice.
References
Hirano I, Richter JE (2007) ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol 102(3):668–685
Campos GM et al (1999) Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 3(3):292–300
Franzen T, Grahn LT (2002) Reliability of 24-hour oesophageal pH monitoring under standardized conditions. Scand J Gastroenterol 37(1):6–8
Weber C, Davis CS, Fisichella PM (2011) Current applications of evolving methodologies in gastroesophageal reflux disease testing. Dig Liver Dis 43(5):353–357
Ayazi S et al (2011) Day-to-day discrepancy in Bravo pH monitoring is related to the degree of deterioration of the lower esophageal sphincter and severity of reflux disease. Surg Endosc 25(7):2219–2223
Pandolfino JE et al (2005) Comparison of the Bravo wireless and Digitrapper catheter-based pH monitoring systems for measuring esophageal acid exposure. Am J Gastroenterol 100(7):1466–1476
Pandolfino JE et al (2005) Acid reflux event detection using the Bravo wireless versus the Slimline catheter pH systems: why are the numbers so different? Gut 54(12):1687–1692
Hakanson BS et al (2009) Comparison of wireless 48-h (Bravo) versus traditional ambulatory 24-h esophageal pH monitoring. Scand J Gastroenterol 44(3):276–283
McCollough M et al (2004) Proximal sensor data from routine dual-sensor esophageal pH monitoring is often inaccurate. Dig Dis Sci 49(10):1607–1611
Vaezi MF, Schroeder PL, Richter JE (1997) Reproducibility of proximal probe pH parameters in 24-hour ambulatory esophageal pH monitoring. Am J Gastroenterol 92(5):825–829
Ayazi S et al (2009) Bravo catheter-free pH monitoring: normal values, concordance, optimal diagnostic thresholds, and accuracy. Clin Gastroenterol Hepatol 7(1):60–67
Kim TH et al (2008) Pepsin detection in the sputum/saliva for the diagnosis of gastroesophageal reflux disease in patients with clinically suspected atypical gastroesophageal reflux disease symptoms. Digestion 77(3–4):201–206
Pandolfino JE et al (2003) Ambulatory esophageal pH monitoring using a wireless system. Am J Gastroenterol 98(4):740–749
Scarpulla G et al (2007) The impact of prolonged pH measurements on the diagnosis of gastroesophageal reflux disease: 4-day wireless pH studies. Am J Gastroenterol 102(12):2642–2647
Ahlawat SK et al (2006) Day-to-day variability in acid reflux patterns using the BRAVO pH monitoring system. J Clin Gastroenterol 40(1):20–24
Grigolon A et al (2011) Diagnostic yield of 96-h wireless pH monitoring and usefulness in patients’ management. Scand J Gastroenterol 46(5):522–530
des Varannes SB et al (2005) Simultaneous recordings of oesophageal acid exposure with conventional pH monitoring and a wireless system (Bravo). Gut 54(12):1682–1686
Williams RB et al (1999) Esophagopharyngeal acid regurgitation: dual pH monitoring criteria for its detection and insights into mechanisms. Gastroenterology 117(5):1051–1061
Pandolfino JE, Kwiatek MA (2008) Use and utility of the Bravo pH capsule. J Clin Gastroenterol 42(5):571–578
Brown SR et al (2011) Clinical outcomes of atypical extra-esophageal reflux symptoms following laparoscopic antireflux surgery. Surg Endosc 25(12):3852–3858
Hamdy E et al (2009) Response of atypical symptoms of GERD to antireflux surgery. Hepatogastroenterology 56(90):403–406
Farrell TM et al (2001) Response of atypical symptoms of gastro-oesophageal reflux to antireflux surgery. Br J Surg 88(12):1649–1652
Johnson WE et al (1996) Outcome of respiratory symptoms after antireflux surgery on patients with gastroesophageal reflux disease. Arch Surg 131(5):489–492
Disclosures
Michelle S. Han MD, Michal J. Lada MD, Dylan, R. Nieman MD, PhD, Andreas Tschoner MD, Christian G. Peyre, MD, Carolyn E. Jones MD, Thomas J. Watson MD, and Jeffrey H. Peters MD have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Han, M.S., Lada, M.J., Nieman, D.R. et al. 24-h multichannel intraluminal impedance-pH monitoring may be an inadequate test for detecting gastroesophageal reflux in patients with mixed typical and atypical symptoms. Surg Endosc 29, 1700–1708 (2015). https://doi.org/10.1007/s00464-014-3867-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3867-1