Abstract
Introduction
Transanal endoscopic microsurgery (TEM) was first published by the late Professor Buess in 1983. The procedure initially had a slow acceptance due to its perceived difficulty, the cost of the equipment, and limited indications. However, the widespread adoption of laparoscopic colorectal surgery provided an impetus to increase the penetration of the platform. The purpose of this study was to evaluate the TEM learning curve (LC).
Methods
After institutional review board approval, all patients who underwent TEM, from November 2005 to October 2008 were identified from a prospective database. The operations were performed by a single, board-certified colorectal surgeon (DRS), after learning the technique from Professor Buess. Patient, operative, and postoperative variables were obtained by retrospective chart review. Rates of excision in minutes per cm2 of tissue were calculated. The CUSUM method was used to plot the LC. Variables were compared using χ 2 and Student’s t test. A p < 0.05 was considered significant.
Results
Twenty-three patients underwent TEM (median age 61 years, 69.5 % male). Mean operative time was 130.5 (range 39–254) min, and the mean specimen size was 16.6 (7.4–42) cm2. Average rate of excision (ARE) was 8.9 min/cm2. A stabilization of the LC was observed after the first four cases, showing an ARE of 13.8 min/cm2 for the first four cases versus 7.9 min/cm2 for the last 19 cases (p = 0.001). An additional rising and leveling of the LC was observed after the first 10 cases, when an increasing number of lesions located cephalad to 8 cm from the dentate line were being resected (lesions above 8 cm in the first 10 cases: 20 % vs. last 13 cases: 61 %; p = 0.04).
Conclusions
The ARE significantly declined after the first four cases. The LC for TEM is associated with a significant decrease in operative time after four cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Minimally invasive surgical techniques have been widely adapted. Significant advances have been made in the realm of laparoscopic surgery, single-port surgery, robotics, and natural orifice surgery. Similar trends have occurred in colorectal surgery, where the natural progression has been towards exploring techniques that would provide minimally invasive access to the rectum. These methods reduce the morbidity and mortality of traditional invasive surgical treatments without compromise to oncological or functional results.
Transanal endoscopic microsurgery (TEM) was first published by the late Professor Buess in 1983 in Tubingen, Germany [1]. This technique allows access and three-dimensional visualization of the entire rectum and rectosigmoid junction through special instrumentation and balanced insufflation [2]. It is associated with less morbidity than radical surgery [3–5] and better outcomes than traditional transanal excision, including improvement in visualization to achieve better resections, lower recurrence rates, and the ability to treat more proximal lesions [6].
The TEM technique is currently used in more than 400 centers around the world [7]. Despite these benefits, TEM initially had a relatively slow acceptance rate. Technical difficulties, high costs of the equipment, and the limited indications for the procedure were some of the perceived limitations. In addition, several authors have alluded to the “learning curve” (LC) associated with TEM [8–11]; however, only a few publications have objectively described this phenomenon [12].
Assessment of a LC can be accomplished in several ways. Various methods have been utilized in the monitoring a trainees’ proficiency in learning a procedure. The most common method is to assess changes in one or more measured outcomes over different time periods. The CUSUM test was originally designed to indicate when an industrial process deviates from an acceptable level of performance. With some modification, CUSUM techniques are being more frequently used in the surgical literature to enable more objective and sophisticated assessment of an individual’s performance. This tool has been utilized and proved valid in several recent studies examining the LCs of off-pump CABGs, sentinel lymph node biopsy, and J-pouch surgery [13–17]. The purpose of this study was to evaluate the LC for TEM.
Methods
After Institutional Review Board (IRB) approval, all the patients who underwent TEM at our institution between November 2005 and October 2008 were identified from an IRB-approved prospective database. All operations were performed by a single, board-certified (DRS), colorectal surgeon, who learned the technique from Professor Buess. Patient demographics and operative and postoperative variables were obtained by retrospective chart review. Operative time was recorded as time from first insertion of proctoscope to final removal of instrumentation. Tumor size was retrieved from pathology reports. All tumors were excised, sewn to specimen boards, and subsequently measured by a pathologist after formalin fixation. To account for varying sizes of specimen excision, the rates of excision in minutes per cm2 of tissue were calculated. The CUSUM method was used to plot the LC and determine the average rate of excision (ARE). Subanalysis of the LC was performed and variables were compared using χ 2 and Student’s t test. p < 0.05 was considered significant.
Description of the procedure
Rigid proctoscopy was performed in the outpatient clinic to identify the location and extent of the lesion to prepare for positioning of the patient. On the day of surgery, patients underwent general anesthesia and subsequently positioned such that the lesion was inferiorly situated. This location maximizes utilization of the operating proctoscope and instruments. The Wolf TEM Operating System® (Richard Wolf Medical Instruments Corp., Vernon Hills, IL, USA) was utilized in all cases in this series. The proctoscope was inserted and the balanced insufflation of the rectum was obtained. The tumor was then circumferentially marked with electrocautery. Depending on the previous biopsy and the depth of tumor invasion on previous rectal ultrasound, a submucosal or full-thickness incision was made circumferentially. A submucosal technique was better suited for large, extensive, high, and benign lesions involving the anterior and lateral rectum, because this technique preserves the integrity of the rectal wall and avoids peritoneal entry. Full thickness was preferentially used in those cases with a previous diagnosis of adenocarcinoma or carcinoid and when deep tumor invasion was identified. If a submucosal dissection was undertaken, saline/epinephrine solution was injected into the submucosal plane to elevate and aid in dissection. All defects were closed with running PDS and locking beads; the procedure and instrumentation have been described in greater detail in the literature [18].
Results
Twenty-three patients underwent TEM (median age 61 years, 69.5 % male). The surgical indications for the procedure were dysplasia in 17 (73.9 %), adenocarcinoma (pT1 2, pT2 1; N0) in 3 (13 %), carcinoid in 2 (8.7 %), and lipoma in 1 (4.3 %).
Lesions were located in the lateral (39 %), posterior (36 %), and anterior (25 %) walls of the rectum, with a mean distance from the anal verge of 8 (range 3–14) cm. The mean operative time was 130.5 (range 39–254) min, and the mean specimen size was 16.6 (range 7.4–42) cm2 with a 4 % incidence of specimen fragmentation. Margin status was histopathologically assessed and reported in all cases. As a standard, benign and malignant lesions were marked out 5 and 10 mm, respectively, for planned resection. Negative margins of resection were achieved in 86.9 % of cases. Procedure-related complications (13 %) included urinary retention, temporary neuropraxia, and spontaneously resolving diarrhea. No major complications were identified. The mean length of hospitalization was 1.8 (range 1–5) days.
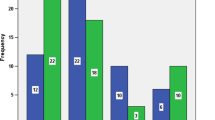
Recurrence was identified in only one case (4.3 %) at a mean follow-up of 26 (range 1–70) months. The ARE was 13.9 min/cm2 for the first four cases versus 7.9 min/cm2 for the last 19 cases (p = 0.001). Figure 1 demonstrates a logarithmic trend line showing a steep decline in the rate of excision over the first four cases, followed by a relative leveling off of the slope of the curve during the ensuing cases. An additional rising and leveling of the ARE was observed after the first 10 cases, when more lesions located above 8 cm from the dentate line were being resected using this technique (lesions cephalad 8 cm in the first 10 cases were 20 % vs. the last 13 cases at 61 %, p = 0.04; Fig. 2).
Figure 3 demonstrates the learning curve for TEM utilizing a CUSUM curve. The stabilization of the curve represents the leveling off of variability within the process and in turn ascent of the learning curve. The curve confirms the stabilization of the rate of excision after the initial 4 cases and then again after 4 more cases half way through the experience when higher lesions were approached.
Discussion
Buess et al. [19] published their early experience with TEM in 1988 in which 140 patients underwent this procedure. The average resection size was 14.4 cm2 with an average operative time of 92 min.
Since then, Saclarides published a single surgeon’s experience with TEM from 1991 to 1996 in which he operated on 73 patients. The improved visualization and optics associated with TEM led to the author’s reluctance to revert to “cumbersome conventional instruments” associated with transanal excision. There is clear evidence in the literature that TEM provides a superior local excision compared to standard transanal excision using retractors.
In their comparison of TEM versus TAE, Moore et al. [20] also identified improvements in clear margins (90 vs. 71 %, respectively), nonfragmented specimen (94 vs. 65 %, respectively), and local recurrence (5 vs. 27 %, respectively). However, they did find that there was a similar distant recurrence rate of 1 and 4 %, respectively.
Several studies have been published comparing TEM to both TAE and LAR with TME in a variety of disease states, from benign tumors to T2 rectal adenocarcinoma. Most studies discuss the safety of TEM and endorse its use in the treatment of large polyps that are endoscopically irretrievable, other benign lesions, or patients in whom radical resection is either refused or contraindicated (Table 1).
De Graaf et al. [21] investigated the feasibility of TEM for the treatment of rectal adenomas. They prospectively evaluated 353 consecutive rectal adenomas. The conversion rate correlated with the distance from the anal verge (p = 0.07) and the operative surgeon’s level of experience. The median operative time was 45 min and correlated with the specimen area, experience, and operating surgeon (p < 0.001). Rectal adenomas with incomplete margins were larger and located more proximally (p < 0.001). Resection margin status was a predictor of recurrence (p < 0.001). They concluded that TEM is safe, feasible, and yields excellent results in almost all adenomas.
The data relative to the use of TEM in the treatment of rectal malignancy generate much more controversy. Initially, most of the published literature consisted of single surgeon retrospective reviews of treatment of T1 cancers (Table 2).
With the mounting enthusiasm towards minimally invasive surgery, promising prospectively randomized studies have been published endorsing the use of TEM for treatment of more advanced rectal cancers. Lezoche et al. compared TEM to LAR with TME in patients with T2 tumors who had undergone preoperative chemoradiation. There were statistically significant improvements in the operative time and blood loss. During a median follow-up of 84 months, TEM and LAR had local recurrence rates of 5.7 and 2.8 %, respectively, and the probability of disease-free survival at the end of the follow-up period was 94 % in both groups [22].
Stipa et al. [23] investigated the management of local recurrence after TEM and evaluated the long-term outcome. A total of 144 patients who underwent TEM for the treatment of rectal carcinoma were included in the study, 44 patients had local or distal recurrence, or both. Overall 5-year survival was 83 % in all 144 patients and 92 % in patients with pT1 tumors. The overall 5-year survival rate was higher in patients who had a radical salvage procedure than in those who had transanal reexcision (69 vs. 43 %; p = 0.05). They concluded that the outcome after transanal excision for rectal cancer depends on close surveillance for early detection of recurrence.
Endoluminal or pelvic recurrence should be treated with an immediate radical salvage operation. Overall long-term survival after local excision with TEM followed by radical salvage surgery for local recurrence is comparable to overall survival after initial radical surgery. In our series, no mortality was observed and the recurrence rate was 4.3 % during a mean follow-up period of 26 months.
Tsai et al. [24] have reviewed their experience with TEM in order to clarify its role in the treatment of different types of rectal pathology. They concluded that TEM can be offered for curative resection of benign tumors, carcinoid tumors, and selected T1 adenocarcinoma, histopathologic staging in indeterminate cases, and for palliative resection in patients medically unfit or unwilling to undergo radical resection.
Complication rates have been widely reported, depending on the inclusion (or exclusion) of minor complications. Kreissler-Haag et al. [10] assessed the anatomical variables of rectal neoplasia as well as surgeon experience on postoperative complications in patients undergoing TEM. They reported a 0.3 % incidence of mortality and a 9 % overall complication rate that included bleeding, fecal incontinence, dysuria, pneumonia, myocardial infarction, and pulmonary emboli. Overall surgical complications as well as bleeding did not correlate with the number of TEM procedures performed, suggesting a short LC for the procedure in surgeons with previous experience in minimally invasive surgery. However, complications did correlate with tumors located more than 8 cm cephalad from the anal verge, especially when laterally located. In our series, complications included urinary retention, temporary neuropraxia, and self-limited diarrhea; no reoperations were required.
Doonerbosch et al. [25] assessed the functional outcome and quality of life after TEM. A total of 47 patients were studied before and at least 6 months after TEM. Functional outcome was determined using the Fecal Incontinence Quality of Life (FIQoL) score. They concluded that TEM has no detrimental effect on fecal continence, and once the tumor has been excised, quality of life is improved. In our series, no complications related to fecal continence were observed.
The combination of increasing interest in minimally invasive techniques and the favorable outcomes reported for this technique has led to a surge in curiosity regarding TEM in the colorectal surgical community. One of the barriers to widespread acceptance of the technique has been the perceived steep LC. Koebrugge et al. [12] presented their initial results of whether experience influences outcome after TEM. They concluded that there was significant reduction in operative time, total length of hospital stay, and complication rate over the years.
As stated earlier, the CUSUM method has been increasingly used to assess competence in certain surgical techniques. Lim et al. [26] researched doctors’ performances in several scenarios and described a flattening of the CUSUM curve associated with learning and increasing skillfulness with a particular technique. In our study, a stabilization of the CUSUM curve, indicating increasing skillfulness with TEM after four cases was demonstrated. In addition, a second upward slope as more proximal and challenging tumors were being excised was noted. This was followed by a second leveling off of the CUSUM curve indicating increasing skillfulness with the technique with more challenging lesions.
Conclusions
This study describes a single surgeon’s early experience with TEM and the relative ease of adoption into one’s surgical practice. Ascent of the LC for TEM appears to be easily achieved.
References
Buess G, Theiss R, Gunther M, Hutterer F, Pichlmaier H (1985) Endoscopic surgery in the rectum. Endoscopy 17(1):31–35
Buess G, Mentges B, Manncke K, Starlinger M, Becker HD (1992) Technique and results of transanal endoscopic microsurgery in early rectal cancer. Am J Surg 163:63–70
Lee W, Lee D, Choi S, Chun H (2003) Transanal endoscopic microsurgery and radical surgery for T1 and T2 rectal cancer. Surg Endosc 17:1283–1287
Langer C, Liersch T, Suss M et al (2003) Surgical cure for early rectal carcinoma and large adenoma: transanal endoscopic microsurgery (using ultrasound or electrosurgery) compared to conventional local and radical resection. Int J Colorectal Dis 18:222–229
Winde G, Nottberg H, Keller R et al (1996) Surgical cure for early rectal carcinomas (T1): transanal endoscopic microsurgery vs. anterior resection. Dis Colon Rectum 39:969–976
Neary P, Makin GB, White TJ et al (2003) Transanal endoscopic microsurgery: a viable operative alternative in selected patients with rectal lesions. Ann Surg Oncol 10(9):1106–1111
Saclarides TJ (2007) TEM/local excision: indications, techniques, outcomes, and the future. J Surg Oncol 96:644–650
Saclarides T (1998) Transanal endoscopic microsurgery: a single surgeon’s experience. Arch Surg 133(6):595–598 (discussion 598–599)
Smith LE, Ko ST, Saclarides T, Caushaj P, Orkin BA, Khanduja KS (1996) Transanal endoscopic microsurgery: initial registry results. Dis Colon Rectum 39(10 Suppl):S79–S84
Kreissler-Haag D, Schuld J, Lindemann W, Konig J, Hildebrandt U, Schilling M (2008) Complications after transanal endoscopic microsurgical resection correlate with location of rectal neoplasms. Surg Endosc 22(3):612–616
Porcher R, Nizard RS, Schlup MM et al (2008) Quantitative and individualized assessment of the learning curve using LC-CUSUM. Br J Surg 95(7):925–929
Koebrugge B, Bosscha K, Ernst MF (2009) Transanal endoscopic microsurgery for local excision of rectal lesions: is there a learning curve? Dig Surg 26(5):372–377
Watters DA, Colson ME, Yap C (2007) Cumulative sum techniques for surgeons: a brief review. ANZ J Surg 77(7):583–586
Wan F, Chen Y (2009) Off-pump coronary artery bypass graft surgery: a training course for novices and its learning curve. Thorac Cardiovasc Surg 57(3):141–147
Blake GO, Kanchev E, Valentine CS et al (2009) Sentinel lymph node biopsy for breast cancer using methylene blue dye manifests a short learning curve among experienced surgeons: a prospective tabular cumulative sum (CUSUM) analysis. BMC Surg 27(9):2
Colquhoun PH (2008) CUSUM analysis of J-pouch surgery reflects no learning curve after board certification. Can J Surg 51(4):296–299
Tekkis PP, Fazio VW, Laveri IC et al (2005) Evaluation of the learning curve in ileal pouch-anal anastomosis surgery. Ann Surg 241(2):262–268
Cataldo P (2006) Transanal endoscopic microsurgery. Surg Clin North Am 86(4):915–925
Buess G, Kipfmuller K, Ibald R et al (1988) Clinical results of transanal endoscopic microsurgery. Surg Endosc 2(4):245–250
Moore JS, Cataldo P, Osler T, Hyman N (2008) Transanal endoscopic microsurgery is more effective than traditional transanal excision for resection of rectal masses. Dis Colon Rectum 51(7):1026–1030 (discussion 1030–1031)
De Graaf EJR, Doornebosch PG, Tetteroo GWM, Geldof H, Hop WCJ (2009) Transanal endoscopic microsurgery is feasible for adenomas throughout the entire rectum: a prospective study. Dis Colon Rectum 52:1107–1113
Lezoche G, Baldarelli M, Paganini M et al (2008) A prospective randomized study with a 5-year minimum follow-up evaluation of transanal endoscopic microsurgery versus laparoscopic total mesorectal excision after neoadjuvant therapy. Surg Endosc 22(2):352–358
Stipa F, Giaccaglia V, Burza A (2012) Management and outcome of local recurrence following transanal endoscopic microsurgery for rectal cancer. Dis Colon Rectum 55:262–269
Tsai BM, Finne CO, Nordenstam JF, Christoforidis D, Madoff R, Mellgren A (2010) Transanal endoscopic microsurgery of rectal tumors: outcomes and recommendations. Dis Colon Rectum 53:16–23
Doornebosch PG, Gosselink MP, Neijenhius PA, Schouten WR, Tollenaar RAEM, de Graaf EJR (2008) Impact of transanal endoscopic microsurgery on functional outcome and quality of life. Int J Colorectal Dis 23(7):709–713
Lim TO, Soraya A, Ding LM, Morad Z (2002) Assessing doctors’ competence: application of CUSUM technique in monitoring doctors’ performance. Int J Qual Health Care 14(3):251–258
Mentges B, Buess G, Schäfer D, Manncke K, Becker HD (1996) Local therapy of rectal tumors. Dis Colon Rectum 39(8):886–892
Mörschel M, Heintz A, Bussmann M, Junginger T (1998) Follow-up after transanal endoscopic microsurgery or transanal excision of large benign rectal polyps. Langenbecks Arch Surg 383(5):320–324
Nagy A, Kovács T, Berki C, Jánó Z (1999) Surgical management of villous and tubulovillous adenomas of the rectum. Orv Hetil 140(40):2215–2219
Buess GF, Raestrup H (2001) Transanal endoscopic microsurgery. Surg Oncol Clin North Am 10(3):709–731
Lloyd GM, Sutton CD, Marshall LJ et al (2002) Transanal endoscopic microsurgery—lessons from a single UK centre series. Colorectal Dis 4(6):467–472
Palma P, Freudenberg S, Samel S, Post S (2004) Transanal endoscopic microsurgery: indications and results after 100 cases. Colorectal Dis 6(5):350–355
Platell C, Denholm E, Makin G (2004) Efficacy of transanal endoscopic microsurgery in the management of rectal polyps. J Gastroenterol Hepatol 19(7):767–772
Endreseth BH, Wibe A, Svinsãs M, Mãrvik R, Myrvold HE (2005) Postoperative morbidity and recurrence after local excision of rectal adenomas and rectal cancer by transanal endoscopic microsurgery. Colorectal Dis 7(2):133–137
Whitehouse PA, Tilney HS, Armitage JN, Simson JN (2006) Transanal endoscopic microsurgery: risk factors for local recurrence of benign rectal adenomas. Colorectal Dis 8(9):795–799
Langer C, Markus P, Liersch T, Füzesi L, Becker H (2001) Ultracision or high-frequency knife in transanal endoscopic microsurgery (TEM)? Advantages of a new procedure. Surg Endosc 15(5):513–517
Demartines N, Von Flüe MO, Harder FH (2001) Transanal endoscopic microsurgical excision of rectal tumors: indications and results. World J Surg 25(7):870–875
Stipa F, Burza A, Lucandri G et al (2006) Outcomes for early rectal cancer managed with transanal endoscopic microsurgery: a 5-year follow-up study. Surg Endosc 20(4):541–545
Floyd ND, Saclarides TJ (2006) Transanal endoscopic microsurgical resection of pT1 rectal tumors. Dis Colon Rectum 49(2):164–168
Baatrup G, Breum B, Qvist N et al (2009) Transanal endoscopic microsurgery in 143 consecutive patients with rectal adenocarcinoma: results from a Danish multicenter study. Colorectal Dis 11(3):270–275
Disclosures
Andrew Vorenberg: Davinci Surgery, Intuitive Surgical. Steven Wexner receives consulting fees and royalties from Karl Storz Endoscopy. Antonio Maya, Myrian Oviedo, Giovanna DaSilva, and Dana Sands have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maya, A., Vorenberg, A., Oviedo, M. et al. Learning curve for transanal endoscopic microsurgery: a single-center experience. Surg Endosc 28, 1407–1412 (2014). https://doi.org/10.1007/s00464-013-3341-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3341-5