Abstract
Background
Cancer gastrectomy seems to benefit type 2 diabetes; however, results are conflicting. In a prospective protocol, including retrospective information, the aim was assessment of changes in glucose profile in patients with both normal and deranged preoperative glucose homeostasis.
Methods
Patients (N = 164) with curative subtotal or total Roux-en-Y gastrectomy for gastric cancer (n = 92), or Roux-en-Y gastric bypass for morbid obesity (RYGB, n = 72) were preoperatively classified into diabetes (including prediabetes) and control group. Postoperative diabetes outcome was stratified as responsive or refractory, and results in controls were correspondingly defined as stable or new-onset diabetes (NOD), according to fasting blood glucose and HbA1c. Dietary intake and biochemical profile was documented. Statistical methods included analysis of variance, multivariate logistic regression, and propensity score matching according to postoperative weight loss.
Results
Age of cancer cases was 67.9 ± 11.5 years, 56.5 % males, initial body mass index (BMI) 24.7 ± 3.7, current BMI 22.6 ± 3.8 kg/m2, and follow-up 102.1 ± 51.0 months, whereas in bariatric individuals age was 51.4 ± 10.1 years, 15.3 % males, initial BMI 56.7 ± 12.2, current BMI 34.8 ± 8.1 kg/m2, and follow-up 104.1 ± 29.7 months. Refractory disease corresponded to 62.5 % (cancer) versus 23.5 % (bariatric) (P = 0.019), whereas NOD represented 69.2 versus 23.8 % respectively (P = 0.016). Weight loss (ΔBMI) was associated with diabetes response in cancer patients but not with NOD. No difference between subtotal and total gastrectomy was detected. Divergent outcomes (refractory vs. responsive) were confirmed in BMI-similar, propensity-matched cancer gastrectomy patients with preoperative diabetes, consistent with weight-dependent and -independent benefits.
Conclusions
Diabetes response was confirmed, however with more refractory cases than in bariatric controls, whereas high proportions of NOD occurred. Such dichotomous pattern seems unusual albeit consistent with previous studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastrectomy for cancer, and particularly total gastrectomy, has been associated with postprandial hyperglycemia and impaired insulin response in the early postoperative period. In one study, such derangement correlated with HbA1c concentration, suggesting a lasting impact and possible precipitation of diabetes mellitus [1]. Such findings are in agreement with experimental and clinical protocols, demonstrating diminished tolerance to oral glucose challenge and insufficient insulin response in gastrectomized mice and patients [2, 3].
In contrast, it is reported that nonobese diabetic patients undergoing cancer and noncancer stomach resection exhibit diabetes alleviation. Responses comparable to, and occasionally exceeding, those seen in bariatric interventions are announced, notably with Roux-en-Y reconstruction. Lanzarini et al. [4] documented remission or improvement in more than 95 % of the cases. Cai et al. [5] observed 90 % success in those submitted to Roux-en-Y reconstruction. Yang et al. [6] reported amelioration in 81 %, and 71 % of the subjects in the cohort of Zervos et al. [7] benefited. Such effects became apparent after periods ranging from a few months to many years.
More disappointing outcomes can be found as well, with weak or absent diabetes amelioration after gastrectomy [8, 9]. Most series include recently operated participants, among which active cancer is difficult to rule out. Body weight changes are not always recorded, therefore implications of weight loss and calorie restriction are incompletely known, only extent of resection and modality of reconstruction, with or without duodenal exclusion, being underscored in most circumstances. Control cohorts are rarely considered; consequently appreciation of the natural history of diabetes in such context cannot always be gleaned.
Given the relevance of the subject and the relatively scarce and controversial literature, a study documenting postoperative diabetes course was designed. The objective was long-term assessment of changes in glucose profile in patients submitted to gastrectomy, with both normal and deranged preoperative glucose homeostasis.
To the best of our knowledge, this is the first protocol simultaneously addressing diabetic and nondiabetic populations, respectively undergoing cancer gastrectomy along with Roux-en-Y gastric bypass (RYGB) for morbid obesity.
Mechanisms sparking attenuation of diabetes after conventional gastrectomy were expected to be the same as in bariatric surgery, namely weight loss combined with remodeling of the gastrointestinal tract. Nonetheless, weaker benefits were predicted, given the older age, heavier diabetes burden, and milder weight loss. The risk of adverse effects of cancer gastrectomy on glucose regulation in nondiabetic controls also was considered a worthy hypothesis, as anticipated before [1–3].
Methods
Experimental design and patient enrollment
This was a prospective, observational case-control study including retrospective information, in which cancer patients undergoing stomach resection were compared with a control population of RYGB patients (Trial Registration Identifier: NCT 01518023). Operated candidates in the late follow-up period were recruited for selection and informed consent, subsequently undergoing clinical and biochemical assessment. Preoperative information was retrieved from hospital files. In both the cancer and the morbid obesity cohorts, priority was given to patients with impaired fasting glucose to avoid underrepresentation of such category. In this sense, this was a consecutive series within each glucose homeostasis modality. Patients screened for the presence of prediabetes or diabetes were consecutively enrolled in the appropriate group, and the same was done with those free from such derangements.
Population
Patients who underwent curative subtotal or total gastrectomy for gastric cancer or gastric bypass for morbid obesity, both with Roux-en-Y reconstruction, were consecutively recruited (N = 164). Criteria of inclusion were age >18 years (males and females), >3 years follow-up, stable weight in the past year, no evidence of disease (for cancer patients), and informed consent. Criteria of exclusion were additional surgical procedures or take-down of the original operation, dumping syndrome, organ or cell transplantation, HIV/AIDS, tuberculosis or other consumptive disease, history of pancreatitis or pancreatic surgery, organ failures, use of corticosteroids, immune modulators, radio- or chemotherapy, malnutrition requiring protein-calorie supplementation, pregnancy or lactation, alcohol or drug addiction, cognitive impairment or Alzheimer’s disease, and refusal to participate in the study.
Stratification
In the main cancer cohort, presence of prediabetes or diabetes was confirmed (diabetics, n = 40), whereas a second group without derangements of glucose homeostasis (controls, n = 52) was included.
Bariatric candidates submitted to RYGB (n = 72), identically stratified and matched regarding follow-up period, were studied for comparative purposes (Fig. 1). Matching according to age was not possible because of the demographic gap; however, bariatric cases <40 years old were eliminated (Fig. 1).
Definitions
DM and prediabetes were diagnosed according to the 2010 criteria of the American Diabetes Association [10]. An individual was considered to have diabetes if receiving pharmacologic prescription, with fasting blood glucose (FBG) ≥126 mg/dL, or with HbA1c ≥6.5 %. Prediabetes was identified by impaired fasting glucose (100–125 mg/dL) or HbA1c 5.7–6.4 %, with or without medication. Controls were those with normal biochemistry and negative clinical history. New-onset prediabetes or diabetes (NOD) was recognized in both cancer and bariatric controls who subsequently developed FBG ≥100 mg/dL or HbA1c ≥5.7 %. Because HbA1c was not registered in the preoperative investigation of the controls, a bias in the interpretation of current findings was possible. In this sense, two sets of NOD results were calculated, either including or not including HbA1c pattern.
Whenever diabetic cases converted to prediabetes or normal, or prediabetics shifted to FBG <100 mg/dL and HbA1c <5.7 % without medication, patients were classified as responsive. Those who failed to achieve such improvements were reported as refractory. Except when otherwise indicated, diabetes and prediabetes are considered as a single group in all circumstances.
Surgical technique
Curative cancer gastrectomy entailed subtotal or total gastric ablation, with or without lymphadenectomy or splenectomy. All procedures involving pancreatic resection were excluded. For reconstruction, a Roux-en-Y jejunal limb of 40 cm, with a biliopancreatic limb of 60–80 cm, was employed. Open RYGB involved the creation of a vertical gastric pouch of 30–50 mL, a Roux-en-Y jejunal limb of 100 cm, and a biliopancreatic limb of 60–80 cm.
Protein and calorie intake
A validated food-frequency questionnaire was selected and Dietsys software, version 4.0 (National Cancer Institute, Bethesda, MD) was used for macronutrient and fiber content.
Biochemical variables
Hematologic counts, lipid fractions, FBG and HbA1c were part of the protocol. Blood samples were collected in the morning subsequent to overnight fast and were measured by a modular analytical system (Roche/Hitachi Diagnostics, Sao Paulo, Brazil). HbA1c was examined by immunoturbidimetry (Boehringer Mannheim, Sao Paulo, Brazil). Blood cells were documented in a Coulter automatic counter (Beckman Coulter, Sao Paulo, Brazil). The same tests were transcribed from preoperative files.
Statistical analysis
Numerical variables were compared by analysis of variance (ANOVA) and post-hoc Bonferroni test, employing log transformation when appropriate. Chi-square test was used for discrete variables. Univariate and multivariate logistic regression analysis of clinical and biochemical variables and diabetes outcome after cancer gastrectomy was conducted.
A nested case-control population was established to measure association between weight loss and diabetes response, by means of propensity scoring responsive and refractory cancer patients. Univariate predictors of diabetes evolution with P < 0.001 (initial HDL cholesterol, current LDL cholesterol) as well as multivariate significant measurements [body mass index (BMI) change] were entered into the model. A backward, stepwise elimination process removed covariates with P > 0.25. With the coefficients of the final regression equation, a propensity score was calculated for each patient, followed by matching to a similar control. After all pairs were identified, individual demographic data were compared for confirmation. Statistical Analysis Systems, version 9.1.3 (SAS Institute, Cary, NC), was used, and differences were considered significant when P < 0.05.
Results
Preliminary survey encompassed 169 participants; however, three were excluded on account of renal failure (n = 1), liver cirrhosis (n = 1), and recurrent malignancy (n = 1) among the cancer patients. Just two exclusions occurred in the bariatric population, both due to difficulty to come to the hospital. Final population was 164 cases.
Total gastrectomy was performed in 45.7 % (42/92) of the cancer cases; the remaining 54.3 % were able to keep the proximal stomach (subtotal gastrectomy). Initial features of these patients can be observed in Table 1. The three subgroups were fairly comparable, with occasional differences concerning controls. Fasting glucose was numerically higher in refractory patients as expected; however, due to scattering of the values significance was not confirmed (Table 1).
Nearly half of the refractory patients (48 %, 12/25) exhibited prediabetes; 26.7 % (4/15) of the responsive cases were in this category. Only three patients (7.5 %, 3/40) were insulin-dependent (all of them refractory), and an additional eight (seven of them refractory) were taking oral glucose-lowering prescriptions (20 %, 8/40). All other participants with diabetes or prediabetes (72.5 %, 29/40) were first diagnosed when admitted to the hospital. As a consequence, disease duration could not be calculated.
Bariatric cases had similar follow-up but were younger, more obese, and a higher proportion were female (Table 2). Two were insulin-dependent (3.9 %, 2/51) and 31.3 % (16/51) were managed with oral drugs. The majority (64.7 %, 33/51) were newly diagnosed cases, again precluding estimation of disease duration (Table 2).
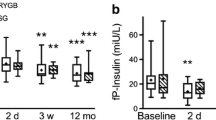
Only 37.5 % of the cancer diabetics metabolically benefitted after surgery, and none of them were insulin dependent, whereas roughly twice as many responded in the obese population. Not <69.2 % of the cancer control population progressed to prediabetes (63.4 %, 33/52) or diabetes (5.8 %, 3/52) during the follow-up period, significantly more than in the bariatric cohort (P = 0.011; Table 3). Weight change, even if negligible (4.2 ± 3.0 kg/m2, approximately 16 % of initial BMI) compared with corresponding bariatric individuals (23.3 ± 12.7 kg/m2, approximately 39 % of initial BMI) was associated with responsive diabetes in cancer cases (P = 0.045), however, not with metabolic deterioration toward NOD among cancer controls (P = 0.524; Table 3).
Maintenance or removal of the gastric fundus could not be linked to diabetes response or to weight loss; similar evolution was documented in both contexts (Table 4). Refractory outcome was associated with significantly less weight loss after either subtotal (P = 0.049) or total gastrectomy (P = 0.046; Table 4).
Energy and protein consumption revealed partially inadequate results in the NOD population and fiber consumption was low in all groups; however, in most circumstances the pattern was acceptable. Reduction of current alimentary consumption or qualitative changes compared with the preoperative diet was not demonstrated (Table 5).
By means of univariate and multivariate regression analysis of cancer gastrectomy, participants preoperative HDL cholesterol (P = 0.004), current LDL cholesterol (P = 0.007), and BMI change (P = 0.002) correlated with diabetes outcome. On the basis of such findings a propensity-score matched group was established with 30 patients (15 in each category), statistically comparable regarding the three confirmed variables as well as two weaker ones, operative technique (P = 0.094) and follow-up period (P = 0.078). Current FBG and HbA1c were obviously different as these were part of the defining criteria (Table 6).
Divergent outcomes persisted (responsive vs. refractory), indicating that weight loss was relevant however not the only influence on the clinical course of diabetes. Other factors were likely operative, such as pancreatic reserve and beta cell function, bile acids, incretins, and gut microbiome (Table 6).
Results in the present series were listed together with those reported by other centers [4–9, 11], aiming to provide an overview of the impact of cancer gastrectomy on diabetes. Diabetes improvement was confirmed; however, percentage was among the lowest at the same time as high rates of NOD occurred. Such results can be ascribed to the protocol design, with strict patient selection and long term follow-up (Table 7).
Discussion
Surgical normalization of glucose homeostasis may proceed through multiple pathways. Weight loss has been deemed crucial, and rearrangement of food transit with subsequent shifts in incretins and other hormones, potentially influencing satiety, pancreatic beta cell mass, and insulin resistance has much to endorse it [4, 6, 7, 9, 11, 12].
Within the gastric cancer context, influence of the malignancy itself should be one of the first concerns, as glucose dysmetabolism is recorded in this setting [13]. Eligibility criteria therefore should focus on disease-free, weight-stable participants with a long follow-up. Late evaluation was selected for a balanced appreciation; patients were interviewed after an average of 7 years. Antidiabetic benefits of surgical operations have remained stable along the years in some experiences, others suggesting slow but unrelenting erosion because of weight regain or age-related degeneration of pancreatic beta cell function [11, 14, 15].
End-points (FBG and HbA1c) followed accepted recommendations [10], whereas combined utilization of prediabetes and diabetes as a single modality is more debatable. Such option stemmed from the interest in covering a wider range of glucose homeostasis shifts induced by gastric intervention. There is a consensus that both prediabetes and diabetes share not only progression toward overt dysglycemia but also augmentation of cardiovascular risk [10, 16].
Weight loss participation in glucose homeostasis after cancer gastrectomy is not obvious, given the modest or negligible BMI shifts compared with the bariatric population. At the same time, weight regain, which has been incriminated in diabetes relapse after antiobesity operations [14, 15], never materialized. New-onset diabetics in this series exhibited no mean weight accrual; current BMI remained lower than before the operation and in the same range as stable controls. Propensity matched patients with BMI reduction equivalent to the responsive population still deteriorated toward refractory disease, confirming that both weight-related and non-weight-related insulin resistance pathways were responsible for the focused phenomenons.
Duodenojejunal exclusion does not seem to enhance glucose-lowering effects of ileal interposition [17], and its role in RYGB has been deemed less conspicuous than previously admitted [18]. Nevertheless, compelling evidence of its impact, including patients without weight loss, has been published [19, 20]. In contrast, no contribution could be ascribed to gastric fundus resection, subtotal and total modality proving irrelevant for diabetes outcome, in agreement with a recent survey [11].
New-onset diabetes after cancer surgery substantially exceeded the percentages observed in bariatric participants and also those published for the general population. Epidemiological surveys in standard middle-age or elderly cohorts unveil 17–29 % of combined new diagnosis of prediabetes and diabetes [12, 21, 22], or less than half current values. Although counterintuitive because it conflicts with the positive effects in diabetic patients, a diabetogenic role for conventional gastrectomy in euglycemic patients cannot be ruled out [1, 3] and should be further ascertained in future studies.
Conclusions
Roux-en-Y cancer gastrectomy was moderately advantageous for previous diabetics undergoing cancer gastrectomy; however, in euglycemic controls, the ensuing clinical course tended to be less favorable. Weight loss was identified as relevant for diabetes response after both partial and total gastrectomy, however not for prevention of new-onset diabetes, whereas no evidence of calorie restriction or dietary macronutrient changes was unveiled in any circumstance. It is speculated that duodenal exclusion was beneficial in this setting; however, no diabetes amelioration related to gastric fundus exclusion was noticed. Studies targeting additional populations and including the molecular basis of such phenomenons are recommended.
References
Yamamoto H, Tsuchihashi H, Akabori H, Naitoh H, Maegawa H, Tani T (2008) Postprandial hyperglycemia after a gastrectomy and the prediabetic state: a comparison between a distal and total gastrectomy. Surg Today 38:685–690
Salehi A, Chen D, Hakanson R, Nordin G, Lundquist I (1999) Gastrectomy induces impaired insulin and glucagon secretion: evidence for a gastro-insular axis in mice. J Physiol 514:579–591
Yoshikawa T, Noguchi Y, Nomura K, Fukuzawa K, Makino T, Tsuburaya A, Imada T, Matsumoto A (1996) Alimentary hyperglycemia in patients with subtotal gastrectomy is associated with decreased insulin secretion but not with insulin resistance. Int Surg 81:32–35
Lanzarini E, Csendes A, Lembach H, Molina J, Gutierrez L, Silva J (2010) Evolution of type 2 diabetes mellitus in non morbid obese gastrectomized patients with Roux-en-Y reconstruction: retrospective study. World J Surg 34:2098–2102
Cai JL, Li BQ, Zheng C, Lin XK, Yin K, Xu JR, Xu LB (2011) Impact of techniques for gastrointestinal tract reconstruction following gastrectomy on pancreatic beta-sell function in patients with type 2 diabetes mellitus. Zhonghua Wei Chang Wai Ke Za Zhi 14:415–418
Yang J, Li C, Liu H, Gu H, Chen P, Liu B (2010) Effects of subtotal gastrectomy and Roux-en-Y gastrojejunostomy on the clinical outcome of type 2 diabetes mellitus. J Surg Res 164:e67–e71
Zervos EE, Agle SC, Warren AJ, Lang CG, Fitzgerald TL, Dar M, Rotondo MF, Pories WJ (2010) Amelioration of insulin requirement in patients undergoing duodenal bypass for reasons other than obesity implicates foregut factors in the pathophysiology of type II diabetes. J Am Coll Surg 210:564–572
Herbella FA, Tineli AC, Wilson JL Jr, Del Grande JC (2009) Duodenal bypass does not decrease glucose levels of lean individuals with gastric cancer submitted to partial or total gastrectomy. Arq Gastroenterol 46:230–232
Lee W, Ahn SH, Lee JH, Park do J, Lee HJ, Kim HH, Yang HK (2012) Comparative study of diabetes mellitus resolution according to reconstruction type after gastrectomy in gastric cancer patients with diabetes mellitus. Obes Surg 22:1238–1243
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1):S62–S69
Kim JW, Cheong JH, Hyung WJ, Choi SH, Noh SH (2012) Outcome after gastrectomy in gastric cancer patients with type 2 diabetes. World J Gastroenterol 18:49–54
Kowall B, Rathmann W, Heier M, Holle R, Peters A, Thorand B, Herder C, Strassburger K, Giani G, Meisinger C (2012) Impact of weight and weight change on normalization of prediabetes and on persistence of normal glucose tolerance in an older population: the KORA S4/F4 study. Int J Obes (Lond) 36:826–833
Cai Z, Zhao JS, Li JJ, Peng DN, Wang XY, Chen TL, Oiu YP, Chen PP, Li WJ, Xu LY, Li EM, Tam JP, Oi RZ, Jia W, Xie D (2010) A combined proteomics and metabolomics profiling of gastric cardia cancer reveals characteristic dysregulations in glucose metabolism. Mol Cell Proteomics 9:2617–2628
Sjostrom L, Lindroos AK, Peltonen M, Hohenberger W, Husemann B, Horbach T (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351:2683–2693
Gunther K, Vollmuth J, Weissbach R, Hohenberger W, Huseman B, Horbach T (2006) Weight reduction after an early version of the open gastric bypass for morbid obesity: results after 23 years. Obes Surg 16:288–296
Ferrannini E, Gastaldelli A, Iozzo P (2011) Pathophysiology of prediabetes. Med Clin N Am 95:327–339
De Paula AL, Stival AR, Macedo A, Ribamar J, Mancini M, Halpern A, Vencio S (2010) Randomized controlled trial comparing 2 versions of laparoscopic ileal interposition associated with sleeve gastrectomy for patients with type 2 diabetes with BMI 21–34 kg/m2. Surg Obes Relat Dis 6:296–304
Boza C, Muñoz R, Yung E, Milone L, Gagner M (2011) Sleeve gastrectomy with ileal transposition (SGIT) induces significant weight loss and diabetes improvement without exclusion of the proximal intestine. J Gastrointest Surg 15:928–934
Cohen RV, Rubino F, Schiavon C, Cummings DE (2012) Diabetes remission without weight loss after duodenal bypass surgery. Surg Obes Relat Dis 8(5):e66–e68
Lee WJ, Chong K, Ser KH, Lee YC, Chen SC, Chen JC, Tsai MH, Chuang LM (2011) Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg 146:143–148
Talbot P, Dunbar MJ (2011) Nova Scotia Prediabetes Project: upstream screening and community intervention for prediabetes and undiagnosed type 2 diabetes. Chronic Dis Inj Can 32:2–11
Onat A, Can G, Cicek G, Ayhan E, Dogan Y, Kaya H (2011) Fasting, non-fasting glucose and HDL dysfunction in risk of pre-diabetes, diabetes and coronary disease in non-diabetic adults. Acta Diabetol. doi:10.1007/s00592-011-0313-x
Acknowledgments
This article has benefited from two Postgraduate CAPES Scholarships (Silvia Y. Hayashi and Camila M. Yamamoto) and from CNPq Scientific Investigator Grant 302915/2011-7 (Joel Faintuch).
Disclosures
Osmar K. Yagi, Jacob J. Faintuch, and Ivan Cecconello have no financial ties or conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration Identifier: NCT 01518023.
Rights and permissions
About this article
Cite this article
Hayashi, S.Y., Faintuch, J., Yagi, O.K. et al. Does Roux-en-Y gastrectomy for gastric cancer influence glucose homeostasis in lean patients?. Surg Endosc 27, 2829–2835 (2013). https://doi.org/10.1007/s00464-013-2829-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2829-3