Abstract
Background
This study aimed to compare the pentafecta rates between laparoscopic radical prostatectomy (LRP) and robot-assisted radical prostatectomy (RALP) and to identify prognostic factors predicting the pentafecta for each technique.
Methods
This prospective comparative study enrolled 248 consecutive male patients 70 years of age or younger with clinically localized prostate cancer [PCa: age ≤70 years, prostate-specific antigen (PSA) ≤10 ng/ml, biopsy Gleason score ≤7] who were fully continent, potent, and candidates for bilateral nerve-sparing (BNS) LRP or RALP. The pentafecta rates between LRP and RALP were compared. A logistic regression model was created to evaluate independent factors for achieving pentafecta.
Results
In the final analysis, 91 LRP and 136 RALP patients were evaluated. The median follow-up period was 21 months for the 91 LRP patients and 18 months for the 136 RALP patients (p = 0.07). Of the 227 patients, 87 reached pentafecta [25 LRP patients (27.5 %) vs 62 RALP patients (45.6 %), p = 0.006]. Of the 140 patients who failed pentafecta, 90 (64.3 %) missed a single parameter, and the difference between the groups was significant (80 % LRP vs 53.3 % RALP, p = 0.007). Lower age, lower pathologic stage, and RALP are significantly associated with pentafecta as independent factors. For the pT3 disease, the two techniques did not differ significantly.
Conclusions
Patients submitted to BNS RP have low possibilities of achieving pentafecta. Use of the robotic platform by a single surgeon significantly enhances the possibility of achieving pentafecta independently of age and pathologic stage. Potency was the most difficult outcome to reach after surgery, and it was the main factor leading to pentafecta failure. LRP and RALP provide equivalent pentafecta rates for the pT3 disease and similar “tetrafecta” outcomes when potency recovery is not included among the postoperative expectations of the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Radical prostatectomy (RP) is a recognized and validated treatment for localized prostate cancer (PCa) in patients with a life expectancy of at least 10 years [1]. In an effort to decrease the morbidity of retropubic RP, first laparoscopic radical prostatectomy (LRP) and then robot-assisted radical prostatectomy (RALP) were introduced in the field of PCa surgical treatment.
Although the risks of complications (e.g., erectile dysfunction, incontinence) and disease recurrence are well described in the published literature, it is recognized that the separate presentation of oncologic and functional results does not provide sufficient information for the patients [2, 3] and probably creates higher expectations, which may lead to higher dissatisfaction rates. Indeed, it is important to educate patients about the probability of becoming cancer free while at the same time maintaining their preoperative functional state [3].
In 2003, Salomon et al. [4] first reported the combined oncologic and functional outcome for patients undergoing RP, whereas Bianco et al. [2] coined the term “trifecta” to indicate the patients who were potent, continent, and free of prostate-specific antigen (PSA) progression after surgery. Almost 10 years have passed since the introduction of this term, but only 11 original articles have reported trifecta rates, with a mean value of 58 % (range 20–83 %) [5].
Recently Patel et al. [6] proposed the concept of “pentafecta” to provide a new and more comprehensive method for reporting outcomes after RP. In pentafecta, the early complications and the positive surgical margin (PSM) rate are included together with the three major outcomes reported in the trifecta. Patel et al. [6] reported a 12-month pentafecta rate of 70.8 % for 332 consecutive patients who underwent RALP.
However, no other study has reported on pentafecta rates, and no studies have compared pentafecta between the various approaches for the surgical treatment of PCa.
Our study aimed to compare the pentafecta rates of patients who underwent bilateral nerve-sparing (BNS) LRP and RALP by a single surgeon in a high-volume laparoscopic reference center.
Materials and methods
Patients
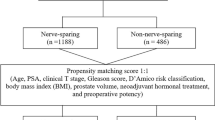
Between January 2008 and December 2010, a prospective, comparative, nonrandomized study enrolled 248 consecutive male patients 70 years of age or younger with clinically localized PCa (T1c–cT2, PSA ≤ 10 ng/ml, biopsy Gleason score ≤7) who were fully continent, potent, and candidates for BNS RP by a laparoscopic or robot-assisted approach.
The study was conducted according to the ethical principles of the Helsinki Declaration. Written informed consent was signed by each patient before enrollment began.
The study excluded patients with any grade of incontinence, erectile dysfunction (defined as 3–5 on a potency scale), history of neoadjuvant treatment for PCa, clinical or magnetic resonance imaging suspicion for locally advanced disease, PSA higher than 10 ng/ml, age exceeding 70 years, or biopsy Gleason score higher than 7 and those undergoing minimal or unilateral or non-nerve-sparing surgery.
Inclusion criteria: definitions of continence and potency
Full continence was defined the absence of any urinary leak. Patients were considered potent if they responded with a “yes” to the following question: Are you able reliably to attain an erection rigid enough for intercourse (level 1 or 2 on the rigidity scale) more than half the time? [7].
Surgical approach
The assignment of the patients to LRP or RALP was guided only by economic reasons (whether patients could afford robotic surgery or not) and not by the clinical or pathologic characteristics of the disease.
As previously described [8], both LRP (96 patients) and RALP (152 patients) were performed using essentially the same technique to control the prostatic vascular structure. This technique was a transperitoneal, antegrade, energy-free procedure using 2-mm microclips (Aesculap/B-Braun, Melsungen, Germany) with no opening of the endopelvic fascia and no use of thermocoagulation, either mono- or bipolar, at the lateral aspect of the prostate, but with preservation of the bladder neck/puboprostatic ligaments and with selective ligation of the dorsal vascular complex.
All the procedures were performed with the intent of bilateral full or partial nerve-sparing dissection involving high anterior release of the neurovascular bundles (NVBs). After the prostatectomy, no posterior or anterior reconstruction was performed. A Monocryl (3–0, Poliglecaprone 25; DemeTECH, Miami, FL, 26-mm ½ c) suture usually is used to perform the urethrovesical anastomosis. Alternatively, a 30-cm V-lock stitch (3–0, 17 mm, ½) may be used.
Postoperative care
All the patients received tadalafil 20 mg, 1 capsule, twice per week for the first 2 months after surgery and then as subjectively needed.
Histopathology report
The prostate specimens were processed with a standard whole-mount technique as described in our previous report [9].
Database
All the baseline, preoperative, inpatient, pathologic, and follow-up data were collected in a customized database.
Follow-up evaluation
After hospital discharge, every patient was counseled to undergo a serum PSA test every 3 months for the first 2 years, every 6 months for the next 3 years, and then annually. The PSA value and early complications were reported to the surgeon during the follow-up visit or by telephone.
On December 2011, a telephone interview was performed by a research fellow to assess PSA serum level, secondary treatments, continence, and capability of intercourse. The follow-up period was calculated as the temporal distance between the date of RP and the last telephone interview before the start of data analysis (December 2011). Only patients with complete follow-up data were evaluated in the final analysis.
Study end points
The primary end point of this study was a comparison of the pentafecta rates between the LRP and RALP groups. The secondary end point was identification of preoperative/prognostic factors predicting pentafecta for each technique.
Pentafecta components: definitions
The single components of pentafecta were defined as follows:
-
A surgical margin considered positive (PSM) when cancer cells were found in contact with the ink-marked resection margin and otherwise considered negative (NSM).
-
Continence, defined as no leakage or need for any protective pad.
-
Potency, as defined preoperatively (if the patient affirmed that he could get an erection firm enough for sexual intercourse, he was further asked about the use or not of PDE5-Is and the frequency of this use).
-
All medical and surgical early complications graded according to the modified Clavien–Dindo’s classification [10].
-
Biochemical recurrence (BCR), defined as a serum PSA higher than 0.2 ng/ml at two consecutive measurements [11].
Only the patients who successfully met all the aforementioned criteria were considered to have reached the pentafecta. In particular, success in reaching the pentafecta was defined as (1) absence of perioperative complications (grade 0 on the Clavien–Dindo scale) [10], (2) negative surgical margins, and (3) achievement of composite trifecta outcomes (continence, potency, and no BCR).
Justification for the number of patients
The sample size of our study was able with adequate power (1-beta > 0.80) to recognize as significant (at an alpha level of 0.05 bilaterally) large differences (>0.30) between the incidence proportions of considered outcomes. Taking into account that only one study was published about pentafecta in RALP [6] and none about pentafecta in LPR, and considering the observational nature of our study, the sample size was calculated assuming a 35 % reduction of the pentafecta rate in LPR compared with RALP. Using this criteria, at least 88 patients per group were needed.
Statistical methods
The Shapiro–Wilk test was used to evaluate normality assumptions. Student’s t test was used to compare age between groups, and the Mann–Whitney U test was used to compare PSA values. Categorical variables were compared by the Chi square test or Fisher’s exact test when necessary.
A logistic regression model was created to evaluate independent factors for achieving the pentafecta. A crude adjusted odds ratio (OR) and its 95 % confidence interval (95 % CI) were calculated. Two separate subanalyses were performed in the LRP and RALP groups to evaluate whether the influence of the parameters differed between the two groups. A p value lower than 0.05 was considered statistically significant. Stata 12.1 (StataCorp. 2011, Stata Statistical Software: Release 12; StataCorp LP, College Station, TX, USA) was used for all analyses.
Results
In the final analysis, 227 patients (91 LRP and 136 RALP) were evaluated. The study excluded 21 patients who either were lost to follow-up evaluation (15 patients) or did not receive BNS-RP for intraoperative reasons (6 patients). The median follow-up period was 21 months [interquartile range (IQR), 15–32 months] for LRP and 18 months (IQR 14–24 months) for RALP (p = 0.07).
The baseline characteristics are summarized in Table 1. Moreover, the groups did not differ significantly in terms of comorbidity, preoperative continence, or potency rates. The rates for postoperative use of phosphodiesterase type 5 inhibitors did not differ significantly between the two groups (26 vs 38 %, p = 0.126).
Outcomes
Of the 227 patients, 87 reached pentafecta [25 LRP patients (27.5 %) vs 62 RALP patients (45.6 %), p = 0.006). The trifecta rates also were significantly higher in the RALP group (58.1 vs 35.2 %, p = 0.001) (Table 2). As shown in Table 2, the single components of pentafecta differed significantly between the two groups, favoring robotics in terms of potency and continence and favoring laparoscopy in terms of NSM. A global nonsignificant trend favoring laparoscopy also was observed in terms of PSM focality and extension.
The presence of locally advanced disease exposes patients to a statistically higher risk of PSM (9.7 % for pT2 vs 25 % for pT3, p = 0.013). A PSM was significantly related to BCR both in the entire cohort (11.1 % of BCR in cases with PSM vs 1.5 % in cases without PSM, p = 0.003) and in the RALP cases (14 vs 2.6 %, p = 0.017).
Reasons of pentafecta failure: analysis (Table 3)
Of the 140 patients who did not reach pentafecta, 90 (64.3 %) missed a single parameter (Fig. 1), with no difference between the LRP and RALP groups (Fig. 2). In 66.7 % of the cases, the parameter missing was potency, and the difference between the groups was statistically significant (80 % LRP vs 53.3 % RALP, p = 0.007) (Figs. 3, 4).
A subanalysis of patients with only one parameter missing indicated that independently of the surgical technique, pT2 fails mainly due to absence of potency recovery, whereas pT3 fails due to absence of both potency recovery and NSM.
Predictive factors of pentafecta: univariate analysis
Lower age, lower pathologic stage, and RALP are significantly associated with the pentafecta (Table 4).
Multivariate logistic regression analysis (Table 5)
After adjustment for age and pathologic stage, RALP still significantly correlates with pentafecta (OR 1.9, 95 % CI 1.0–3.5, p = 0.036). After adjustment for pathologic stage and technique, age remains a significant predictive factor of pentafecta, with a 6 % reduction in the possibility of reaching this outcome for each extra year of life (OR 0.94, 95 % CI 0.9–1.0, p = 0.035). Finally, a pathologic stage pT3 reduces the probability of reaching pentafecta about 75 % after adjustment for age and technique (OR 0.24, 95 % CI 0.1–0.7, p = 0.006).
Role of age and pathologic stage in reaching pentafecta in LRP and RALP
Lower age was significantly associated with pentafecta in LRP, whereas RALP was not influenced by age. In contrast, a locally advanced disease (pT3) significantly affected pentafecta in the RALP group, whereas LRP was not influenced.
Logistic regression analysis confirmed that in LRP, age significantly affected pentafecta (OR 0.23, 95 % CI 0.06–0.84, p = 0.026), whereas pT3 did not influence the outcome (p = 0.264). On the contrary, in RALP, age did not significantly affect pentafecta (OR 0.92, 95 % CI 0.35–2.44, p = 0.869), whereas pT3 did (OR 0.2, 95 % CI 0.05–0.72, p = 0.014).
Influence of age and of pathologic stage on erectile function recovery
Older age (>65 years) negatively influenced erectile function recovery (EFR) in both the entire cohort and LRP. Independently of age, RALP significantly enhanced EFR probability (≤65 years: OR 2.29, 95 % CI 1.21–4.31, p = 0.01 vs >65 years: OR 4.6, 95 % CI 1.24–16.96, p = 0.022).
Pathologic stage pT3 did not significantly affect EFR in the entire cohort (EFR: 58 % for pT2 vs 41 % for pT3, p = 0.068) (Fig. 5). The comparison between LRP and RALP showed that for pT2 disease, RALP scored significantly better (OR 3.1, 95 % CI 1.7–5.6, p < 0.001). In contrast, for stages pT3a and higher, EFR did not differ significantly between the two techniques (OR 2.5, 95 % CI 0.6–11.0, p = 0.226).
Comparison of LRP and RALP in cases of patients not interested in EFR
When EFR was not required, the outcomes of the evaluated techniques were similar (67 vs 63 %, OR 0.85, p = 0.557). After adjustment for age, the impact of the technique on tetrafecta remained nonsignificant (OR 0.87, p = 0.643).
Discussion
Recent reviews and metaanalyses of the literature have highlighted the potential benefit of RALP compared with LRP in terms of functional outcomes [12, 13] and transfusion rates [14]. The first two controlled trials comparing LRP and RALP using a transperitoneal approach [15, 16] reported better functional results for RALP both in terms of potency [15, 16] and continence recovery [15].
Recently, Ploussard et al. [17] demonstrated in the extraperitoneal setting that robotic assistance offers better results than pure laparoscopy in terms of potency recovery and surgical margins in pathologically organ-confined disease (when strict indications of nerve-sparing techniques are respected). However, their study incorporated the outcomes of more surgeons and covered a period of about 10 years, implying that several refinements of the technique have been incorporated in the surgical practice. Moreover, both techniques were used only during the period 2007–2009, with a net predominance of pure laparoscopy before 2007 and of robotics after 2009. However, the mean follow-up period was 39 months in the LRP group and 15.4 months in the RALP group, probably influencing issues such as BCR rates and potency recovery.
Another recent single-surgeon comparative study [18] failed to identify differences between LRP and RALP in terms of safety, oncologic outcomes, and potency recovery. However, more favorable outcomes for RALP were noted in terms of operating time, pain numeric rating scale, catheter duration, and urinary continence recovery time.
All the aforementioned studies compared the two techniques in terms of isolated RP outcomes. However, because PCa is diagnosed for increasing numbers of younger and healthier men, their expectations of the surgical intervention could not be adequately addressed with separate reports of oncologic and the functional outcomes. This “fragmented” information was frequently the source of higher preoperative expectations, leading to a higher postoperative dissatisfaction rate [19].
The term “trifecta,” borrowed from horse-racing terminology, was proposed to inform the patient preoperatively on the combined possibility of his becoming free of PSA progression and experiencing continence and potency after RP [2]. Recently, a new term, “pentafecta,” was coined. Pentafecta added the early complication rate and surgical margin status to the previous variables considered in the trifecta [6] to provide more accurate counseling for patients with clinically localized PCa.
Reporting of single outcomes after LRP or RALP may be misleading with regard to the patient’s expectation for the surgical intervention. Our study primarily demonstrated that preoperatively continent and potent patients submitted to BNS-RP have low possibilities of achieving pentafecta independently of the used technique. In fact, <30 % of the patients in the LRP group and 50 % of the patients in the RALP group reached pentafecta.
In the hands of a single experienced surgeon, use of the robotic platform instead of pure laparoscopy significantly enhances the possibility of achieving pentafecta. Compared with the study of Patel et al. [6], our pentafecta rate in RALP was significantly lower (45.6 vs 70.8 %). The difference was mainly due to the EFR rate (66 vs 90 %), probably reflecting the impact of the surgical volume between surgeons with different experience in robotic surgery and suggesting a rather never-ending learning curve.
According to other studies [3, 6, 20, 21], potency was the most difficult single outcome to achieve after surgery, and it was the main factor (alone or in combination) leading to pentafecta failure with both surgical techniques, although a significant difference in favor of robotics was noted (Fig. 6). Lower age and pathologic stage as well as the use of robotics were significantly associated with the pentafecta. The results are not surprising because pathologic stage is one of the most important predictors for PSMs and BCR after RP, whereas patient age clearly is correlated with functional outcomes after surgery.
The effect of age on pentafecta and EFR is seen mainly in LRP, with patients younger than 65 years reaching significantly better results than patients older than 65 years. The same effect was not noted after RALP, which showed similar pentafecta and potency outcomes independent of patient age.
Our results suggest that for locally advanced disease (pT3), the two techniques achieve equivalent results, with no significant differences in pentafecta and potency outcomes. However, RALP enhances both pentafecta and EFR when used for pT2 disease.
The preoperative identification of patients at high risk for locally advanced disease and those not interested in EFR may be crucial to the rationale used to select the ideal candidate for each surgical technique. In these cases, the extra costs of robotics may not be justified.
To our knowledge, this is the first study to compare pentafecta outcomes of LRP and RALP, both performed by a single surgeon using similar surgical techniques. However, the following biases could affect the scientific value of our study:
-
The study was not randomized, even though the assignment of the patients to each group was not guided by the clinical or pathologic characteristics of the disease. In this regard, it must be underscored that very few surgeons adequately perform RP with different surgical approaches and that single-surgeon randomized trials, consequently, are hardly to be obtained. Thus, an adequately designed, prospective, and comparative single-surgeon trial represents a valid alternative.
-
The patients treated were from different geographic areas with respect to the treating center, so evaluation of the exact time that potency and continence recovery occurred is not known.
-
The extent of NVB dissection was determined subjectively and not by measuring the amount of nerve tissue left on the specimen.
-
Finally, no validated questionnaire was used to evaluate potency, but a good correlation between the definition of potency used in this study and the patient-derived International Index of Erectile function (IIEF) was demonstrated, with a potency scale of 1–2 corresponding to a median IIEF score of 24 or higher, to a maximum of 30 [7].
Conclusions
Continent and potent patients submitted to BNS-RP have a low possibility of achieving pentafecta independently of the surgical approach. In the hands of a single experienced surgeon, use of the robotic platform significantly enhances pentafecta, independently of age and pathologic stage. Potency was the most difficult single outcome to reach after surgery, and it was the main factor leading to pentafecta failure. LRP and RALP provide equivalent pentafecta rates for the pT3 disease and similar “tetrafecta” outcomes when potency recovery is not included among the postoperative expectations of the patient.
References
Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid HP, van der Kwast T, Wiegel T, Zattoni F, European Association of Urology (2011) EAU guidelines on prostate cancer: part 1. screening, diagnosis, and treatment of clinically localized disease. Eur Urol 59:61–71
Bianco FJ Jr, Scardino PT, Eastham JA (2005) Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology 66(5 suppl):83–94
Saranchuk JW, Kattan MW, Elkin E, Touijer AK, Scardino PT, Eastham JA (2005) Achieving optimal outcomes after radical prostatectomy. J Clin Oncol 23:4146–4151
Salomon L, Saint F, Anastasiadis AG, Sebe P, Chopin D, Abbou C–C (2003) Combined reporting of cancer control and functional results of radical prostatectomy. Eur Urol 44:656–660
Ficarra V, Sooriakumaran P, Novara G, Schatloff O, Briganti A, Van der Poel H, Montorsi F, Patel V, Tewari A, Mottrie A (2012) Systematic review of methods for reporting combined outcomes after radical prostatectomy and proposal of a novel system: the survival, continence, and potency (SCP) classification. Eur Urol 61:541–548
Patel VR, Sivaraman A, Coelho RF et al (2011) Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol 59:702–707
Eastham JA, Scardino PT, Kattan MW (2008) Predicting an optimal outcome after radical prostatectomy: the trifecta nomogram. J Urol 179:2207–2210
Asimakopoulos AD, Montes VEC, Gaston R (2012) Robot-assisted laparoscopic radical prostatectomy with intrafascial dissection of the neurovascular bundles and preservation of the pubovesical complex: a step-by-step description of the technique. J Endourol 26:1578–1585. doi:10.1089/end.2012.0405 Epub 16 October 2012
Asimakopoulos AD, Annino F, D’Orazio A, Pereira CF, Mugnier C, Hoepffner JL, Piechaud T, Gaston R (2010) Complete periprostatic anatomy preservation during robot-assisted laparoscopic radical prostatectomy (RALP): the new pubovesical complex-sparing technique. Eur Urol 58:407–417. doi:10.1016/j.eururo.2010.04.032 Epub 18 May 2010
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6, 336 patients and results of a survey. Ann Surg 240:205–213
Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D’Amico AV, Dmochowski RR, Eton DT, Forman JD, Goldenberg SL, Hernandez J, Higano CS, Kraus SR, Moul JW, Tangen C, Thrasher JB, Thompson I (2007) Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol 177:540–545
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, Menon M, Montorsi F, Patel VR, Stolzenburg JU, Van der Poel H, Wilson TG, Zattoni F, Mottrie A (2012) Systematic review and metaanalysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 62:405–417. doi:10.1016/j.eururo.2012.05.045
Ficarra V, Novara G, Ahlering TE, Costello A, Eastham JA, Graefen M, Guazzoni G, Menon M, Mottrie A, Patel VR, Van der Poel H, Rosen RC, Tewari AK, Wilson TG, Zattoni F, Montorsi F (2012) Systematic review and metaanalysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol 62:418–430. doi:10.1016/j.eururo.2012.05.046
Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P (2012) Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and metaanalysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol 62:1–15. doi:10.1016/j.eururo.2012.02.029
Porpiglia F, Morra I, Chiarissi ML, Manfredi M, Mele F, Grande S, Ragni F, Poggio M, Fiori C (2013) Randomised controlled trial comparing laparoscopic and robot-assisted radical prostatectomy. Eur Urol 63:606–614
Asimakopoulos AD, Pereira Fraga CT, Annino F, Pasqualetti P, Calado AA, Mugnier C (2011) Randomized comparison between laparoscopic and robot-assisted nerve-sparing radical prostatectomy. J Sex Med 8:1503–1512
Ploussard G, de la Taille A, Moulin M, Vordos D, Hoznek A, Abbou CC, Salomon L (2012) Comparisons of the perioperative, functional, and oncologic outcomes after robot-assisted versus pure extraperitoneal laparoscopic radical prostatectomy. Eur Urol. doi:10.1016/j.eururo.2012.11.049
Park B, Kim W, Jeong BC, Jeon SS, Lee HM, Choi HY, Seo SI (2013) Comparison of oncological and functional outcomes of pure versus robotic-assisted laparoscopic radical prostatectomy performed by a single surgeon. Scand J Urol 47:10–18. doi:10.3109/00365599.2012.696137
Schroeck FR, Krupski TL, Sun L, Albala DM, Price MM, Polascik TJ, Robertson CN, Tewari AK, Moul JW (2008) Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol 54:785–793. doi:10.1016/j.eururo.2008.06.063 Epub 23 June 2008
Pierorazio PM, Spencer BA, McCann TR, McKiernan JM, Benson MC (2007) Preoperative risk stratification predicts likelihood of concurrent PSA-free survival, continence, and potency (the trifecta analysis) after radical retropubic prostatectomy. Urology 70:717–722
Xylinas E, Durad X, Ploussard G et al (2013) Evaluation of combined oncologic and functional outcomes after robotic-assisted laparoscopic extraperitoneal radical prostatectomy: trifecta rate of achieving continence, potency, and cancer control. Urol Oncol 31:99–103. doi:10.1016/j.urolonc.2010.10.012
Disclosures
Drs. Anastasios D. Asimakopoulos, Roberto Miano, Nicola Di Lorenzo, Enrico Spera, Giuseppe Vespasiani, and Camille Mugnier have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asimakopoulos, A.D., Miano, R., Di Lorenzo, N. et al. Laparoscopic versus robot-assisted bilateral nerve-sparing radical prostatectomy: comparison of pentafecta rates for a single surgeon. Surg Endosc 27, 4297–4304 (2013). https://doi.org/10.1007/s00464-013-3046-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3046-9