Abstract
Introduction
Gastroparesis is a common chronic and costly disorder for which medical therapy is often unsuccessful. Gastric electrical stimulation (GES) has been used to treat refractory cases, however, response is variable and difficult to predict. This study aims to assess whether pre-operative opioid analgesics (OA) use affects clinical success of GES.
Methods
Records of 128 patients who underwent laparoscopic GES placement from March 2001 to September 2012 were analyzed retrospectively. Data collected included demographics, surgical outcomes, and clinical parameters. Pre- and post-operative opioid analgesic dosing (No = 0 morphine equivalents (ME)/day, Low = 0–40 ME/day, Mid = 41–80 ME/day, High >80 ME/day), as well as clinical symptom assessment was collected for up to 3 years post-operatively. Clinical success was defined as (1) OA reduction of >50 %, (2) maintenance of weight, or (3) symptom improvement. Descriptive statistics were computed for all factors. A p < 0.05 was considered statistically significant.
Results
Fifty-three patients were on OA pre-operatively compared to 69 patients who were not. Patients not on OA pre-operatively were less likely than those on OA pre-op group to be on OA post-operatively (p = 0.005); however, there were no differences in weight or symptom improvement. Sub-group analysis of the 53 patients on OA demonstrated significant improvement in clinical symptoms in the low-morphine cohort compared to the mid-morphine cohort (p = 0.02), and OA dosing post-operatively in the low-morphine cohort diminished significantly compared to mid- and high-morphine cohort (p = 0.032). There was no significant difference in weight.
Conclusion
OA dosing pre-operatively significantly affects clinical success of GES placement. Criteria for offering GES implantation may need to take OA dosing into consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastroparesis is a chronic disorder defined by delay in emptying of the stomach and is most commonly characterized by nausea, vomiting, epigastric pain, early satiety, fullness, and bloating [1]. Gastroparesis occurs in up to 5 million patients in the United States and typically affects the younger population. The female to male ratio is approximately 4:1 [2]. Sex-specific incidence per 100,000 persons with gastroparesis between the reported years 1996 and 2006 was 9.8 % in women and 2.4 % in men [3]. Medical therapy consists of prokinetic and antiemetic agents, with the aim of the therapy being symptom relief. Despite medical therapy, patients may continue to experience symptoms, such as pain, often leading to the use of opioid analgesia (OA). Gastric electrical stimulation (GES) therapy has been used to treat medically refractory cases of gastroparesis. At our institution, most GES are implanted with a laparoscopic approach. Response to GES treatment is variable, and predicting improvement is difficult. The aim of the current study is to assess whether OA use preoperatively is associated with the clinical success of GES.
Methods
Patients
After Institutional Review Board approval, pre- and post-operative data were collected in all patients who underwent GES placement (Enterra Therapy System: Medtronic, Minneapolis, MN, USA) between 2001 and 2012. Pre-operative variables included: past medical history, weight, body mass index, medications used and discontinued, OA usage, pre-operative work-up, and nutritional support was input into the database. Post-operative variables included weight, medications used, discontinued medications, OA use, nutritional support, complications, and post-operative results. OA dosing pre- and post-operatively [No = 0 morphine equivalents (ME)/day, Low = 0–40 ME/day, Mid = 41–80 ME/day, High > 80 ME/day], as well as clinical symptom assessment was collected for up to 3 years post-operatively at 1-, 3-, and 6-month, and 1-, 2-, and 3-year post-operative follow-up intervals. Opioid analgesic (OA) use was determined by chart review of clinic notes both pre-operatively and post-operatively, and was corroborated through validation by reviewing the medications in the medications list for each individual under the medications tab in our electronic medical records (EMR). Furthermore, our group didn’t calculate OA use for an interval of 4 weeks post-operatively to allow sufficient time for resolution of post-operative pain, this was done to avoid calculating OA use for post-operative pain control versus pain related to gastroparesis.
Our group defined the clinical success as (1) OA dose reduction of >50 %, (2) maintenance or increased weight, or (3) symptom improvement. Symptom improvement was based on a subjective evaluation reported by each individual patient.
The primary outcome of the study was whether there was a difference in clinical success as defined above (individual and combined metrics) in patients who were on pre-operative OA compared to those who were not. Secondary outcomes were (1) whether there was a difference in clinical success in patients on low, mid, and high pre-operative OA dosing and (2) whether there was a difference in clinical success in patients who were on short-term OA (defined as less than 1 month) compared to chronic OA (defined as greater than 1 month).
Statistical analysis
Data are presented as mean ± SD for continuous variables and frequency percentages for categorical variables. The distribution of the data was checked for normality using the Shapiro–Wilk test. These characteristics were analyzed using unpaired student’s t test (or Mann–Whitney test) for continuous variables and Chi square test (or Fisher’s exact test) for categorical variables. All tests were two-tailed and the results with a p < 0.05 were considered statistically significant. Additionally, Cox regression was used to assess the role of OA in GES success. A p value <0.05 was considered statistically significant. Statistical analyses were performed using the software package IBM SPSS, version 21.0 for Windows (Armonk, NY, USA).
Results
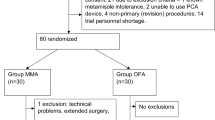
Patient demographics are listed in Table 1. A total of 128 patients underwent gastric electrical stimulator placement during the study period with six patients lost to follow up in regards to opioid usage (Fig. 1). The remaining 122 patients were analyzed.
Primary outcome
Fifty-three patients were on OA pre-operatively compared to 69 patients who were not. Patients who were not on OA pre-operatively were less likely than those on OA pre-op group to be on OA post-operatively (p = 0.005); our group classified low OA use to be 0–40 ME, mid OA use to be 40–80 ME, and high OA to be >80 ME. The high-morphine group had significantly higher failure rate for morphine usage (p = 0.03). There was no statistical significance for “symptom improvement” or “maintenance of weight” (p = 0.09).
Secondary outcomes: We further conducted a sub-group analysis on the 53 patients receiving OA pre-operatively. The mid-morphine cohort had significantly higher clinical failure rates compared to the low-morphine cohort (p = 0.02), as expected, high-morphine sub-group analysis had significantly higher failure rate by morphine usage criterion (p = 0.03). Details of the statistical results are shown in Fig. 2. Multivariable analysis confirms that OA is an independent risk factor for GES failure Table 2.
Discussion
There is variable clinical success in the use of GES placement for gastroparesis. Our group recently published a study demonstrating no difference between those who received GES for idiopathic gastroparesis and those who received GES for diabetic gastroparesis in terms of overall symptoms improvement and weight maintenance. Hence, it became vital to ascertain what other factors may be playing a role in GES clinical success if disease etiology does not. To the best of our knowledge, this is the first study of its kind evaluating and demonstrating that OA use pre-operatively impacts clinical success in patients who undergo GES placement.
OA use has played a significant role in gastroparesis management, since abdominal pain is often a predominant symptom. For this reason, we considered it important to include OA use as one of the parameters of success. Our findings demonstrate that a significant number of patients continued the use of OA therapy post-operatively and overall were less likely to benefit from GES placement. There may be biochemical causes for this finding. Chronic pain is thought to be less about an increase in afferent visceral stimuli and more about the central nervous system [4]. Patients who develop increased pain sensitivity despite treatment with OA can develop opioid-induced hyperalgesia, an adverse effect of chronic use of OA, [5, 6] which is thought to be related to the effects by opioid metabolites, such as morphine 3-gluceronide (M3G) [7]. This has been confirmed by studies conducted on patients with chronic opioid use [8].
There are at least three mechanisms induced by chronic opioid use, leading to a hyperalgesic state: (1) bimodal opioid dysregulation, in which both the excitatory and inhibitory modulation of sensory neuron action by opiates mediated by G s receptor activation at the dorsal root ganglia leading to hyperalgesia [9, 10]. (2) Counter-regulatory mechanisms, due to increase in dynorphin production causing further hyperalgesia, and (3) glial activation and opioid facilitation, where the use of OA binds to the mu receptor causing an activation of glia and leading to a release of inflammatory cytokines causing glial cells to increase, furthermore increasing receptor expression causing an increase in the development of hyperalgesia [10–12].
In short, chronic use of OA post-operatively will alter pain perception in these individuals. The use of OA may initially control the symptoms of abdominal pain early on in the course of treatment, but as the use of OA over time continues, this will lead to a reduction of pain tolerance due to chronic suppression of pain with continuous use of OA. The pain-free periods become shorter in duration despite increasing doses of opiates. OA use must be taken into high consideration in treatment of post-operative pain symptoms, or patients may ultimately face clinical failure.
In terms of failure of nutritional improvement, of all patients who needed supplemental nutrition at some point during their GES therapy (N = 12), only six required supplemental nutrition at last follow-up. Six out of these 12 patients had no improvement of symptoms, which led to persistent need for enteral access. The other six patients had improvement of symptoms but required ongoing nutritional supplementation due to the severity of their malnutrition or symptom constellation. These findings confirm the theory that gastroparesis is a disorder with a broad spectrum of symptom duration and severity, and long-term follow-up with a multi-disciplinary approach is required [13]. A particular challenge arises when addressing patients with both medically refractory gastroparesis and class I or II obesity. Those with class II obesity remained obese following GES placement, and several patients with class I obesity converted to class II obesity during the study period [13].
Secondary outcomes
Low-morphine usage (0–40 ME/day) had the greatest symptom improvement, whereas mid-morphine usage (41–80 ME/day) had a significant failure rate. The reason for this is not completely clear, although opioid-induced hyperalgesia may be partly playing a role.
Opioid analgesics have variable effects on gastric motility. Opioid-induced bowel dysfunction (OIBD) may cause symptoms ranging from nausea and vomiting, delay in gastric emptying (causing symptoms of GERD), abdominal pain, bloating, flatulence, constipation, hard stools, and severe straining during bowel movements [14]. More serious complications such as fecal impaction, pseudo- obstruction, and pseudo- obstructions leading to perforation have been previously documented [15]. Various sources note that 40–95 % of patients using OA are prone to develop opioid-induced constipation (OIC) and decrease gastric motility [16]. This is of significant importance for patients who suffer from gastric motility disorders such as gastroparesis. Opioids enhance their effect on the gut through three receptors: μ-, δ-, and κ- opioid receptors. The majority of opioids exert their effects primarily through the μ-receptors, which are located on the myenteric and submucosal neurons [17]. These receptors are primarily in the stomach and proximal colon. OIC is achieved through various mechanisms within the gut. Opioids cause a delay in intestinal transit through the stimulation of non-propulsive motility, increase of intestinal tone, and stimulation of sphincters of the gut, such as the pyloric and ileocecal sphincters, through the μ-receptors in the myenteric and submucosal neurons. Furthermore, opioids enhance fluid absorption by delay in transit time, which causes a prolonged contact time for absorption, and lastly causing the stimulation of mucosal sensory receptors [18].
There are several limitations to our study that need to be acknowledged. This is a retrospective database study which poses its own inherent limitations. Although this is the biggest study of its kind up-to-date, the number of the patients is a possible limiting factor. One possible limitation is the fact that our institution is a tertiary care center that has a main campus as well as small satellite hospitals with their own independent inpatient facilities. Some patients may have been lost to follow up, or had medication adjustments that we did not detect. We also consider the review of OA medications through our chart review to be a possible limitation of our study. Review of OA medications was dependent on the accuracy of medical records in addition to the frequency, and the number of follow-up visits of each individual patient.
Additionally, standardization was performed of dosing which was achieved by converting all dosage of narcotic analgesics to morphine equivalents, and maximal possible dosages of patient prescriptions were used in calculations to maintain consistency in our results. Because of this, our results may reflect an overestimation of dosage received by the patients, but this effect is consistent across all patients.
Conclusion
In conclusion, the findings of this study support the importance of reducing and if possible, eliminating pre-operative OA use prior to GES placement. There is now evidence that there may be a dose response correlation with clinical success. Future protocols determining candidacy for GES implantation should consider OA dosing although multicenter, prospective trials are needed to confirm this finding.
References
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L (2013) Clinical guideline: management of gastroparesis. Am J Gastroenterol 108:18–37. doi:10.1038/ajg.2012.373.Clinical quiz 38
Stanghellini V, Tosetti C, Paternico A, Barbara G, Morselli-Labate AM, Monetti N, Marengo M, Corinaldesi R (1996) Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology 110:1036–1042
Camilleri M, Bharucha AE, Farrugia G (2011) Epidemiology, mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol 9:5–12. doi:10.1016/j.cgh.2010.09.022 quiz e7
Nozu T, Kudaira M (2009) Altered rectal sensory response induced by balloon distention in patients with functional abdominal pain syndrome. Biopsychosoc Med 3:13. doi:10.1186/1751-0759-3-13
Mercadante S, Villari P, Ferrera P (2003) Burst ketamine to reverse opioid tolerance in cancer pain. J Pain Symptom Manag 25:302–305
Mercadante S, Arcuri E (2005) Hyperalgesia and opioid switching. Am J Hosp Palliat Care 22:291–294
Mao J, Sung B, Ji R–R, Lim G (2002) Neuronal apoptosis associated with morphine tolerance: evidence for an opioid-induced neurotoxic mechanism. J Neurosci 22:7650–7661
Pud D, Cohen D, Lawental E, Eisenberg E (2006) Opioids and abnormal pain perception: new evidence from a study of chronic opioid addicts and healthy subjects. Drug Alcohol Depend 82:218–223. doi:10.1016/j.drugalcdep.2005.09.007
Crain SM, Shen KF (2000) Antagonists of excitatory opioid receptor functions enhance morphine’s analgesic potency and attenuate opioid tolerance/dependence liability. Pain 84:121–131. doi:10.1016/S0304-3959(99)00223-7
Grunkemeier DMS, Cassara JE, Dalton CB, Drossman DA (2007) The narcotic bowel syndrome: clinical features, pathophysiology, and management. Clin Gastroenterol Hepatol 5:1126–1139. doi:10.1016/j.cgh.2007.06.013 quiz 1121–1122
Farmer AD, Ferdinand E, Aziz Q (2013) Opioids and the gastrointestinal tract—a case of narcotic bowel syndrome and literature review. J Neurogastroenterol Motil 19:94–98. doi:10.5056/jnm.2013.19.1.94
Watkins LR, Hutchinson MR, Johnston IN, Maier SF (2005) Glia: novel counter-regulators of opioid analgesia. Trends Neurosci 28:661–669. doi:10.1016/j.tins.2005.10.001
Timratana P, El-Hayek K, Shimizu H, Kroh M, Chand B (2013) Laparoscopic gastric electrical stimulation for medically refractory diabetic and idiopathic gastroparesis. J Gastrointest Surg 17:461–470. doi:10.1007/s11605-012-2128-7
Brock C, Olesen SS, Olesen AE, Frøkjaer JB, Andresen T, Drewes AM (2012) Opioid-induced bowel dysfunction: pathophysiology and management. Drugs 72:1847–1865. doi:10.2165/11634970-000000000-00000
Leppert W (2013) New treatment possibilities for opioid-induced bowel dysfunction. Pain 154:1491–1492. doi:10.1016/j.pain.2013.06.010
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, Glaser SE, Vallejo R (2008) Opioid complications and side effects. Pain Phys 11:S105–S120
Ketwaroo GA, Cheng V, Lembo A (2013) Opioid-induced bowel dysfunction. Curr Gastroenterol Rep 15:344. doi:10.1007/s11894-013-0344-2
Camilleri M (2011) Opioid-induced constipation: challenges and therapeutic opportunities. Am J Gastroenterol 106:835–842. doi:10.1038/ajg.2011.30 quiz 843
Disclosures
Dr. Mena Boules, Dr. Hideharu Shimizu, Dr. Andrea Zelisko, Dr. Kevin El-Hayek, Dr. Maged Rizk, and Dr. Matthew Kroh have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boules, M., Shimizu, H., Zelisko, A. et al. Pre-operative opioid analgesia reduces clinical success of laparoscopic gastric electrical stimulation placement in patients with gastroparesis. Surg Endosc 29, 805–809 (2015). https://doi.org/10.1007/s00464-014-3754-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3754-9