Abstract
Background
This study aimed to evaluate the operative and clinical outcomes in a series of 302 consecutive laparoscopic splenectomies and to analyze the risk factors of postoperative complications.
Methods
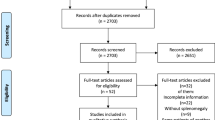
The study retrospectively reviewed 302 consecutive patients who underwent laparoscopic splenectomy. The patients were classified into three disease groups: benign spleen-related disease (group 1, n = 196), malignant spleen-related disease (group 2, n = 42), and portal hypertension (group 3, n = 64). The three groups were compared in terms of perioperative data. Postoperative complications were classified into three complication groups according to the Clavien–Dindo Classification of Surgical Complications and Severity: no complication, mild complications, and severe complications. Multivariate logistic regression was used to analyze the independent risk factors of postoperative complications.
Results
The patients in group 1 were younger and had a higher body mass index, a lower American Society of Anesthesiology (ASA) score, and a smaller spleen than the patients in groups 2 and 3. Fewer patients in group 1 required hand-port assistance than in the other two groups. Group 1 had shorter operative times, required fewer transfusions, presented a lower incidence of complications, and had shorter postoperative stays than groups 2 and 3. In the analysis of complications, high ASA score was an independent risk factor for the occurrence of complications. Both high ASA score and larger spleen size were independent risk factors for the occurrence of severe complications. Compared with total laparoscopic splenectomy, the data including the hand-assisted cases showed a reduction in odds ratio for both the occurrence of complications and the occurrence of severe complications.
Conclusions
The treatment of malignant spleen-related disease and portal hypertension with laparoscopic splenectomy is more challenging than the treatment of benign disease. High ASA score is an independent risk factor for the occurrence of complications, whereas high ASA score and larger spleen size are both independent risk factors for the occurrence of severe complications. The appropriate introduction of the hand-assisted technique may facilitate the laparoscopic procedure and reduce postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since the first description of laparoscopic splenectomy (LS) in 1991 [1], LS has become the technique of choice for removal of the spleen. Together with the accumulation of experience and technical innovations, indications for LS have rapidly increased, and LS currently is considered the choice for almost all spleen-related disease requiring splenectomy, including benign spleen-related disease, malignant spleen-related disease [2, 3], and portal hypertension [4, 5].
According to the European Association for Endoscopic Surgery (EAES) [6], some of the aforementioned conditions, such as malignancy and portal hypertension, still are challenging in terms of technique. Indeed, the bulk and vascularity of the spleen as well as the pathologic processes taking place make splenectomy-related complications a major concern for LS [7]. However, few studies have investigated these concerns, especially studies based on a large series of procedures performed by a single surgeon. This allows for a clearer comparison of outcomes after the application of LS in the treatment of these diseases requiring splenectomy.
Moreover, no uniform standard exists to grade postoperative complications or to analyze the risk factors for complications after LS. This study therefore aimed to evaluate the efficacy of LS in the treatment of these various diseases and to determine risk factors for postoperative complications.
Patients and methods
Patients
Between 2003 and 2012, a total of 302 consecutive patients were referred for splenectomy to the Department of Hepatobiliary Pancreatic Surgery at West China Hospital of Sichuan University, China. Patients who had concomitantly undergone other major surgery were excluded from the study.
All the surgeries were performed by the same surgeon. The patients were divided into three disease groups on the basis of clinical diagnosis: benign spleen-related disease (group 1, n = 196), malignant spleen-related disease (group 2, n = 42), and splenomegaly secondary to portal hypertension (group 3, n = 64). The indications for splenectomy in group 2 patients with non-Hodgkin lymphoma especially included symptomatic splenomegaly and hypersplenism (platelet count <30 × 109/L or white blood cell count <3 × 109/L).
The indications for splenectomy in the patients with portal hypertension included bleeding tendency due to thrombocytopenia (platelet count <30 × 109/L), difficulties receiving treatment for hepatocarcinoma or hepatitis due to thrombocytopenia, and high risk of esophageal variceal hemorrhage due to severe portal hypertension. To analyze the influence of splenomegaly on the postoperative complications and thus to take it as a parameter for preoperative evaluation, spleen size was divided into the following four groups: normal spleen size (≤15 cm), splenomegaly (15–17 cm), massive splenomegaly 17–22 cm), and supramassive splenomegaly (>22 cm) [8].
The hand-assisted technique was routinely applied in patients with supramassive splenomegaly (spleen size, >22 cm) and patients with portal hypertension after October 2009. Postoperative complications were classified into three groups according to the Clavien–Dindo Classification of Surgical Complications [9] and according to previous experience as follows: no complications, mild complications (grade 1: complications involving any deviation from the normal postoperative course without the need for pharmacologic treatment and complications needing surgical, endoscopic, or radiologic interventions; and grade 2: complications requiring pharmacologic treatment), and severe complications (grade 3: complications requiring surgical, endoscopic, or radiologic intervention; grade 4: life-threatening complications requiring intensive care unit (ICU) management; and grade 5: death).
Patient demographics and perioperative clinical data were collected. Comparisons were performed among the three groups, and analyses in terms of risk factors for postoperative complications were performed.
Preoperative management
Preoperative computed tomography (CT) was routinely performed in all cases to assess spleen size and to evaluate the spleen-related disease. For patients with portal hypertension, we routinely conducted a screening esophagogastroduodenoscopy before surgery, and endoscopic variceal ligation was performed for patients with medium or large varices to prevent lethal hemorrhaging.
Antibiotic prophylaxis was started half an hour before surgery and continued until 2 days after surgery for all patients. In cases with apparent infection, antibiotic use was continued accordingly.
Surgical technique
All surgeries were performed with the patient under general anesthesia on an electric operating table to facilitate positioning. Patients were placed in a right semidecubitus position with the left flank elevated, and the operating table was slightly tilted in a reverse Trendelenburg position.
In LS procedures, the first 10-mm trocar, used for the 30° camera, was placed in a specific periumbilicus area depending on the splenic size and location. Three additional trocars then were placed at the subxiphoid for the laparoscopic grasper (5 mm); at the left midclavicular line below the margin of the spleen for the ultrasonic dissector, the biploar vessel sealing device, and the laparoscopic linear vascular stapler (12 mm); and at the left axillary line below the lower pole of the spleen for the laparoscopic grasper or aspiration (5 mm).
In the hand-assisted LS (HALS), the subxiphoid trocar was replaced by a 6-cm midline subxiphoid incision for the hand-port so the surgeon could insert his left hand into the abdominal cavity through the device. First, a careful intraabdominal exploration was performed. Then the splenogastric ligament was divided, after which attachments and ligaments were dissected in the order of splenocolic ligament, splenorenal ligament, and splenophrenic ligament. Generally, perisplenic hemostasis was achieved via an ultrasonic dissector or a laparoscopic suture, or more recently, with the aid of a biploar vessel-sealing device.
After the spleen had been mobilized from the attachments and ligaments, the hilar pedicles were transected by the laparoscopic linear vascular stapler. Finally, the spleen was manipulated into a retrieval bag and retracted. A closed suction drain was routinely placed in the left subphrenic area to detect postoperative bleeding or pancreatic leakage and to prevent fluid collection.
Statistical analysis
The operative time was measured from the first incision to skin closure, and the postoperative hospital stay was measured as the number of days between surgery and discharge or transfer from our department. Statistical analysis was performed using SPSS 17.0 for windows (SPSS, Chicago, IL, USA). Data are reported as mean ± SD or counts (%). Comparisons among groups were conducted by analysis of variance, chi-square test, and Fisher’s exact test. Multivariate logistic regression was used to analyze the independent risk factors for postoperative complications.
Results
Laparoscopic splenectomy was attempted for 302 patients comprising three disease groups based on diagnosis as follows: benign spleen-related disease (group 1 [G1], n = 196), malignant spleen-related disease (group 2 [G2], n = 42) and splenomegaly secondary to portal hypertension (group 3 [G3], n = 64). Patient demographic and preoperative data are listed in Table 1. The three groups did not differ significantly in terms of gender. The patients in group 1 were younger and had a higher body mass index (BMI) as well as a lower American Society of Anesthesiology (ASA) score than the patients in groups 2 and 3.
The hemoglobin levels were significantly higher in group 1 than in group 2. The white blood cell count was significantly higher in group 3 than in group 1. The patients in group 3 had the lowest level of platelets in the three groups. The patients in groups 2 and 3 had significantly larger spleens than the patients in group1.
As shown in Table 2, fewer patients in group 1 required hand-port than in the other two groups: 5 of 196 patients in group 1, 20 of 42 patients in group 2, and 25 of 64 patients in group 3 required a hand-port. The patients in group 1 had significantly shorter operative times, required fewer transfusions, had a lower incidence of complications, and experienced shorter postoperative hospital stays than the patients in groups 2 and 3.
The estimated blood loss was less in group 1 than in group 3. The three groups did not differ significantly in terms of conversion rate, accessory spleen, or mortality.
As shown in Table 3, the pathologic results for the three groups indicated that idiopathic thrombocytopenic purpura (ITP, n = 142), constituting 72 % of the pathologic diagnoses in group 1, was the most common benign spleen-related disease. Other relatively rare benign spleen-related diseases included benign splenic tumor (n = 30), beta-thalassaemia (n = 11), autoimmune hemolytic anemia (n = 7), hereditary spherocytosis (n = 5), and Niemann-Pick disease (n = 1).
In group 2, non-Hodgkin lymphoma, constituting 71 % of the pathologic diagnoses in this group (data not shown), was the most common malignant spleen-related disease. Other relatively rare diagnoses in this group included leukemia (n = 8) and metastatic tumor (n = 4).
The presence of postoperative complications was one of the main outcome variables investigated in our study. As shown in Tables 4, 5 and 6, the postoperative complications were divided into three classes: no complications, mild complications, and severe complications. In group 1, postoperative complications arose in 30 (15%) of 196 patients, with 23 (11%) of the 196 patients experiencing mild complications and 7 (4%) experiencing severe complications. In group 2, 16 (38%) of 42 patients experienced postoperative complications, including nine patients (21%) with mild complications and seven patients (17%) with severe complications. In group 3, 25 (39%) of 64 patients experienced postoperative complications, including 17 patients (17%) with mild complications and 14 patients (22%) with severe complications.
To investigate better the risk factors for postoperative complications, a multiple logistic regression model was used in this study. The analysis showed that regardless of the inclusion or exclusion of the hand-assisted cases, a high ASA score was an independent risk factor for the occurrence of complications and that both high ASA score and larger spleen size were independent risk factors for the occurrence of severe complications. However, the data including HALS (n = 302) showed a significant reduction in the odds ratio (OR) for both the occurrence of complications and the occurrence of severe complications. Particularly for patients with supramassive splenomegaly, the risk for experiencing severe complications was approximately 22 times (OR, 22.311) that for patients with normal spleen size (≤15 cm) when hand-assisted cases were excluded (n = 252). However, the OR decreased to 6.713 when hand-assisted cases were included (n = 302).
Discussion
Since the first reports of LS in 1991 [1], the laparoscopic approach for removal of the spleen has gained favor over conventional surgery due to its advantages in terms of both morbidity rates [7] and cosmetic results. Although almost all spleen-related disease requiring splenectomy may be considered an indication for LS, certain situations still prove challenging for the laparoscopic approach, including supramassive splenomegaly [10] and portal hypertension [6]. To overcome these challenges, the hand-port technique has been applied [11, 12]. Using a hand-port, the surgeon can insert a hand into the abdomen while pneumoperitoneum is maintained and use the hand to assist in the surgical procedure directly. Meanwhile, the incision for the hand-port also provides a convenient means for extracting the enlarged spleen.
Many articles have published data regarding LS in the treatment of benign and malignant spleen-related disease. In a review of LS used for hematologic disease, Baccarani et al. [13] showed that LS was as safe and effective as open splenectomy for hematologic diseases and that it had several advantages over the open approach such as a shorter postoperative hospital stay, better cosmetic results, and a more rapid return to regular activities. In addition, both Makrin et al. [14] and Tessier et al. [15] demonstrated the feasibility and safety of LS for diagnosis and treatment of both benign and malignant tumors of the spleen. All these results suggest that LS is the best treatment for both benign and malignant spleen-related diseases.
Patients with portal hypertension generally present with splenomegaly, thrombocytopenia, and frequently the coexistence of perisplenic collateral vessels, as well as poor liver function [16]. Therefore, the risk of intraoperative uncontrolled bleeding and perisplenic structure injury are increased, which makes the application of LS for these patients controversial.
Although portal hypertension was considered a contraindication for LS in the 2008 clinical practice guidelines of the European Association for Endoscopic Surgery [6], some reports nevertheless published successful application of LS for patients with portal hypertension. Cai et al. [5] and Anegawa et al. [17] respectively demonstrated the safety, feasibility, and effectiveness of LS in patients with portal hypertension, with patients generally attaining favorable postoperative outcomes.
In the current study, all the patients in the three groups had satisfactory outcomes except the two patients who died in groups 1 and 2, respectively. The two deaths were not directly related to the surgical procedures but rather to the progression of underlying disease. Consistent with other reports [8, 10, 18], our results suggest that the significantly larger spleen sizes in the malignant group (group 2: 23.6 ± 8.7 cm) and the portal hypertension group (group 3: 22.6 ± 7.3 cm) increased the difficulty of the operative procedures.
To overcome the limitation of spleen size with the laparoscopic approach, a number of methods have been reported. Hama et al. [19] used preoperative splenic balloon catheters and platelet transfusions for patients with splenomegaly due to portal hypertension. Poulin et al. [20] and Iwase et al. [21] performed splenic artery embolization before LS in patients with splenomegaly. However, these methods still had limitations when confronted with extremely enlarged spleens (spleen size >30 cm).
In our study, patients with extremely enlarged spleens accounted for 32 (10.5%) of the 302 patients (data not shown). To meet this challenge, we introduced the hand-assisted technique. With this technique, surgeons can manipulate enlarged spleens with relative ease, providing good exposure and also hemostasis when required. As we demonstrated in our previous study, the application of the hand-assisted technique was superior to total LS in patients with portal hypertension and supramassive splenomegaly [22]. Furthermore, although the patients with malignant spleen disease and those with portal hypertension in our study had longer operative times and more blood loss, more frequently requiring transfusions than the patients with benign spleen-related disease, appropriate application of LS with the help of hand-port in these patients demonstrated satisfactory outcomes.
Several single-center trials have reported LS to be safe and to have an acceptably low complication rate. Rosen et al. [23] showed a 4 % incidence of minor complications and a 12 % incidence of major complications with LS used for hematologic diseases. Hama et al. [19] and Tomikawa et al. [24] reported the postoperative complication rate for patients with portal hypertension who underwent LS to be respectively 11.8 and 19 %. However, the true impact of LS on the incidence of postoperative complications still is uncertain because single-center studies often are relatively small in scale and lack a uniform standard for classifying complications.
Our study graded postoperative complications based on the Clavien–Dindo Classification of Surgical Complications [9], grouping postoperative complications into three levels to facilitate clinical application. In the three-grade classification system, all postoperative complications could be clearly graded on the basis of severity. Our results showed that the incidence of postoperative complications was significantly higher in group 2 (38 %) and group 3 (39 %) than in group 1 (15 %). Moreover, the incidences of severe complications in group 2 (17 %) and group 3 (22 %) also were significantly higher than in group 1 (4 %).
In 1963, ASA scoring was introduced by the American Society of Anesthesiologists [25]. This scoring has been used as a predictor of patient outcomes in many different types of surgeries. Many studies give results relating the ASA score to postoperative complications. In a prospective study consisting of 6,301 open surgery patients, Wolters et al. [26] indicated that a high ASA score was closely related to the occurrence of postoperative complications. Due to the advantages of LS in terms of complications, it was unclear whether the ASA score could be used as a predictor of postoperative complications.
In our study, a logistic regression was implemented to clarify this link between the ASA score and the risk for postoperative complications. Our results suggest that a high ASA score is an independent risk factor both for the occurrence of complications and for the occurrence of severe complications. Consistent with our study, Kavic et al. [27] also found the ASA score to be tightly associated with the postoperative complications in patients undergoing LS. As such, we propose with relative confidence that a high ASA score is an independent risk factor for postoperative complications in LS.
Many studies have suggested a close relationship between splenic size and risk of postoperative complications. Patel et al. [28] demonstrated that splenomegaly was an independent risk factor for complications of LS and that patients with massive splenomegaly (>1,000 g) were 14 times more likely to have postoperative complications. A multicenter study also indicated that spleen longitudinal diameter is an independent predictor for the occurrence of postoperative complications [29].
The logistic regression used in our study showed splenic size to be a risk factor for the occurrence of severe complications. This finding is relevant to surgeons in making clinical decisions because severe complications greatly affect patient outcomes and often require surgical intervention or ICU care. To investigate the influence of HALS on the occurrence of postoperative complications in these patients, we applied the data including and excluding patients who underwent HALS for further analysis. As a result, data both including and excluding patients who underwent HALS after 2009 showed significant differences in the OR with regard to ASA score and splenic size. Interestingly, for the patients with supramassive splenomegaly, the data including hand-assisted cases showed a significant reduction in OR (from 22.311 to 6.713) compared with the data that did not include hand-assisted cases. Thus, our results suggest that when the hand-assisted technique is used in patients with supramassive splenomegaly, the risk of severe complications may be significantly reduced.
With the hand-assisted approach, surgeons can gently manipulate extremely enlarged spleens, decreasing the need for traumatic retraction and blunt dissection. Meanwhile, the introduction of tactile feedback helps to facilitate secure and precise placement of laparoscopic linear staples. We speculate that HALS helps to reduce the occurrence of complications by minimizing injury to the pancreas and other neighboring structures. We therefore recommend the hand-assisted technique for patients with supramassive splenomegaly. Preoperative assessment of splenic size and ASA score to identify high-risk patients will help in determining when adoption of the hand-assisted technique is appropriate for a given LS procedure.
In summary, although this was a nonrandomized and retrospective study without direct analysis of risk factor for postoperative complications related to HALS, we still can draw the following conclusions from our large series:
-
1.
Although the treatment of malignant spleen-related disease and portal hypertension with LS is more challenging than its use for benign disease, LS still is safe and effective for these patients.
-
2.
High ASA score is an independent risk factor for the occurrence of complications, whereas high ASA score and larger spleen size are both independent risk factors for the occurrence of severe complications.
-
3.
Appropriate introduction of hand-assisted technique may facilitate the laparoscopic procedure and reduce postoperative complications.
Future randomized controlled prospective studies are required to obtain more detailed information about LS.
References
Delaitre B, Maignien B (1991) Splenectomy by the laparoscopic approach: report of a case. Presse Med 20:2263
Knauer EM, Ailawadi G, Yahanda A et al (2003) 101 laparoscopic splenectomies for the treatment of benign and malignant hematologic disorders. Am J Surg 186:500–504
Schlachta CM, Poulin EC, Mamazza J (1999) Laparoscopic splenectomy for hematologic malignancies. Surg Endosc 13:865–868
Wang Y, Zhan X, Zhu X et al (2010) Laparoscopic splenectomy in portal hypertension: a single-surgeon 13-year experience. Surg Endosc 24:1164–1169
Cai YQ, Zhou J, Chen XD et al (2011) Laparoscopic splenectomy is an effective and safe intervention for hypersplenism secondary to liver cirrhosis. Surg Endosc 25:3791–3797
Habermalz B, Sauerland S, Decker G et al (2008) Laparoscopic splenectomy: the clinical practice guidelines of the European association for endoscopic surgery (EAES). Surg Endosc 22:821–848
Winslow ER, Brunt LM (2003) Perioperative outcomes of laparoscopic versus open splenectomy: a meta-analysis with an emphasis on complications. Surgery 134:647–653
Grahn SW, Alvarez JR, Kirkwood K et al (2006) Trends in laparoscopic splenectomy for massive splenomegaly. Arch Surg 141:755–762
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Mahon D, Rhodes M (2003) Laparoscopic splenectomy: size matters. Ann R Coll Surg Engl 85:248–251
Katkhouda N, Lord RV (2000) Once more, with feeling: handoscopy, or the rediscovery of the virtues of the surgeon’s hand. Surg Endosc 14:985–986
Hellmann P, Ardvinsson D, Rastad J (2000) Handport-assisted laparoscopic splenectomy in massive splenomegaly. Surg Endosc 14:1177–1179
Baccarani U, Donini A, Terrosu G et al (1999) Laparoscopic splenectomy for hematological diseases: review of current concepts and opinions. Eur J Surg 165:917–923
Makrin V, Avital S, White I et al (2008) Laparoscopic splenectomy for solitary splenic tumors. Surg Endosc 22:2009–2012
Tessier DJ, Pierce RA, Brunt LM et al (2008) Laparoscopic splenectomy for splenic masses. Surg Endosc 22:2062–2066
Schuppan D, Afdhal NH (2008) Liver cirrhosis. Lancet 371:838–851
Anegawa G, Kawanaka H, Uehara H et al (2009) Effect of laparoscopic splenectomy on portal hypertension gastropathy in cirrhotic patients with portal hypertension. J Gastrenterol Hepatol 24:1554–1558
Terrosu G, Baccarani U, Bresadola V et al (2002) The impact of splenic weight on laparoscopic splenectomy for splenomegaly. Surg Endosc 16:103–107
Hama T, Takifuji K, Uchiyama K et al (2008) Laparoscopic splenectomy is a safe and effective procedure for patients with splenomegaly due to portal hypertension. J Hepatobiliary Pancreat Surg 15:304–309
Poulin EC, Mamazza J, Schlachta CM et al (1998) Splenic artery embolization before laparoscopic splenectomy: an update. Surg Endosc 12:870–875
Iwase K, Higaki J, Mikata S et al (1999) Laparoscopically assisted splenectomy following preoperative splenic artery embolization using contour emboli for myelofibrosis with massive splenomegaly. Surg Laparosc Endosc Percutan Tech 9:197–202
Wang X, Li Y, Zhou J et al (2012) Hand-assisted laparoscopic splenectomy is a better choice for patients with supramassive splenomegaly due to liver cirrhosis. J Laparoendosc Adv Surg Tech A 22:962–967
Rosen M, Brody F, Walsh RM et al (2002) Outcome of laparoscopic splenectomy based on hematologic indication. Surg Endosc 16:272–279
Tomikawa M, Akahoshi T, Sugimachi K et al (2010) Laparoscopic splenectomy may be a superior supportive intervention for cirrhotic patients with hypersplenism. J Gastroenterol Hepatol 25:397–402
American Society of Anesthesiologists (1963) New classification of physical status. Anesthesiology 24:111
Wolters U, Wolf T, Stutzer H et al (1996) ASA classification and perioperative variables as predictor of postoperative outcome. Br J Anaesth 77:217–222
Kavic SM, Segan RD, Park AE et al (2005) Laparoscopic splenectomy in the elderly: a morbid procedure? Surg Endosc 19:1561–1564
Patel AG, Parker JE, Wallwork B et al (2003) Massive splenomegaly is associated with significant morbidity after laparoscopic splenectomy. Ann Surg 238:235–240
Casaccia M, Torelli P, Pasa A et al (2010) Putative predictive parameters for the outcome of laparoscopic splenectomy: a multicenter analysis performed on the Italian registry of laparoscopic surgery of the spleen. Ann Surg 251:287–291
Acknowledgments
The study was supported by the West China Hospital, Sichuan University.
Disclosures
Xin Wang, Yongbin Li, Nicolas Crook, Bing Peng, and Ting Niu have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xin Wang, Yongbin Li, Bing Peng and Ting Niu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, X., Li, Y., Crook, N. et al. Laparoscopic splenectomy: a surgeon’s experience of 302 patients with analysis of postoperative complications. Surg Endosc 27, 3564–3571 (2013). https://doi.org/10.1007/s00464-013-2978-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2978-4