Abstract
Background
In the last decade, the robotic platform has been used in different surgical fields. However, the field of foregut and bariatric surgery is still evolving. Most surgeons still prefer laparoscopic techniques because it has proven clinical benefits, does not require complex setups, and does not have high costs compared with that of robotics. The aim of this article is to review the outcomes of foregut and bariatric surgery and its potential clinical advantages.
Methods
We performed a search on PUBMED for the most relevant articles published in the field of robotic bariatric and foregut surgery in the last 15 years. More than 40 articles were selected and included on this review. Several systematic reviews were also included. Very few randomized clinical trials are available.
Results
For the most part, robotic procedures were associated with better ergonomics for the surgeon, better visualization of the anatomy, easier fine dissection (i.e., lymphadenectomy) when required, and higher costs. In foregut surgery, the robotic system is associated with a significant lower rate of mucosal perforation in Heller myotomy compared to laparoscopy. In bariatric surgery, the clinical advantages have not been well documented yet; however, it seems robotics shortens the learning curve of Roux-en-Y gastric bypass (RYGB).
Conclusion
Foregut and bariatric robotic surgery is a surgical field still in development. For the vast majority of the procedures in this area, the clinical outcomes of robotic surgery are the same of standard laparoscopy. However, the use of robots in selected cases may have specific advantages and may overcome the limitations of laparoscopic surgery. More research is needed, especially large and well-designed randomized clinical trials, to elucidate more accurate conclusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Before the Food and Drug Administration (FDA) approved the use of the Da Vinci surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA) in 2000, more than 300 cases had been performed outside the US. Most of them were cholecystectomies and gastric fundoplications and provided the data for the FDA application about the use of computerized telesurgical devices in general surgery [1]. In 2001, Marescaux and colleagues reported the first transatlantic robot-assisted telesurgery procedure performing a cholecystectomy of a patient in Strasbourg, France, from New York City, US [2]. Since then, multiple robotic surgical procedures have been performed in the US involving the fields of urology, gynecology, cardio-thoracic, and general surgery. However, the field of general surgery has been slow in adopting this technology when compared to the other specialties. It is believed that this difference in robotic implementation among specialties could be explained by conditioning factors like surgeon endoscopic skill level, equipment limitations, and procedure complexity [3].
Implementing a robotic program in general surgery is highly dependent on the amount of time a surgeon is willing to give as well as enthusiasm from the institution to house the robot hardware. Financial support, appropriate facilities, and demand from the patient population to sustain the program are also needed. We have implemented the robotic general surgery program in our institution during the last 10 months. Our surgical team is composed of two laparoscopic surgeons and two clinical fellows. We started the training by completing industry designed online modules, tasks on a simulator, and dry labs. We demonstrated on a previous publication that robotic simulators improve the surgeon’s performance in selected drills [4]. Depending on the institution, the surgeon will have to perform a certain amount of supervised cases prior to obtaining full privileges. Currently, there are no formal robotic training centers but high-volume centers may host certain events.
We have observed that once the surgical team develops experience about patient safety precautions, operating room (OR) setup, and type of instruments needed; the robotic platform can be used efficiently in general surgery with similar clinical outcomes to laparoscopic cases. Our goal with this article is to perform a literature review about the outcomes of foregut and bariatric surgery and its potential clinical benefits. Studies including the most commonly performed procedures in these areas are discussed in this article. Certain technical aspects like docking and OR setup for upper abdominal procedures are also mentioned.
In this review, recommendations were classified according the levels of evidence in Grades A, B, or C as follows: Grade A. There is good research-based evidence to support the statement (prospective, randomized trials), Grade B. There is fair research-based evidence to support the statement (well-designed studies without randomization), and Grade C. The statement is based on expert opinion, minor reports, and editorial consensus.
Overview and robot setup
Robot-assisted general and foregut surgery is still a field in development. However, comparing with the traditional laparoscopic approach there are several potential advantages with the robotic system. It can overcome the limitations of standard laparoscopic instrumentation and provide an excellent interface for the surgeon [1]. These advantages, common to other surgical procedures, include high definition magnification of the surgical field, superior binocular three-dimensional visualization of the anatomy, full range of motion with articulated instruments, tremor filtration and motion scaling, and comfortable ergonomics for the surgeon [1, 3, 5]. Thus, the use of the robotic system may improve the surgeon skills during dissection and this might result in better clinical outcomes in certain cases [5]. In the particular field of upper gastrointestinal (UGI) surgery, some studies have demonstrated other additional benefits by using the robotic platform (Table 1).
By the contrary, there are also some well-known disadvantages of the robot. The only commercially available robotic system is still a bulky instrument with three large and heavy components [5, 6]. For upper abdominal procedures, the bedside cart needs to be often docked from above the patients head or left shoulder, limiting the access of the anesthesiologist to the airway and the surgeon for performing intraoperative endoscopy. Repositioning of the patient bed is not possible once the robot is docked so the bedside surgeon must undock the robot first before the table could be relocated [6]. In addition, the lack of haptic feedback may lead to tissue trauma during some procedures [3, 5, 6]. However, once the surgical team acquires some experience, we believe some of these limitations can be minimized allowing the safe and efficient use of the robotic system. In addition, the recently unveiled da Vinci Xi® model also promises to address many of the above restrictions.
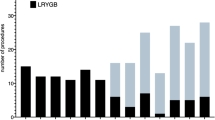
Different combinations of OR setup and docking have been reported. However, we found that docking the robot from above the patient’s head has been reproducible and the easiest for our surgical team to learn (Fig. 1). The patient is intubated in the regular position by the anesthesia staff. Once this is done, all tubing and monitoring devices are disconnected in order to turn the operating table 180°. The patient-side cart is set for docking from above the patient’s head. The surgeon is seated at the console which is located at the right of the operating table. The assistant surgeon is at the patient’s left. Vision cart and auxiliary monitors are placed at different angles facilitating the visualization to all the members of the team. For most of the procedures, we used the four-arm robotic system (Da Vinci® SI), three 8 mm robot trocars, two 12 mm trocars, and usually the same set of three or four robot instruments. The table is placed in reverse trendelenburg position before docking is done. Trocar placement is quite different to the one we use in laparoscopic cases (Fig. 2). In the early experience in our institution, we have safely performed more than 70 procedures of general robotic surgery, most of them were bariatric and foregut cases (Table 2).
OR setup for foregut and bariatric operations. Diagram indicating our OR setup for all foregut operations. The operating table is turned 180°. The patient-side cart is set for docking from above the patient’s head. The surgeon is seated at the console which is located at the right of the operating table. The assistant surgeon is at the patient’s left
Trocar placement for UGI robotic procedures. Diagram showing the patient positioning, trocar placement, and bedside surgeon positioning we use for most of robotic foregut procedures. In addition, it shows a comparison between laparoscopic (L) and robotic (R) trocar placement. “A” indicates the assistant trocar used during robotic procedures for stapling, suture passing, and irrigation/suctioning. UGI upper gastrointestinal
Procedures and outcomes
Heller myotomy
For delicate procedures like Heller myotomy, the robotic system offers superior visualization and may allow a more precise dissection technique. Melvin et al. [7], in a series of 104 patients with achalasia underwent robotic Heller myotomy, reported no esophageal mucosa perforations and suggested that the robotic technique may provide superior outcomes in selected procedures compared to regular laparoscopy. Afterwards, Horgan and colleagues [8] compared the outcomes of laparoscopic vs. robotic myotomy. The operative time between the groups was longer for the robotic procedure (141 ± 49 vs. 122 ± 44 min; P < 0.05); however, times were not different comparing the last 30 cases. There was no difference in dysphagia relief at short term and again, the rate of mucosal perforation was higher for the laparoscopic group (16 vs. 0 %; P < 0.01). The authors believe the freedom of movement and the three-dimensional visualization which allow better identification to divide each individual muscular fiber are key factors to ensure adequate and safe myotomy.
Subsequent reports have confirmed these previous findings regarding laparoscopic vs. robotic myotomy. According to these results, both procedures result in more than 90 % relief of symptoms but the robotic procedure is associated with 0 % mucosal perforation rate [9]. However, it is important to note that the clinical relevance of mucosal perforation during the procedure is uncertain since most of them are detected and repaired intraoperatively. We found no specific analysis addressing the postoperative outcomes of this specific subset of patients. In a large retrospective study including 2,683 patients who underwent open, laparoscopic, and robotic Heller myotomy, a comparative analysis was performed. Comparing laparoscopic and robotic procedures, no difference in morbidity, mortality, length of stay, or readmission rate was found. Both laparoscopic and robotic were superior to open myotomy regarding perioperative outcomes. However, the robotic myotomy group had a significantly higher cost than the other two groups [10].
In brief, after the learning curve is reached, laparoscopic and robotic Heller myotomy are comparable in clinical outcomes and operative times but the robotic procedure appears to have a lower risk of mucosal perforation and a higher cost [6, 11] (evidence Grade B/C).
Hiatal hernia repair and fundoplication
The first two cases of robot-assisted Nissen fundoplications were performed by Cadiere et al. [12]. They analyzed their series and found that the robotic procedures were associated with significantly longer operative times compared with standard laparoscopic cases and the postoperative outcomes were similar in both groups. Melvin et al. [13] confirmed these results in a prospective non-randomized trial comparing robotic vs. laparoscopic Nissen fundoplication. There were no differences regarding clinical outcomes in both groups; however the robotic procedures took approximately 45 min longer. Another early series including six patients, reported that the use of four-arm robotic system can be used safely and effectively for performing gastric fundoplications without complications related to the instruments [14].
In a systematic literature review and meta-analysis, six randomized trial including 226 patients were included. The standard laparoscopic approach and robotic fundoplication were compared. The study demonstrated that robotic surgery currently does not offer any additional clinical benefits compared to conventional laparoscopic Nissen fundoplication, but is associated with increased operative time and cost [15]. Wang et al. [16], on a similar review, found no differences regarding the clinical results but the operative times again were longer for the robotic arm. They concluded laparoscopic fundoplication remains as the standard approach since it is associated with shorter operative time and lower cost.
The literature about robotic repair of hiatal hernias is scarce. We found one recent study that included 42 patients with paraesophageal hernias (PEH). Patients were divided in three groups: 12 robotic, 17 laparoscopic, and 13 open repairs, respectively. Analysis regarding perioperative outcomes showed robotic repair is superior to open repair but it is comparable to the laparoscopic approach. Again, operative times were longer for the robotic group and the authors concluded there is no additional benefit by using this technology [17].
In summary, robotic anti-reflux surgery seems not to offer additional advantages comparing with the laparoscopic approach. Operative times and costs are higher (evidence Grade A/B). However, we believe robot-assisted procedures may be useful in patients undergoing to redo operations or patients with large hiatal hernias in whom surgical dissection is expected to be more challenging. There is little objective data to assess this assumption (evidence Grade C) [6, 11].
Esophagectomy
Horgan et al. [18] reported the first robotic-assisted esophagectomy in 2003. However, the adoption of robotics for this procedure has been less enthusiastic since there is scarce data that demonstrates improved outcomes in terms of morbidity, operative times, or costs compared with laparoscopic or thoracoscopic techniques [5, 19]. Galvani et al. [20] performed 18 robotic-assisted transhiatal esophagectomies for adenocarcinoma with no hospital mortality and minimal morbidity. However, a third of the patients experienced leaks and strictures. The authors highlighted the advantages of using the robotic system such as easier dissection in narrow spaces like the mediastinum and the possibility of performing a more proximal dissection beyond the level of the carina since robotic instruments are 7.5 cm longer than standard laparoscopic ones. Another similar series included 32 patients who underwent esophagectomy through laparoscopy and prone position robot-assisted thoracoscopy with cervical anastomosis. Mean operative time was 210 min, mean blood loss was 80 ml, and mean length of stay was 9 days. They were able to retrieve an average of 20 mediastinal lymph nodes. The leak rate was 9.3 % [21]. No long-term follow-up and survival was provided in this study.
Two other recent series of robotic esophagectomies exhibit similar results in terms of perioperative outcomes. Reported operative times range from 311 to 556 min, estimated blood loss from 97 to 307 ml, and length of stay from 9 to 10 days. Median number of lymph nodes was around 20 for both. Global morbidity was around 24 % with a leak rate from 14 to 25 %, and 30-day mortality of 2.5 % [22, 23]. One study reported a mean disease-free survival of 20 months [22]. We found no prospective comparative trials among the different minimally invasive techniques for esophagectomy. With the few data available and the small number of patients analyzed, there are no clear benefits of robotic esophagectomy compared with the regular laparoscopic/thoracoscopic approach. Longer operative times and higher costs may be limiting factors for the adoption of this technique [6] (evidence Grade C).
Gastrectomy
Regarding gastric cancer, most of the published studies have no shown big differences between laparoscopic and robotic gastrectomy in terms of morbidity, mortality, and oncologic results [24, 25]. However, the robotic approach may facilitate a reproducible D2 lymph node dissection, improve performance of complex in-bloc resections, and intracorporeal reconstruction techniques including esophagojejunostomy following total gastrectomy [26]. One of the earliest series included 100 patients (33 total and 67 subtotal robotic-assisted gastrectomies). All the dissection was done by using robotic approach and then a minilaparotomy was made to perform the anastomosis. Mean operative time, number of retrieved lymph nodes, and length of stay were 231 min, 36.7 nodes, and 7.8 days, respectively. Leak rate was 2 % and mortality was 1 % [27].
Another comparative study included more than 680 patients who underwent open, laparoscopic, or robotic gastrectomy. The authors demonstrated significantly less blood loss and shorter length of stay in the robotic gastrectomy group [24]. However, the robotic procedure was also associated with a significantly longer operative time and higher cost (more than double). Kang et al. [25] confirmed the previous results and reported less blood loss in the robotic group but the other outcomes were otherwise comparable to laparoscopic gastrectomy. Both studies suggested a learning curve for robotic gastrectomy of about 20–25 cases.
In summary, the current literature exhibits only case series and randomized trials are needed to evaluate better the results of robotic gastrectomy. This approach appears to offer less blood loss and easier lymphadenectomy than the laparoscopic procedure although it leads to longer operative times and higher costs [28] (evidence Grade B/C).
Bariatric surgery
Cadiere et al. [29] reported the first robotic-assisted adjustable gastric band (AGB) placement in 1999. The first series of robotic Roux-en-Y gastric bypass (RYGB) was published by Horgan and colleagues [30]. Many other bariatric procedures including sleeve gastrectomy (SG), biliopancreatic diversion with or without duodenal switch (BPD/DS), and revisional procedures have been performed safely with the robotic platform. Potential advantages of this approach in bariatrics include an improved ergonomics against a thick and heavy abdominal wall, better mobility in small working spaces such as below large livers, and shorten learning curve for complex procedures like RYGB [3, 5, 31].
Adjustable gastric band
AGB is a procedure less commonly performed around the world and other more definitive operations with better outcomes like SG are replacing this modality of treatment. Furthermore, the general conception of using the robot for band placement is that this approach does not offer any additional benefit comparative with laparoscopy but longer operative times and higher costs [11]. However, Edelson et al. [32], in one of the largest series published, compared 287 AGB placed robotically and 120 laparoscopically. Both approaches were similar in operative time, morbidity and length of stay; for patients with BMI >50 kg/m2 the operative time was shorter using the robotic technique. We recommend looking at these results carefully since we believe super obese patients need a different surgical approach other than AGB. As we mentioned earlier, gastric banding is decreasing overtime and may become a historical procedure in the near future (evidence Grade B/C).
Roux-en-Y gastric bypass
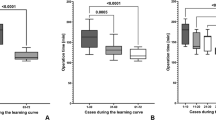
Several series have shown comparable results of robotic RYGB with the standard laparoscopic approach [33–37]. Hubens et al. [33] reported the results of 45 robotic RYGB and demonstrated no difference in clinical outcomes with regular laparoscopy but significantly longer operative time. The authors highlighted that the robot techniques can facilitate the hand-sewn anastomosis and suggested a learning curve of 35 cases. The largest series reported compared 320 robotic RYGB vs. 356 laparoscopic RYGBP. They found the robotic arm had a mean operative time of 192, mean length of stay of 2.7 days, and a significantly lower leak rate comparing to laparoscopic arm [34]. A subsequent report found no big differences between both approaches but interestingly, the operative time was significantly shorter in the robot group (207 vs. 227 min, P < 0.001) [35].
A systematic literature review included seven studies with a total of 1,686 patients and made a comparison of the robotic approach with the laparoscopic one. The authors found no significant differences in operative times, length of stay, leaks, and mortality but a reduced incidence of anastomotic stricture in the robot group (P = 0.04) [38]. A recent report analyzed the costs of laparoscopic, robotic, and open RYGBP. Interestingly, the robotic group was cheaper when compared to the other two groups; however, it is important to note that laparoscopic cases were performed by using stapled anastomosis and robot cases were performed with a hand-sewn technique—a fact that could explain the cost savings in the robotic approach [39]. In brief, robot-assisted RYGB is feasible and safe, it offers similar outcomes of that laparoscopy, and may shorten the learning curve. More well-designed studies are required to determine if there is any superiority over the standard laparoscopic approach (evidence Grade B/C).
Sleeve gastrectomy
SG is a relatively novel procedure that is gaining acceptance because of its technical simplicity, low morbidity, and excellent outcomes. It has been performed robotically; however, the scarce reports reviewed did not report considerable differences compared to the standard laparoscopic approach. Vilallonga et al. [40] reported a series of 32 patients who underwent robotic SG. They concluded the technique is feasible and safe, and found a learning curve of about 20 cases. Another report compared 200 patients who underwent either robotic or laparoscopic SG. No clinical differences were found in both groups although the robotic arm had a significantly longer operative time (P < 0.005) [41]. A similar study confirmed prolonged operative times in the robotic arm without any other important difference [42]. An interesting case report about an obese patient with a history of allergy to metallic devices including nickel was published recently. The authors performed a novel approach on this patient with a robotic staple less SG avoiding the use of metallic staples and closing the stomach by using a hand-sewn technique [43].
In summary, robotic SG seems to have no additional advantages over its counterpart laparoscopic approach and the technique is associated with longer operative times. However, we believe since the procedure is usually a straightforward case, it might be a good start for general surgeons interested in robotics implementation to their practice (evidence Grade B/C).
Conclusions
Foregut and bariatric robotic surgery is a surgical field in development. For the vast majority of the procedures in this area, the clinical outcomes of robotic surgery are similar to the standard laparoscopic approach. However, the use of robots in selected cases may have specific clinical advantages and may overcome the limitations of laparoscopic surgery. In foregut surgery, the main advantage of robotics seems to be in procedures where better visualization and highly fine dissection is required such as Heller myotomy, redo operations, and oncologic resections including lymphadenectomy. In bariatric surgery, the key advantage of the robotic system is the improved ergonomics which is more notorious on obese population with a heavy abdominal wall, and the shorter learning curve for RYGB. More research is needed, especially large and well-designed randomized clinical trials to elucidate more accurate conclusions.
References
Melvin WS, Needleman BJ, Krause KR, Schneider C, Wolf RK, Michler RE, Ellison EC (2002) Computer-enhanced robotic telesurgery. Initial experience in foregut surgery. Surg Endosc 16:1790–1792
Marescaux J, Leroy J, Gagner M, Rubino F, Mutter D, Vix M, Butner SE, Smith MK (2001) Transatlantic robot-assisted telesurgery. Nature 413:379–380
Wilson EB (2009) The evolution of robotic general surgery. Scand J Surg 98:125–129
Patel A, Patel M, Lytle N, Toro JP, Medbery RL, Bluestein S, Perez SD, Sweeney JF, Davis SS, Lin E (2014) Can we become better robot surgeons through simulator practice? Surg Endosc 28(3):847–853
Ito F, Gould JC (2006) Robotic foregut surgery. Int J Med Robot 2:287–292
Kastenmeier A, Gonzales H, Gould JC (2012) Robotic applications in the treatment of diseases of the esophagus. Surg Laparosc Endosc Percutan Tech 22:304–309
Melvin WS, Dundon JM, Talamini M, Horgan S (2005) Computer-enhanced robotic telesurgery minimizes esophageal perforation during Heller myotomy. Surgery 138:553–558 discussion 558–559
Horgan S, Galvani C, Gorodner MV, Omelanczuck P, Elli F, Moser F, Durand L, Caracoche M, Nefa J, Bustos S, Donahue P, Ferraina P (2005) Robotic-assisted Heller myotomy versus laparoscopic Heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg 9:1020–1029 discussion 1029–1030
Galvani C, Gorodner MV, Moser F, Baptista M, Donahue P, Horgan S (2006) Laparoscopic Heller myotomy for achalasia facilitated by robotic assistance. Surg Endosc 20:1105–1112
Shaligram A, Unnirevi J, Simorov A, Kothari VM, Oleynikov D (2012) How does the robot affect outcomes? A retrospective review of open, laparoscopic, and robotic Heller myotomy for achalasia. Surg Endosc 26:1047–1050
Maeso S, Reza M, Mayol JA, Blasco JA, Guerra M, Andradas E, Plana MN (2010) Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg 252:254–262
Cadiere GB, Himpens J, Vertruyen M, Bruyns J, Fourtanier G (1999) Nissen fundoplication done by remotely controlled robotic technique. Ann Chir 53:137–141
Melvin WS, Needleman BJ, Krause KR, Schneider C, Ellison EC (2002) Computer-enhanced vs. standard laparoscopic antireflux surgery. J Gastrointest Surg 6:11–15 discussion 15–16
Newlin ME, Mikami DJ, Melvin SW (2004) Initial experience with the four-arm computer-enhanced telesurgery device in foregut surgery. J Laparoendosc Adv Surg Tech A 14:121–124
Markar SR, Karthikesalingam AP, Hagen ME, Talamini M, Horgan S, Wagner OJ (2010) Robotic vs. laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease: systematic review and meta-analysis. Int J Med Robot 6:125–131
Wang Z, Zheng Q, Jin Z (2012) Meta-analysis of robot-assisted versus conventional laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease. ANZ J Surg 82:112–117
Gehrig T, Mehrabi A, Fischer L, Kenngott H, Hinz U, Gutt CN, Muller-Stich BP (2013) Robotic-assisted paraesophageal hernia repair—a case–control study. Langenbeck’s Arch Surg 398:691–696
Horgan S, Berger RA, Elli EF, Espat NJ (2003) Robotic-assisted minimally invasive transhiatal esophagectomy. Am Surg 69:624–626
Watson TJ (2008) Robotic esophagectomy: is it an advance and what is the future? Ann Thorac Surg 85:S757–S759
Galvani CA, Gorodner MV, Moser F, Jacobsen G, Chretien C, Espat NJ, Donahue P, Horgan S (2008) Robotically assisted laparoscopic transhiatal esophagectomy. Surg Endosc 22:188–195
Puntambekar SP, Rayate N, Joshi S, Agarwal G (2011) Robotic transthoracic esophagectomy in the prone position: experience with 32 patients with esophageal cancer. J Thorac Cardiovasc Surg 142:1283–1284
Dunn DH, Johnson EM, Morphew JA, Dilworth HP, Krueger JL, Banerji N (2013) Robot-assisted transhiatal esophagectomy: a 3-year single-center experience. Dis Esophagus 26:159–166
Sarkaria IS, Rizk NP, Finley DJ, Bains MS, Adusumilli PS, Huang J, Rusch VW (2013) Combined thoracoscopic and laparoscopic robotic-assisted minimally invasive esophagectomy using a four-arm platform: experience, technique and cautions during early procedure development. Eur J Cardiothorac Surg 43:e107–e115
Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, Hsieh MC, Li AF, Chiou SH, Wu CW (2012) Initial experience of robotic gastrectomy and comparison with open and laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg 16:1303–1310
Kang BH, Xuan Y, Hur H, Ahn CW, Cho YK, Han SU (2012) Comparison of surgical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: the learning curve of robotic surgery. J Gastric Cancer 12:156–163
Coratti A, Annecchiarico M, Di Marino M, Gentile E, Coratti F, Giulianotti PC (2013) Robot-assisted gastrectomy for gastric cancer: current status and technical considerations. World J Surg 37(12):2771–2781
Song J, Oh SJ, Kang WH, Hyung WJ, Choi SH, Noh SH (2009) Robot-assisted gastrectomy with lymph node dissection for gastric cancer: lessons learned from an initial 100 consecutive procedures. Ann Surg 249:927–932
Marano A, Hyung WJ (2012) Robotic gastrectomy: the current state of the art. J Gastric Cancer 12:63–72
Cadiere GB, Himpens J, Vertruyen M, Favretti F (1999) The world’s first obesity surgery performed by a surgeon at a distance. Obes Surg 9:206–209
Horgan S, Vanuno D (2001) Robots in laparoscopic surgery. J Laparoendosc Adv Surg Tech A 11:415–419
Fourman MM, Saber AA (2012) Robotic bariatric surgery: a systematic review. Surg Obes Relat Dis 8:483–488
Edelson PK, Dumon KR, Sonnad SS, Shafi BM, Williams NN (2011) Robotic vs. conventional laparoscopic gastric banding: a comparison of 407 cases. Surg Endosc 25:1402–1408
Hubens G, Balliu L, Ruppert M, Gypen B, Van Tu T, Vaneerdeweg W (2008) Roux-en-Y gastric bypass procedure performed with the da Vinci robot system: is it worth it? Surg Endosc 22:1690–1696
Snyder BE, Wilson T, Leong BY, Klein C, Wilson EB (2010) Robotic-assisted Roux-en-Y Gastric bypass: minimizing morbidity and mortality. Obes Surg 20:265–270
Ayloo SM, Addeo P, Buchs NC, Shah G, Giulianotti PC (2011) Robot-assisted versus laparoscopic Roux-en-Y gastric bypass: is there a difference in outcomes? World J Surg 35:637–642
Park CW, Lam EC, Walsh TM, Karimoto M, Ma AT, Koo M, Hammill C, Murayama K, Lorenzo CS, Bueno R (2011) Robotic-assisted Roux-en-Y gastric bypass performed in a community hospital setting: the future of bariatric surgery? Surg Endosc 25:3312–3321
Germain A, Reibel N, Brunaud L (2011) Totally robotic gastric bypass. J Visc Surg 148:e267–e272
Markar SR, Karthikesalingam AP, Venkat-Ramen V, Kinross J, Ziprin P (2011) Robotic vs. laparoscopic Roux-en-Y gastric bypass in morbidly obese patients: systematic review and pooled analysis. Int J Med Robot 7:393–400
Hagen ME, Pugin F, Chassot G, Huber O, Buchs N, Iranmanesh P, Morel P (2012) Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg 22:52–61
Vilallonga R, Fort JM, Gonzalez O, Caubet E, Boleko A, Neff KJ, Armengol M (2012) The initial learning curve for robot-assisted sleeve gastrectomy: a surgeon’s experience while introducing the robotic technology in a Bariatric Surgery Department. Minim Invasive Surg 2012:347131
Vilallonga R, Fort JM, Caubet E, Gonzalez O, Armengol M (2013) Robotic sleeve gastrectomy versus laparoscopic sleeve gastrectomy: a comparative study with 200 patients. Obes Surg 23:1501–1507
Romero RJ, Kosanovic R, Rabaza JR, Seetharamaiah R, Donkor C, Gallas M, Gonzalez AM (2013) Robotic sleeve gastrectomy: experience of 134 cases and comparison with a systematic review of the laparoscopic approach. Obes Surg 23:1743–1752
Rezvani M, Sucandy I, Antanavicius G (2013) Totally robotic stapleless vertical sleeve gastrectomy. Surg Obes Relat Dis 9:e79–e81
Disclosure
Drs. Juan Toro, Edward Lin, and Ankit Patel have no conflicts of interest or financial ties to disclose.
Funding
There is no funding for this publication.
Conflict of interest
There is no conflict of interest for all authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is not based on any previous presentation.
Rights and permissions
About this article
Cite this article
Toro, J.P., Lin, E. & Patel, A.D. Review of robotics in foregut and bariatric surgery. Surg Endosc 29, 1–8 (2015). https://doi.org/10.1007/s00464-014-3646-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3646-z