Abstract
Background
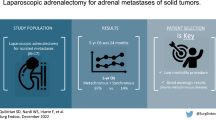
Laparoscopic adrenalectomy (LA) is the treatment of choice for benign adrenal lesions. Size of the lesion and radiologic features define the risk for malignancy. In lesions at high risk of malignancy, the experience with the laparoscopic approach is limited and therefore controversial. The purpose of this study was to determine the feasibility and oncological safety of LA for malignant disease.
Methods
Retrospective analysis of prospectively collected database. All LA performed in our department from 2003 to 2011 were reviewed and demographic, perioperative, and follow-up data for those who had malignancy in the final histological report was analyzed. Data are presented as mean ± standard deviation or median (range).
Results
Of 121 LA, we identified 20 patients with 21 malignant adrenal pathologies: 11 primary tumors, 5 adrenocortical carcinoma, 5 large B cell lymphoma, and 1 leiomyosarcoma. Ten metastatic lesions included 5 malignant melanoma (1 patient, both sides), 4 adenocarcinoma, and 1 renal cell carcinoma. There was no conversion to laparotomy. Tumor size was 4.5 (1–9.5) cm, operative duration was 79 (42–262) min, and estimated blood loss was 40 (0–250) ml. All patients resumed regular diet on postoperative day 1, and the median length of stay was 2 days after surgery. Two patients died at 6 and 24 months postoperatively. Three patients were lost to follow-up. All the rest of the patients were disease-free at a follow-up of 58 (7–96) months.
Conclusions
LA for primary or metastatic malignant lesions is feasible and seems oncologically safe. Surgical principles should be the same for all LA: en bloc resection of all epinephric fat, minimal touch technique, and low threshold for conversion. Size of the lesion alone should not be an indication for open surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since it was first introduced in 1992 by Gagner et al. [1], laparoscopic adrenalectomy (LA) has become the standard of care for hyperfunctioning adrenal lesions and nonfunctioning tumors larger than 4 cm at low suspicion for malignancy. The advantages of the laparoscopic approach over the traditional open approach in adrenal resections are clear and include less analgesic requirement, less blood loss, earlier recovery in terms of postoperative ileus, earlier resumption of regular diet, shorter length of hospital stay, and earlier return to work [2–5]. Nevertheless, the studies that have shown these advantages included patients with benign lesions only. As more surgeons have gained experience with the operative technique, indications for LA have expanded. The main concern while performing LA is the risk of capsule rupture and peritoneal carcinomatosis in the case of adrenocortical carcinoma (ACC).
Preoperative pathological diagnosis by fine needle biopsy is usually not indicated for an adrenal mass because of the risk of spreading cancer cells in ACC, as well as the low negative predictive value of this biopsy [4]. The only exception would be for patients with a history of cancer for whom the appropriate treatment might be nonsurgical. Over the years there have been attempts to define the risk of malignancy of an adrenal lesion by preoperative clinical and radiological evaluation alone. Factors that have been associated with higher risk of malignancy are size of the tumor, history of malignancy, and suspicious radiological features [6]. Attempts are made to define biochemical markers that would improve accuracy in the preoperative diagnosis of ACC [7]. Regarding size of the lesion, it is difficult to define the cutoff size for a lesion to be considered malignant. One should remember that most lesions larger than 6 cm are benign, and that malignant lesions can be discovered incidentally when they are smaller than 6 cm [8]. Because there are no randomized, controlled trials that address the issue of surgical approach to malignant adrenal lesions, there is a need to accumulate evidence from numerous sources in order to decide whether the laparoscopic approach is appropriate in suspected ACC or other malignancies of the adrenal.
The purpose of this study was to assess the feasibility and oncological safety of the laparoscopic approach for resection of malignant lesions of the adrenal, and contribute evidence by reporting a single center’s 8 years’ experience.
Methods
We conducted a retrospective analysis of our prospectively collected database. All LA performed at the department of surgery in Bnai-Zion Medical Center from July 2003 through December 2011 were reviewed, and demographic, perioperative, and follow-up data for those who had malignancy in the final histological report was analyzed. We also compared the perioperative data with that of the patients who were operated for benign disease. Data are presented as mean±standard deviation or mean (range). Student’s t test was used to compare the benign and malignant groups.
Surgical technique
Patients are placed in the lateral decubitus position. We use the anterolateral transperitoneal approach. The bed is flexed to allow opening of the costoiliac angle. We use four subcostal ports and a harmonic scalpel as an energy source. Ports are placed in an airtight fashion in order to prevent air leak during the operation (chimney effect). We use small sponge sticks for gentle retraction of the suprarenal fat or the lesion, with an emphasis on keeping the integrity of the lesion’s capsule through a minimal touch technique. The adrenal vein is secured on both sides with hemoclips. In all procedures, we resect all the suprarenal fat to its anatomical borders: the upper pole of the kidney, psoas muscle, liver, and inferior vena cava on the right, and the spleen, pancreatic tail, and left kidney vessels on the left. The tumor is always removed within an endobag through the lateral incision, which is enlarged according to the lesion size to ensure that the lesion is not squeezed and the endobag does not tear. We routinely leave no drains; the patient is allowed to start drinking the same evening and start eating the next day. Patients are discharged whenever they are able to resume their diet with no nausea or vomiting, and manage their pain with oral analgesics.
Follow-up
Follow-up data were obtained through chart review, telephone calls, and office visits to the oncology, hematology, and endocrinology clinics at our institution.
Results
One hundred twenty-one laparoscopic adrenal resections were performed in 118 patients during the study period. Of those, we identified 20 patients with 21 malignant adrenal pathologies. Table 1 compares patients with benign and malignant pathologies in our cohort in terms of demographic and perioperative data. Patients with malignant pathologies were 8 years older, on average, than patients with benign lesions; further, there were more men and more lesions on the right side. Malignant lesions were on average 8 mm larger than benign ones. In terms of the procedure itself, there were no differences in length of operation, estimated blood loss, or length of hospital stay. Table 2 provides the histological diagnosis of the malignant lesions in these patients as well as lesion size.
There were no conversions to laparotomy. Two patients had combined left adrenalectomy with laparoscopic colon resection due to colon cancer and suspected adrenal metastasis. The final diagnosis for one of them was indeed metastatic adenocarcinoma; the other had a nonfunctioning adenoma. Three more patients had combined surgery with their adrenalectomy, two for recurrent breast carcinoma and one had laparoscopic distal pancreatectomy for a lesion that turned out to be benign. All of them had benign adrenal histology.
Complications
Three patients who were operated for benign lesions had major complications: one patient with a cortisol-producing tumor had postoperative hypocortisolism that required large doses of corticosteroids and prolonged monitoring in the intensive care unit. The other was operated for pheochromocytoma and went through computed tomography–guided drainage of an infected hematoma 8 days after surgery. One patient with myelolipoma had postoperative myocardial infarction and was treated with urgent coronary intervention. One patient with malignant melanoma had partial ureteral obstruction and had to be reoperated for clip removal and placement of a ureteral stent. There was no perioperative mortality.
Follow-up
All five patients with large B cell lymphoma were treated accordingly and were in remission 64 (8–96) months after surgery. Of the patients with malignant melanoma, one had died from metastatic disease 6 months after surgery, one was free of disease at 62 months after surgery, and the one who was operated on both sides was free of disease 94 months after the first operation and 66 months after the second operation. This patient was operated again for a single retroperitoneal lymph node metastasis.
The patient with metastatic adenocarcinoma of the colon was disease-free 9 months after surgery. The patient with parotid adenocarcinoma, at 26 months after surgery, had brain metastasis, for which she received radiotherapy, with good response. The two patients who had metastatic lung cancer and the patient with metastatic renal cell carcinoma were free of disease at 84, 92, and 31 months after surgery, respectively. The patients with ACC were all treated with mitotane postoperatively. One of them died 24 months after surgery, and three patients were free of disease at 11, 20, and 58 months after surgery.
Three patients were lost to follow-up—the one with leiomyosarcoma, one patient with ACC, and one with malignant melanoma.
Discussion
Adrenal lesions should be treated surgically if they are clinically or biochemically active (functional) regardless of their size and regardless of whether they are likely to be malignant [4]. Preoperative diagnosis is usually not known because fine needle biopsy is not recommended in primary lesions suspected to be malignant. The most feared primary pathology of the adrenal is ACC, a rare tumor with a poor prognosis. Definitive preoperative diagnosis of ACC is impossible, and the risk of a lesion being an ACC depends on the size of the lesion and its radiographic appearance [9]. The prevalence of ACC in series of adrenal incidentalomas is 2 % in lesions <4 cm, 6 % in lesions 4–6 cm, and as high as 25 % in lesions >6 cm in diameter. The most commonly used histological algorithm for ACC is the Weiss score (0–9), which is highly correlated with aggressiveness of the disease and prognosis [10], but this score could only be obtained during complete histological evaluation of the tumor after surgery.
There is an ongoing debate in the last decade regarding the appropriate surgical approach for large and potentially malignant adrenal tumors. Table 3 summarizes recent selected reports of laparoscopically resected ACCs. MacGillivray et al. have shown that it is safe to resect tumors >6 cm if they are well defined with no signs of local invasion. Of the 12 patients who were operated with large tumors, only one had ACC (a well-encapsulated 9-cm tumor). They stated that the size of the tumor should not be the primary factor in determining the surgical approach [11]. Henry et al. selected 19 patients with solid tumors >6 cm and excluded any large benign-appearing lesions. Six patients had ACC on final histology. In two of these patients, there was an early conversion to laparotomy as a result of dense adhesions and unusual and numerous retroperitoneal feeding vessels. All the ACC patients had a complete resection with no capsular disruption. For the patients who were operated laparoscopically, the authors stated that they would not have performed more extensive surgery through an open approach [12]. Ramacciato et al. presented their experience with adrenal masses >7 cm. Of the 18 patients in their series, four had malignant disease; two had ACC and two had metastasis (colon and renal cell carcinoma). The ACC patients were disease-free 45 months after surgery [13].
An international consensus conference was held in 2003 at the University of Michigan in Ann Arbor regarding the management of patients with adrenal cancer. The recommendations were based on the available literature and the participants’ experience. The recommendations stated that there is no role for laparoscopic removal of a known or likely ACC, but there is controversy about the role of laparoscopic removal of indeterminate incidentalomas that could admittedly be small ACCs. Also recommended were open resection of any lesion over 6 cm or with clear imaging characteristics of malignancy, laparoscopic approach for lesions 4–6 cm in size, and conversion to open resection with any intraoperative evidence of malignancy [14]. In 2005, Shen et al. reviewed the management of adrenal tumor according to their diagnosis. Regarding ACC, they concluded that there is a minimal role for the laparoscopic technique in adrenal cortical tumors with invasion to adjacent organs, enlarged regional lymph nodes, or size >10–12 cm [15].
In our point of view, this debate comes down to the question whether the adrenal tumor can be resected in an appropriate fashion, with no oncological compromise due to surgical technique. There are a few recent reports that looked specifically into ACC and surgical approach. Leboulleux et al. conducted a retrospective cohort study of 64 ACC patients with a main outcome of peritoneal carcinomatosis. They found that the only risk factor for the development of peritoneal carcinomatosis was surgical approach. During 4 years of follow-up, it occurred in four of six patients who were treated with LA and only in 11 of 55 who were operated via an open approach. Tumor size was not found to be a risk factor for peritoneal carcinomatosis [16]. It is important to note, however, that the six LA were performed by five different surgeons in five different hospitals. Another report by Miller et al. identified 88 ACC patients who were operated with a curative intent, 17 of them by LA. Half of the patients who were operated laparoscopically had positive margins or intraoperative tumor rupture. This fact alone can explain their results showing a shorter time to recurrent disease in the LA group (9.6 months) than in the open group (19.2 months). It seems that there is a large selection bias in their report because all patients who had been operated laparoscopically were referred to the author’s institution after surgery [17].
On the other hand, several authors have shown that laparoscopic resection of stage I and II ACC is comparable to open surgery in oncological outcome. Porpiglia et al. analyzed 43 ACC patients who were operated with curative intent. Recurrence rates and recurrence-free survival were no different in the LA and open groups (50 and 64 %; and 23 vs. 18 months, respectively) [18]. The largest series of ACC patients by Brix et al. included 152 stage I–III patients with tumors ≤10 cm. In this study, each of the 35 patients who were operated by LA, was matched with a patient who was operated by an open approach, according to tumor stage, size of tumor, adjuvant therapy, age, and steroid excess. The major finding of their analysis was a similar oncological outcome after LA and open approach [19]. This debate is expressed clearly by a union of the groups from Turin and Michigan. They agreed that surgery for suspected ACC should be limited to experienced surgeons at referral centers and that oncologically appropriate surgical resection is of the utmost importance [20]. Another review by Carnaille summarizes the literature regarding the surgical approach in ACC. Carnaille concluded that tumor size is not necessarily a limiting factor for LA as long as the tumor can be completely resected. In cases where local invasion is found or oncological principles cannot be met, conversion to open surgery is recommended [21].
Our study is a retrospective cohort and therefore has the same limitations as many of the series that were discussed: a small and heterogeneous group of patients, and no ability to compare the LA approach with the open approach. Our department serves as a referral center for laparoscopic cases, and thus selection bias is inevitable. We have no data regarding other patients who might have been operated by an open approach elsewhere for large adrenal tumors. A total of 29 % of the malignant tumors in our series (6 of 21) were ≥6 cm, compared to 13 % of the benign tumors. On the other hand, out of all the large tumors ≥6 cm, two-thirds were benign (13 of 19), so we agree that a size of ≥6 cm should not be a contraindication to LA. One should take into account the risk factors for malignancy as were expressed by Wright et al. [6]—suspicious radiological appearance, history of malignancy, and, of course, the size of the lesion. In patients with a history of malignancy and suspected metastatic adrenal lesion, there is no reason not to operate laparoscopically, and a combined procedure with another abdominal operation is feasible. We had two patients who had LA combined with colectomy and one with distal pancreatectomy. One of the colon patients turned out to have adrenal metastasis. The other two had nonfunctioning adenomas. In these cases, prognosis would be related to the primary malignancy. When addressing a suspected malignant adrenal tumor laparoscopically, one must be meticulous about the anatomical plains of dissection in order to achieve an R0 resection—exactly as in open surgery. Whenever there is a chance of oncologic compromise, there should be an early conversion to open approach. In our series, one of the five ACC patients with a 4-cm tumor had a violation of the capsule according to the pathological report. This capsule injury was not noticed during the operation; it was assumed to have taken place during the handling of the specimen extracorporeally. This patient received mitotane treatment and was disease-free 12 months after surgery.
Conclusions
Our study contributes evidence that LA for primary or metastatic malignant lesions is feasible and seems oncologically safe as long as surgical principles are kept meticulously by an experienced surgical team. These principles include en bloc resection of all epinephric fat, a minimal touch technique, and a low threshold for conversion in cases of unclear plane of dissection or local invasion of the tumor to surrounding structures. We believe that the size of the tumor alone should not be an indication for open surgery.
References
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327(14):1033
Brunt LM, Doherty GM, Norton JA, Soper NJ, Quasebarth MA, Moley JF (1996) Laparoscopic adrenalectomy compared to open adrenalectomy for benign adrenal neoplasms. J Am Coll Surg 183(1):1–10
Prinz RA (1995) A comparison of laparoscopic and open adrenalectomies. Arch Surg 130(5):489–492
National Institutes of Health (2002) State-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens State Sci Statements 19(2):1–25
Jacobs JK, Goldstein RE, Geer RJ (1997) Laparoscopic adrenalectomy. A new standard of care. Ann Surg 225(5):495–501
Wright L, Nordenstrom E, Almquist M (2012) Determinants for malignancy in surgically treated adrenal lesions. Langenbecks Arch Surg 397(2):217–223
Kouyama R, Hiraishi K, Sugiyama T, Izumiyama H, Yoshimoto T, Akashi T, Kihara K, Homma K, Shibata H, Hirata Y (2011) Clinicopathological features, biochemical and molecular markers in 5 patients with adrenocortical carcinoma. Endocr J 58(7):527–534
Corcione F, Miranda L, Marzano E, Capasso P, Cuccurullo D, Settembre A, Pirozzi F (2005) Laparoscopic adrenalectomy for malignant neoplasm: our experience in 15 cases. Surg Endosc 19(6):841–844
Zeiger MA, Thompson GB, Duh QY, Hamrahian AH, Angelos P, Elaraj D, Fishman E, Kharlip J, American Association of Clinical Endocrinologists, American Association of Endocrine Surgeons (2009) American association of clinical endocrinologists and American association of endocrine surgeons medical guidelines for the management of adrenal incidentalomas: executive summary of recommendations. Endocr Pract 15(5):450–453
Weiss LM, Medeiros LJ, Vickery AL Jr (1989) Pathologic features of prognostic significance in adrenocortical carcinoma. Am J Surg Pathol 13(3):202–206
MacGillivray DC, Whalen GF, Malchoff CD, Oppenheim DS, Shichman SJ (2002) Laparoscopic resection of large adrenal tumors. Ann Surg Oncol 9(5):480–485
Henry JF, Sebag F, Iacobone M, Mirallie E (2002) Results of laparoscopic adrenalectomy for large and potentially malignant tumors. World J Surg 26(8):1043–1047
Ramacciato G, Mercantini P, La Torre M, Di Benedetto F, Ercolani G, Ravaioli M, Piccoli M, Melotti G (2008) Is laparoscopic adrenalectomy safe and effective for adrenal masses larger than 7 cm? Surg Endosc 22(2):516–521
Schteingart DE, Doherty GM, Gauger PG, Giordano TJ, Hammer GD, Korobkin M, Worden FP (2005) Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr Relat Cancer 12(3):667–680
Shen WT, Sturgeon C, Duh QY (2005) From incidentaloma to adrenocortical carcinoma: the surgical management of adrenal tumors. J Surg Oncol 89(3):186–192
Leboulleux S, Deandreis D, Al Ghuzlan A, Aupérin A, Goéré D, Dromain C, Elias D, Caillou B, Travagli JP, De Baere T, Lumbroso J, Young J, Schlumberger M, Baudin E (2010) Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur J Endocrinol 162(6):1147–1153
Miller BS, Ammori JB, Gauger PG, Broome JT, Hammer GD, Doherty GM (2010) Laparoscopic resection is inappropriate in patients with known or suspected adrenocortical carcinoma. World J Surg 34(6):1380–1385
Porpiglia F, Fiori C, Daffara F, Zaggia B, Bollito E, Volante M, Berruti A, Terzolo M (2010) Retrospective evaluation of the outcome of open versus laparoscopic adrenalectomy for stage I and II adrenocortical cancer. Eur Urol 57(5):873–878
Brix D, Allolio B, Fenske W, Agha A, Dralle H, Jurowich C, Langer P, Mussack T, Nies C, Riedmiller H, Spahn M, Weismann D, Hahner S, Fassnacht M, German Adrenocortical Carcinoma Registry Group (2010) Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur Urol 58(4):609–615
Porpiglia F, Miller BS, Manfredi M, Fiori C, Doherty GM (2011) A debate on laparoscopic versus open adrenalectomy for adrenocortical carcinoma. Horm Cancer 2(6):372–377
Carnaille B (2012) Adrenocortical carcinoma: which surgical approach? Langenbecks Arch Surg 397(2):195–199
Disclosures
Drs. Sroka, Slijper, Shteinberg, Mady, Galili, and Matter have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sroka, G., Slijper, N., Shteinberg, D. et al. Laparoscopic adrenalectomy for malignant lesions: surgical principles to improve oncologic outcomes. Surg Endosc 27, 2321–2326 (2013). https://doi.org/10.1007/s00464-012-2772-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2772-8