Abstract
Background
It is still unknown to what extent the reported morbidity and recovery benefits of laparoscopic total abdominal colectomy (TAC) for severe ulcerative colitis (UC) are associated with patient selection bias. This study aimed to evaluate whether laparoscopic TAC has any advantages over open surgery after control for perioperative confounding factors.
Methods
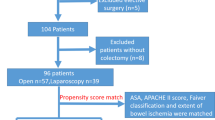
Patients undergoing TAC for UC during 2006–2010 were identified. Demographics, disease characteristics, and perioperative outcomes were compared between laparoscopic and open TAC. Postoperative recovery and 30-day complications were further assessed by covariate-adjusted multivariate regression models. The outcomes of different laparoscopic techniques were compared. A subgroup analysis including surgeons who routinely used both laparoscopic and open techniques was also performed.
Results
Of the 412 eligible patients, the 197 patients undergoing laparoscopic TAC were significantly younger and had a decreased Charlson Comorbidity Index and ASA score, increased hemoglobin and serum albumin levels, and a smaller proportion of extensive colitis and urgent cases. Unadjusted analyses showed that intraoperative morbidity, postoperative mortality, and rates for readmission and reoperation were similar. Laparoscopic TAC was associated with a longer operative time but a decrease in blood loss, overall morbidity, ileus, and thromboembolism, as well as a faster return to bowel function and a shorter hospital stay. After covariate adjustments, laparoscopic surgery remained associated with a reduction in the time to stoma function, incidence of postoperative ileus, and hospital stay compared with open TAC. The rates of postoperative morbidity, readmission, and reoperation did not differ regardless whether the conventional multitrocar technique, hand-assisted procedure, or single-incision technique was used. Laparoscopic TAC among surgeons using both open and laparoscopic techniques was associated with recovery benefits similar to those observed in the overall study population.
Conclusion
The data suggest that laparoscopic TAC retains recovery advantages over open surgery even after adjustments for confounders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred standard of care in the surgical treatment of ulcerative colitis (UC). However, when the general condition of the patient is poor due to factors such as malnutrition, anemia, and immunosuppression [1], an immediate restorative proctocolectomy is not desirable, and the recommended initial approach is instead total abdominal colectomy with end ileostomy (TAC) [2]. In addition, TAC more recently has been proposed as the initial surgical approach for patients who had treatment with infliximab within the last 12 weeks before surgery because of the increase in septic complication rates after restorative proctocolectomy [3, 4].
During the past decade, a number of comparative studies have indicated that laparoscopic TAC is a safe and feasible alternative to open TAC for selected patients [5–12]. However, considering the complexity of the minimally invasive approach, a selection bias among patients suitable for laparoscopic versus open surgery may be possible, with open surgery preferentially offered to patients who have anticipated technical difficulties or higher surgical risks.
In the absence of a randomized controlled trial comparing outcomes, it is therefore still unclear to what extent the reported morbidity and recovery benefits are genuine advantages of laparoscopic TAC over its open counterpart rather than the results of patient selection bias. For example, an open TAC remains generally recommended for treating the most severe presentations of UC, especially in case of life-threatening complications including toxic megacolon, free perforation, and massive hemorrhage [2]. Because it is expected that patients with more severe disease still may be offered open surgery, this study aimed to evaluate whether laparoscopic TAC still has advantages over open TAC for severe UC when control is used for comorbidity, disease severity, and other such potential confounders.
Methods
Patients and clinical variables
All adult patients who underwent TAC for UC or indeterminate colitis during 1998–2010 were identified by International Classification of Disease, 9th edition (ICD-9) diagnosis and Current Procedural Terminology (CPT)-4 procedure codes. Colitis complicated by toxic megacolon, massive hemorrhage, or colonic perforation was excluded from the study.
Patient characteristics, perioperative variables, and short-term postoperative outcomes were retrospectively collected by chart review. Preexisting medical comorbidity rates were determined by calculating the age-adjusted Charlson Comorbidity Index (CCI) score [13]. The definition of severe colitis was based on Truelove and Witts [14] criteria and required more than six bowel movements per day with bloody diarrhea plus any one of the following items: temperature higher than 37.5 °C, heart rate faster than 90 beats per minute, and hemoglobin level lower than 10.5 g/dl [15]. Severe acute colitis was defined as an acute episode of severe colitis requiring hospitalization. Extensive colitis was defined as disease extending proximally to the splenic flexure.
Steroid use was defined as corticosteroids administered within 1 month before TAC. High-dose steroid exposure was defined as intravenous methylprednisolone administration or oral prednisone at a dose of 40 mg or more per day [16]. Immunosuppressive use was defined as azathioprine (AZA) or 6-mercaptopurine (6-MP) administration within 2 months before TAC. Antitumor necrosis factor (TNF) monoclonal antibody use was defined as at least one infusion of infliximab within 12 weeks after TAC [17] or current treatment at the time of TAC surgery with either adalimumab or certolizumab pegol, which were used off-label for 12 and 2 patients, respectively.
Elective TAC was defined as an operation performed for a patient on the day of admission. Urgent TAC was instead defined as an operation performed for an otherwise already hospitalized patient after failure of maximal medical treatment. Conversion was defined as the need for laparotomy to accomplish anything other than specimen extraction or extension of the incision used for placement of the hand-assist device to complete the surgical procedure [18].
Operative time was calculated from skin incision to wound closure. Return of bowel function was defined as the passage of flatus or stool into the ileostomy appliance. Postoperative morbidity and mortality were defined as those occurring within 30 days after TAC or during the same hospital stay. Morbidity was calculated based on the number of patients who experienced at least one complication. Hospital readmission was determined as previously reported [19].
The definitions of specific complications after TAC used at our institution have been previously described [20]. (Colo)rectal stump leak was defined as either radiologic leakage or purulent or feculent discharge from the area in which the stump was placed associated with visible mucosa at physical examination. Early postoperative bowel obstruction (EPSBO) was defined based on obstructive symptoms associated with radiographic findings consistent with mechanical intestinal obstruction occurring within the first 30 days after surgery [21]. Ileus was defined as absence of bowel function on postoperative day (POD) 5 or the need for insertion of a nasogastric tube because of abdominal distension, nausea, and emesis after the start of a liquid diet in the absence of a mechanical bowel obstruction detected by imaging studies or at the time of reoperation. Wound infection was defined as purulent drainage from a surgical wound in the absence of stump leak or clinical signs of infection requiring deliberate opening of the wound or antibiotic treatment, excluding wounds that were opened but without microorganisms identified by wound culture.
Surgical technique and postoperative care
The laparoscopic and open surgical techniques used for the patients in the current study have been described previously [22]. The decision for a particular operative technique (open or laparoscopic) was left to the discretion of the individual operating surgeon. Cases treated with single-incision laparoscopic surgery were managed through the opening used to create the end ileostomy by an approach similar to that described for single-incision total proctocolectomy [23].
After mobilization of the colon, a decision was made either to preserve the rectum as a Hartmann stump or to leave a longer rectosigmoid stump whose stapled tip was to be brought up into the subcutaneous tissue of the extraction site. Enhanced-recovery protocols were used after both laparoscopic and open procedures as previously described [24, 25]. Alvimopan was not administered in either study group.
Statistical analysis
Quantitative variables were summarized as mean ± standard deviation or as median and range. Categorical variables were summarized as frequency or “percentage. For univariate analysis, Fisher’s exact probability test, the Chi square test, or the Wilcoxon rank sum test were used as appropriate, and P values lower than 0.05 were considered statistically significant.
For age at surgery and body mass index (BMI), model parameter and odds ratio estimates corresponded to a 5-year or 5-kg/m2 increase. For American Society of Anesthesiology (ASA) level and age-adjusted CCI, model parameter and odds ratio estimates corresponded to a 1-U increase. For hemoglobin and albumin, estimates corresponded to a 1 g/dl decrease.
Covariate-adjusted associations between surgery type and outcomes were performed using multivariable logistic regression or multivariable linear regression models. We applied a log2 transformation to the continuous outcomes to achieve approximate normality. Associations were measured by outcome ratios for open surgery relative to laparoscopic surgery, which we defined as odds ratios for yes/no morbidity outcomes and the multiplicative increase in the median for continuous outcomes.
Multivariable linear regression models were built for the following continuous outcomes: estimated blood loss, operative time, return of stoma function, and hospital length of stay. Multivariable logistic regression models were also built for morbidity outcomes including overall morbidity, ileus, wound infection, and thromboembolic complications.
Covariates statistically significant at the 0.05 level were selected based on the results of univariate analysis. Preoperative medical treatment using one or a combination of high-dose steroids, immunosuppressives, or biologics within 1 month before colectomy was also selected for its clinical significance. Ileus, wound infection, and thromboembolic complications had too few events to support a large set of covariates, so final covariates for their logistic regression models were selected by a forward selection with a cutoff of P lower than 0.20.
Results
The study identified 412 consecutive patients who underwent TAC for UC/indeterminate colitis performed by 18 staff surgeons in this institution between 2006 and 2010. For 197 of these patients (48 %), laparoscopic TAC was performed. The patients undergoing open TAC were significantly older and had a higher age-adjusted CCI, a higher ASA classification, and a higher BMI than their laparoscopic counterparts (Table 1).
The percentage of obese patients (BMI ≥30 kg/m2) undergoing surgery via an open approach was significantly higher than in the laparoscopic group (28 vs. 17 %; P = 0.006). In addition, open TAC was significantly associated with decreased hemoglobin levels, hypoalbuminemia, and extensive colitis. On the other hand, the two groups did not differ significantly in terms of other preoperative parameters reflecting disease severity such as stool frequency, body temperature, or pulse, nor in preoperative medical treatments (Table 1).
With respect to perioperative outcomes as shown in Table 2, a significantly increased proportion of open TACs were performed urgently. The majority (94 %) of open TACs were associated with subcutaneous implantation of the rectosigmoid stump, whereas nearly half of the defunctionalized stumps were placed intraperitoneally as a Hartmann pouch in the laparoscopic group. Laparoscopic TAC required a longer operative time and was associated with significantly less estimated blood loss than open TAC. One patient in the laparoscopic group died postoperatively due to acute myocardial infarction, whereas two deaths occurred in the open group due to multiple organ failure and acute pulmonary embolism, respectively.
No significant differences in intraoperative morbidity, reoperation, or readmission rates were found between the two groups. However, both the median time to stoma function and the median postoperative hospital length of stay were significantly shorter after laparoscopic TAC (2 vs. 3 days, P < 0.001 and 4 vs. 7 days, P < 0.001, respectively). Unadjusted univariate analysis showed that overall postoperative morbidity, ileus, and thromboembolic complications were significantly increased after open TAC. An increased wound infection rate also was observed after open TAC, but the P value did not reach statistical significance.
Next, covariate-adjusted multivariate analyses to verify the associations between surgery type and outcomes were performed with significantly different outcome variables, including age at colectomy, BMI, ASA level, age-adjusted CCI, hemoglobin, serum albuminemia, extent of colitis, urgency of the operation, and (colo)rectal stump management (implantation of the rectosigmoid stump in the subcutaneous tissue vs the Hartmann stump).
After multivariate analysis, the covariate-adjusted outcome ratios confirmed significantly increased operative times after laparoscopic TAC but also significantly reduced time to ileostomy function, incidence of ileus, and hospital stay. Blood loss and overall morbidity were similar. The covariate-adjusted odds of ileus (with ASA level as a covariate) still was significantly higher for the open TAC patients, whereas the covariate-adjusted odds of thromboembolic complications (with extent of colitis, hemoglobin, and urgency of the operation as covariates) indicated a marginally increased risk after open TAC, although statistical significance at the 0.05 level was not reached (Table 3). Consideration of all 197 laparoscopic cases showed no differences in the rates of postoperative morbidity, readmission, or reoperation regardless whether conventional multi-trocar, hand-assisted, or single-incision technique was used (Table 4).
We performed further analyses to address the possible effect of the selection bias on outcomes of the laparoscopic versus the open approach. In particular, 6 of the 18 staff surgeons performed only open TAC for a total of 117 patients. On the other hand, 4 surgeons performed only laparoscopic TAC for a total of 6 patients. The remaining 8 surgeons operated on the remainder of the patients using various proportions of either laparoscopic or open techniques.
The surgeons who used both laparoscopic and open approaches (with experience of at least 5 cases of each) and had managed more than 25 cases altogether were discretionally included in a subgroup analysis. Of all 412 patients, 38.8 % (160 cases including 93 laparoscopic and 67 open cases) were managed by three surgeons, with surgeon 1 managing 56 laparoscopic and 48 open cases, surgeon 2 managing 21 laparoscopic and 9 open cases, and surgeon 3 managing 16 laparoscopic and 10 open cases. Of those 93 laparoscopic cases, 72 (77 %) were managed with a multiport laparoscopic approach and 21 (23 %) with a hand-assisted approach. The conversion rate was 9.7 %.
As shown in Table 5, most of the preoperative differences between the laparoscopic and open groups in this subset of patients could still be observed except for hemoglobin levels, extent of colitis, and proportion of patients receiving high-dose preoperative steroids. Perioperative outcomes including blood loss, operative time, return of stoma function, and postoperative hospital stay were still significantly different after univariate analysis. However, the differences in wound infection rates did not quite reach statistical significance, and the overall morbidity rate, ileus, and thromboembolic complications also were similar between the two groups.
Multivariable linear regression models were built for estimated blood loss, operative time, return of stoma function, and hospital length of stay. Eight covariates including age at surgery, BMI, ASA level, smoking status, age-adjusted CCI, urgency of the operation, management of the rectal stump, and preoperative medical treatment were selected based on univariate analyses and clinical significance as described previously. Similar results were found, as shown in Table 6.
Discussion
After adjustment for the degree of patient comorbidity and other inherent differences between the groups, our data confirmed the recovery benefits of laparoscopic TAC for UC. The recovery benefits are corroborated by the subset analysis of patients whose operations were performed by surgeons using both laparoscopic and open techniques. However, the advantage in reduced postoperative complications was obviously influenced by the healthier condition of the patients treated laparoscopically.
To our knowledge, this is the first and largest study to date that objectively evaluated the benefits of laparoscopic TAC for severe UC after controlling for confounding factors. The overall morbidity rates of the current study are similar to the aggregate morbidity rates from a recent metaanalysis, which reported rates of almost 40 % for laparoscopic and 68 % for and open TAC [26].
As suggested earlier, the current study, unlike other studies, did not show any advantages in overall morbidity associated with laparoscopic TAC after confounder adjustment [10, 11]. We believe that this primarily depended on the covariate-adjusted analyses that constituted the core of this study, specifically aimed at correcting the effect of comorbidity in comparing the two surgical approaches. However, it also might have depended partially on this study’s exclusion of patients with the most severe complications of UC (toxic megacolon, massive hemorrhage, and perforation), which still are treated with the open technique.
Notably, the absolute incidences of wound infection and thromboembolic events after laparoscopic TAC were reduced by half and two-thirds compared with open TAC, indicating specific benefits deriving from the laparoscopic approach, as reported from previous studies [27–29]. However, multivariate analysis failed to confirm such advantages of laparoscopic TAC, thus implying that perioperative confounders did contribute to the morbidity benefits of laparoscopic TAC.
Our study confirmed recovery advantages after laparoscopic TAC, as reported in previous studies without covariate adjustments [10, 11] but with a larger sample and maximal control of confounding factors. Notably, unlike some of the previous reports, postoperative length of stay rather than total length of hospital stay was used in this study, [6, 10], which we believe more specifically reflected surgical outcomes than the preoperative disease course. In particular, the risk for the development of ileus after open TAC was nearly five times higher than after laparoscopic TAC even with confounder adjustment.
Although a reduction in ileus and general bowel dysfunction has been reported after laparoscopic colectomy compared with open technique [30], the difference for this particular indication when control was used for other factors, seems to be even more remarkable. Future studies are needed to confirm the magnitude of the reduction in the rate of postoperative ileus specifically associated with laparoscopic TAC.
Our series was purposefully focused on patients whose operation was performed after laparoscopic TAC had gained acceptance and was widely practiced in our unit. It is therefore notable that more than half of our consecutive patients still underwent open surgery. A variety of reasons can explain this finding. First, a number of unfavorable factors such as older age, comorbidities, extensive colitis, and urgent surgery, often regarded as contraindications for laparoscopic surgery [1, 31], restrained surgeons from more liberally using minimally invasive techniques. This practice is, however, facing increasing challenges from developments in technology, advancements in surgical techniques, and accumulation of experience [32, 33], which could further increase our proportion of laparoscopic TACs performed in the future.
An additional factor explaining the prevalence of open surgery in our series is the specific surgeon mix of our unit, which is composed of individuals who use both laparoscopic and open approaches to treat their patients as well as surgeons who exclusively perform open TAC. It is therefore possible that the obvious selection bias for a particular surgical approach emerging from the analysis of our entire cohort might have been even more pronounced if all the surgeons had practiced both laparoscopic and open surgery. In any case, the subgroup analysis restricted to those surgeons who routinely performed both laparoscopic and open TAC confirmed the results based on the entire patient population.
Another significant difference between the current study and earlier reports (Table 7) is that our patient population included a significant number of elective procedures, which reflects a clinical practice shift in the indications for TAC, probably attributable to a widespread use of anti-TNF therapy. To decrease the influence of heterogeneity, both the timing of colectomy (urgent vs. elective) and the characteristics of the medical treatment preceding the decision for TAC also were used as cofactors in our multivariable analysis.
Although we carefully considered its design, this study has inevitable limitations due to its retrospective nature and inherent selection bias, which was minimized but may not have been eliminated by adjustment for potential confounders, even when all univariably different variables were included. Hence, the results should be delineated carefully. Although our data confirm the safety and feasibility of laparoscopic surgery on a larger scale, future studies are needed to assess the extent to which laparoscopic TAC can replace open TAC as the initial surgical management of severe UC and maintain its recovery benefits. However, in the absence of a randomized controlled trial comparing outcomes after laparoscopic and open TAC, considering the careful control of confounding factors that might be responsible for any differences, the current study provides the best currently available evidence indicating the advantages of the minimally invasive approach even for patients with severe UC.
References
Teeuwen PH, Stommel MW, Bremers AJ, van der Wilt GJ, de Jong DJ, Bleichrodt RP (2009) Colectomy in patients with acute colitis: a systematic review. J Gastrointest Surg 13:676–686
Cohen JL, Strong SA, Hyman NH, Buie WD, Dunn GD, Ko CY, Fleshner PR, Stahl TJ, Kim DG, Bastawrous AL, Perry WB, Cataldo PA, Rafferty JF, Ellis CN, Rakinic J, Gregorcyk S, Shellito PC, Kilkenny JW 3rd, Ternent CA, Koltun W, Tjandra JJ, Orsay CP, Whiteford MH, Penzer JR (2005) Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum 48:1997–2009
Mor IJ, Vogel JD, da Luz Moreira A, Shen B, Hammel J, Remzi FH (2008) Infliximab in ulcerative colitis is associated with an increased risk of postoperative complications after restorative proctocolectomy. Dis Colon Rectum 51:1202–1207; discussion 1207–1210
Selvasekar CR, Cima RR, Larson DW, Dozois EJ, Harrington JR, Harmsen WS, Loftus EV Jr, Sandborn WJ, Wolff BG, Pemberton JH (2007) Effect of infliximab on short-term complications in patients undergoing operation for chronic ulcerative colitis. J Am Coll Surg 204:956–962; discussion 962–953
Dunker MS, Bemelman WA, Slors JF, van Hogezand RA, Ringers J, Gouma DJ (2000) Laparoscopic-assisted vs open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): a retrospective study in 42 patients. Surg Endosc 14:911–914
Seshadri PA, Poulin EC, Schlachta CM, Cadeddu MO, Mamazza J (2001) Does a laparoscopic approach to total abdominal colectomy and proctocolectomy offer advantages? Surg Endosc 15:837–842
Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW (2001) Laparoscopic total colectomy for acute colitis: a case-control study. Dis Colon Rectum 44:1441–1445
Marceau C, Alves A, Ouaissi M, Bouhnik Y, Valleur P, Panis Y (2007) Laparoscopic subtotal colectomy for acute or severe colitis complicating inflammatory bowel disease: a case-matched study in 88 patients. Surgery 141:640–644
Ouaissi M, Lefevre JH, Bretagnol F, Alves A, Valleur P, Panis Y (2008) Laparoscopic 3-step restorative proctocolectomy: comparative study with open approach in 45 patients. Surg Laparosc Endosc Percutan Tech 18:357–362
Chung TP, Fleshman JW, Birnbaum EH, Hunt SR, Dietz DW, Read TE, Mutch MG (2009) Laparoscopic vs open total abdominal colectomy for severe colitis: impact on recovery and subsequent completion restorative proctectomy. Dis Colon Rectum 52:4–10
Watanabe K, Funayama Y, Fukushima K, Shibata C, Takahashi K, Sasaki I (2009) Hand-assisted laparoscopic vs open subtotal colectomy for severe ulcerative colitis. Dis Colon Rectum 52:640–645
Telem DA, Vine AJ, Swain G, Divino CM, Salky B, Greenstein AJ, Harris M, Katz LB (2010) Laparoscopic subtotal colectomy for medically refractory ulcerative colitis: the time has come. Surg Endosc 24:1616–1620
Kunitake H, Hodin R, Shellito PC, Sands BE, Korzenik J, Bordeianou L (2008) Perioperative treatment with infliximab in patients with Crohn’s disease and ulcerative colitis is not associated with an increased rate of postoperative complications. J Gastrointest Surg 12:1730–1736; discussion 1736–1737
Truelove SC, Witts LJ (1955) Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J 2:1041–1048
Strong SA (2010) Management of acute colitis and toxic megacolon. Clin Colon Rectal Surg 23:274–284
Colombel JF, Loftus EV Jr, Tremaine WJ, Pemberton JH, Wolff BG, Young-Fadok T, Harmsen WS, Schleck CD, Sandborn WJ (2004) Early postoperative complications are not increased in patients with Crohn’s disease treated perioperatively with infliximab or immunosuppressive therapy. Am J Gastroenterol 99:878–883
Ferrante M, D’Hoore A, Vermeire S, Declerck S, Noman M, Van Assche G, Hoffman I, Rutgeerts P, Penninckx F (2009) Corticosteroids but not infliximab increase short-term postoperative infectious complications in patients with ulcerative colitis. Inflamm Bowel Dis 15:1062–1070
Gu J, Stocchi L, Geisler DP, Kiran RP (2011) Staged restorative proctocolectomy: laparoscopic or open completion proctectomy after laparoscopic subtotal colectomy? Surg Endosc 25:3294–3299
Kiran RP, Delaney CP, Senagore AJ, Steel M, Garafalo T, Fazio VW (2004) Outcomes and prediction of hospital readmission after intestinal surgery. J Am Coll Surg 198:877–883
Kiran RP, da Luz Moreira A, Remzi FH, Church JM, Lavery I, Hammel J, Fazio VW (2010) Factors associated with septic complications after restorative proctocolectomy. Ann Surg 251:436–440
Sajja SB, Schein M (2004) Early postoperative small bowel obstruction. Br J Surg 91:683–691
Stocchi L (2010) Laparoscopic surgery for ulcerative colitis. Clin Colon Rectal Surg 23:248–258
Geisler DP, Kirat HT, Remzi FH (2011) Single-port laparoscopic total proctocolectomy with ileal pouch-anal anastomosis: initial operative experience. Surg Endosc 25:2175–2178
Delaney CP, Fazio VW, Senagore AJ, Robinson B, Halverson AL, Remzi FH (2001) “Fast track” postoperative management protocol for patients with high comorbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg 88:1533–1538
Senagore AJ, Delaney CP, Brady KM, Fazio VW (2004) Standardized approach to laparoscopic right colectomy: outcomes in 70 consecutive cases. J Am Coll Surg 199:675–679
Tan JJ, Tjandra JJ (2006) Laparoscopic surgery for ulcerative colitis: a meta-analysis. Colorectal Dis 8:626–636
Kiran RP, El-Gazzaz GH, Vogel JD, Remzi FH (2010) Laparoscopic approach significantly reduces surgical-site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211:232–238
Shapiro R, Vogel JD, Kiran RP (2011) Risk of postoperative venous thromboembolism after laparoscopic and open colorectal surgery: an additional benefit of the minimally invasive approach? Dis Colon Rectum 54:1496–1502
Aytac E, Stocchi L, Vogel J, Kiran RP (2012) The minimally invasive approach minimizes the perioperative thromboembolic and bleeding complications for patients on chronic oral anticoagulant therapy undergoing colorectal surgery. The American Society of Colon & Rectal Surgeons Annual Scientific Meeting, San Antonio, p 98
Masoomi H, Kang CY, Chaudhry O, Pigazzi A, Mills S, Carmichael JC, Stamos MJ (2012) Predictive factors of early bowel obstruction in colon and rectal surgery: data from the nationwide inpatient sample, 2006–2008. J Am Coll Surg 214:831–837
de Silva S, Ma C, Proulx MC, Crespin M, Kaplan BS, Hubbard J, Prusinkiewicz M, Fong A, Panaccione R, Ghosh S, Beck PL, Maclean A, Buie D, Kaplan GG (2011) Postoperative complications and mortality following colectomy for ulcerative colitis. Clin Gastroenterol Hepatol 9:972–980
da Luz Moreira A, Kiran RP, Kirat HT, Remzi FH, Geisler DP, Church JM, Garofalo T, Fazio VW (2010) Laparoscopic versus open colectomy for patients with American Society of Anesthesiology (ASA) classifications 3 and 4: the minimally invasive approach is associated with significantly quicker recovery and reduced costs. Surg Endosc 24:1280–1286
Makino T, Shukla PJ, Rubino F, Milsom JW (2012) The impact of obesity on perioperative outcomes after laparoscopic colorectal resection. Ann Surg 255:228–236
Disclosure
Jinyu Gu, Luca Stocchi, Feza H. Remzi, and Ravi P. Kiran have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gu, J., Stocchi, L., Remzi, F.H. et al. Total abdominal colectomy for severe ulcerative colitis: does the laparoscopic approach really have benefit?. Surg Endosc 28, 617–625 (2014). https://doi.org/10.1007/s00464-013-3218-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3218-7