Abstract
Background
Current surgical training involves integration of educational interventions together with service requirements during regular working hours. Studies have shown that voluntary training has a low acceptance among surgical trainees and obligatory simulation training during the regular working week leads to better skill acquisition and retention. We examined the difference in training effectiveness depending on the time of day.
Methods
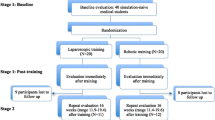
Surgical novices underwent a curriculum consisting of nine basic laparoscopic tasks. The subjects were permitted to choose a training session between during regular working hours (8:00–16:00) or after hours (16:00–20:00). Each subject underwent baseline and post-training evaluation after completion of two 4-h sessions. Task completion was measured in time (s), with penalties for inaccurate performance. Statistical analysis included matched-pairs analysis (sex, age, and previous operative experience) with χ2 und Mann–Whitney U test for between groups and Wilcoxon signed-rank test for testing within one group.
Results
There were no differences in demographic characteristics between the groups. Comparison of the individual baseline and post-training performance scores showed a significant (P < 0.05) improvement for all subjects in all exercises. No significant differences between groups were observed.
Conclusion
All subjects improved in skill significantly throughout the week regardless of the timing of the training intervention. Simulation training can be offered outside of regular working hours with acceptable effectiveness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Factors associated with a higher risk of surgical adverse outcome and complications have been extensively examined but still remain controversial. Studies have implied that insufficient experience is associated with an increased number of technical errors and potentially poorer clinical outcomes [1] and have tried to examine the learning curves for various laparoscopic procedures [2–4]. In the education of surgical novices, multiple training concepts have been validated and can be used for training and proficiency testing [5–9]. Simulation training of junior surgeons has been implemented by numerous surgical residency programs in North America and Europe [10, 11]. Nevertheless, the growing service requirements and the need to adhere to work-hour regulations make integration of additional simulation training into the work week difficult. Attention and memory are known to fluctuate throughout the day and multiple factors influencing performance have been investigated [12]. Recent research showed that in motor skills acquisition of a basic task, the component of declarative learning was influenced by the time of day, with better results in the morning, whereas the kinematic component of motor skills acquisition was independent of time of day [13]. Whether this applies to the learning of a more complex motor skill such as required in laparoscopic surgery has not yet been investigated. We conducted this study to evaluate whether “after hours” simulation training is less effective than training during core working hours.
Methods
Participants
Of the 36 senior medical students participating in a basic laparoscopic skills course at a university hospital between 2007 and 2010, 24 were included in this study. Informed consent was obtained from the participants for the analysis of the data obtained during the course.
Each course was split into three time periods: 8:00–12:00, 12:00–16:00, and 16:00–20:00. The students were able to select a time slot for their training, wherein each slot was open to four students within each course. Once allocated a session, the students formed pairs and no changes between groups were allowed. Furthermore, the subjects were not afforded the opportunity to practice between sessions. A questionnaire on demographic data and prior surgical experience was completed by each participant. Previous experience was rated on a 5-point Likert scale, with 5 being no experience and 1 being very experienced. For the purpose of this study, regular working hours were defined as 8 am to 4 pm.
Course design and tasks
All participants completed a structured 5-day curriculum [14]. The course commenced with an introduction theory tutorial regarding laparoscopic techniques, equipment handling, and an explanation of the course’s tasks. The next day baseline (BL) evaluation with repetition of each task twice without further instruction was performed. The two following days were training sessions with a total of four course cycles performed by each pair. The curriculum consisted of nine basic laparoscopic tasks performed twice a day by each participant. Four of these tasks were modifications of established tasks used in validated curricula [5, 15–17]. For evaluation purposes, the tasks were classified as easy (E), moderate (M), or hard (H) [14]. The tasks were camera navigation (M), grasping (E), cube positioning (M), pattern cutting (M), loop tying (M), extra- and intracorporeal knot tying (H), and clipping (E). The task repetitions were combined with intensive individual coaching, feedback, and demonstrations by an expert for each student pair. The same four tutors took part throughout the course, each rotating through the workstations to ensure equal coaching of all participants. Post-training (PT) assessment included performance of each task twice on the last day of the course (Fig. 1).
Performance measure and scoring
Each trial of the task was assessed quantitatively (time in seconds), with an additional error score applied for incorrect or inaccurate execution (error score). Errors were communicated to the participants during the introduction session. During scoring each error was registered and later converted to penalty points. Minor errors such as deviation from marked targets were penalized with 1 s per millimeter, whereas more substantial errors such as loose knots, sliding knots, gap formation between cloth pieces, and leakage from clipped tubing were penalized with 10 s (per leaking side in the clip task). Each task was limited to 300 s. All unfinished tasks could be completed by the student during the training sessions without cutoff scoring; during evaluation testing the task was aborted and scored with 300 s.
Statistical analysis
Nonparametric testing was used. Demographic data were evaluated with Fisher’s exact test for categorical data and Mann–Whitney’s U test for continuous variables. Performance scores between groups and within groups were compared using Mann–Whitney’s and Wilcoxon signed-rank tests, respectively.
The 12 participants of the “after hours” group (AH) were individually matched with 12 participants of the “regular hours” group (RH). Matching criteria were demographic details such as sex, age (±2 years), semester (±1 semester), operative experience self-rating score (±1 point), and previous experience with camera navigation self-rating score (±1 point). Significance was defined as P < 0.05. Statistical evaluation was performed with the Statistical Package for Social Sciences (SPSS)® 17.0 (SPSS Inc., Chicago, IL).
Results
Demographics
BL and PT data were available for all 36 course participants. Twenty-four participants were trained during RH (8:00–12:00 and 12:00–16:00) and 12 participants were trained AH (16:00–20:00). Prior to matching, the groups differed significantly with respect to gender (RH: 11 male and 13 female; AH: 10 male and 2 female; P = 0.04). No significant differences were found in the general demographic characteristics or in previous surgical experience of the groups after matching (Table 1). All selected students stated an interest in a future surgical career. None were currently employed in night-shift work.
Task performance
For all tasks, except for the positioning task, the BL values between the groups showed no significant differences (Table 2). Comparison of PT and BL values in both groups after completing the training course showed that task performance was significantly improved in both groups after training in all nine tasks (P < 0.05) (Figs. 2, 3, 4). There were no significant differences in values between the groups after training (Table 3).
Baseline (BL) and post-training (PT) results between study groups. RH regular hours (8:00–16:00), AH after hours (16:00–20:00). Easy tasks (grasping and clipping) depicted as box plots, with the horizontal bar representing median and boxes representing 25th and 75th percentile; whiskers mark 10th and 90th percentile
Baseline (BL) and post-training (PT) results between study groups. RH regular hours (8:00–16:00), AH after hours (16:00–20:00). Moderate tasks (camera navigation, transfer, cube positioning, pattern cutting, and loop tying) depicted as box plots, with horizontal bar representing median and boxes representing 25th and 75th percentile; whiskers mark 10th and 90th percentile
Baseline (BL) and post-training (PT) results between study groups. RH regular hours (8:00–16:00), AH after hours (16:00–20:00). Hard tasks (extra- and intracorporeal knot tying) depicted as box plots, with horizontal bar representing median and boxes representing 25th and 75th percentile; whiskers mark 10th and 90th percentile
Discussion
The aim of this study was to evaluate whether the time of day influences acquisition of basic laparoscopic skills. The results showed that all participants significantly improved in skill throughout the training irrespective of what time of day the training was conducted. No differences were observed between the groups in regard to post-training skill levels.
Previous research has suggested that learning curves could be shortened by simulation training, introducing the concept of the “pretrained novice” [18–20]. Currently, basic laparoscopic training to benchmarked proficiency is integrated into several validated curricula such as the Fundamentals of Laparoscopic Surgery (FLS) [5]. Maintenance of proficiency, however, requires ongoing practice [21] and additional refresher training is of great importance in long-term skill retention [22]. Although simulation training has been shown to enhance surgical skill, it is necessary to integrate this form of training into formal curricula since it has been shown that voluntary training has low acceptance among residents [23, 24]. Chang et al. [23] showed that after introduction of virtual reality simulation into resident curriculum only 31 % of eligible residents used the simulator on a voluntary basis at least once throughout the following 3 months. One of the main reasons stated for not using the simulator more frequently was lack of time. A Dutch study on the same topic showed similar results. In the first 4 months of the study, only 10 % of eligible residents trained on the simulator after being granted unrestricted access [24]. Again, the reason stated by this group for not conducting voluntary training was lack of time. In this group, work hours had been limited to 48 h/week to comply with European work-hour legislation. The majority of time spent on the simulator when residents did practice was during the night shift. No training was conducted during personal time. Forty percent of the residents suggested mandatory integration of the training.
Planning and integrating curricular training poses several challenges. Most clinical educators agree that training curricula should be available to all residents in a unit without causing a disruption of daily resident routines and without further reducing time for training in the OR while abiding by work-hour regulations. The findings from this study in regard to overall skill acquisition showed that there was no negative effect associated with an “after hours” session. For the purpose of this study, we defined “regular working hours” based on the hours considered core working hours in our hospital for medical staff. This definition may naturally vary between departments. “After hours” was considered to be between 4 pm and 8 pm. Since work-hour regulations and resident rostering vary greatly between countries and programs, many units may consider this after-hours time frame to be within their regular working hours. Declarative learning appears to be influenced by circadian rhythm, with better results when learning sessions are conducted in the morning. However, Kvint et al. [13] showed that kinematic learning as a component of motor skill acquisition was independent of time of day. The results from our study also support these findings since the level of skill acquisition did not vary throughout the day, and therefore a training session in the afternoon or evening can be equally effective as a morning session.
Finally, when evaluating the data it is important to consider quality-of-life issues and fatigue. There still remains much debate about the effects of fatigue on motor skill, mental work load, and error rate. A number of studies focusing on motor skills did not show a significant negative effect of fatigue on task execution or skill acquisition [25, 26]. On the other hand, negative effects on dexterity, error rate, mental workload, and cognitive function have also been described [26–28]. In our study, participants had no regular curricular obligations and went about normal daily activities, including part-time work. None of the participants were on night shifts. Nevertheless, we did not explicitly evaluate individual alertness nor did we question what the students did the evening before training. Therefore, we cannot exclude the possibility that participants in either group may have been more fatigued than others. This represents one limitation of this study and results in a resident group could well be different. Additionally, this student group potentially differs from more senior residents, especially in regard to overall motivation to participate. This course was a voluntary skills training course and represented the first opportunity for structured exposure to surgical skills. The students in this group were all highly motivated. This motivating effect may be less strong in a more senior resident group who have a heavy workload and potentially the novelty of such a course may have worn off with respect to basic skills. Therefore, it seems appropriate to offer more senior residents skill tasks that still challenge them and that may spark similar enthusiasm.
Furthermore, the students were permitted to choose a training session and were not randomized to a specific group. A higher number of male participants registered for the after-hours session. In order to exclude this potential gender factor, matched-pairs analysis was performed thus reducing the number of evaluated subjects. Since the matched group was demographically homogeneous and factors such as parallel ongoing training and exposure to surgical procedures could be excluded, we believe that the groups were comparable and suited for investigating the influence of the time of training on the basic skill learning curves.
Lastly, we did not address the issue of independent practice in this study since we first wished to investigate whether any negative effects of after-hours training session could be shown in a controlled experimental design. In order to limit confounding factors such as variability of duration, intensity, and timing of independent training sessions, we chose a standardized curriculum. This study therefore does not answer the question regarding independent skills practice and acquisition during an after-hours session, which may well show different results. To address this controversial topic further research is required.
Conclusion
Although the concept of training on “personal time” is a sensitive topic, we believe that with introduction of the work-hour directives across Europe, this topic will become very important. Furthermore, although many questions remain unanswered, this study addressed a very important question and was able to demonstrate that there was no difference in skill acquisition between groups trained in the morning or early afternoon compared to an evening group. All trainees acquired the basic laparoscopic skill irrespective of the time of training. This is important for educators because it allows for more flexibility in the planning of training sessions for residents in order to accommodate very diverse resident schedules. In contrast to declarative learning, there is no obvious disadvantage to afternoon or evening sessions in motor skill acquisition.
References
Prystowsky JB (2005) Are young surgeons competent to perform alimentary tract surgery? Arch Surg 140:495–500
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23:622–628
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum 46:1371–1388
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525
Rosser JC Jr, Rosser LE, Savalgi RS (1998) Objective evaluation of a laparoscopic surgical skill program for residents and senior surgeons. Arch Surg 133:657–661
Keyser EJ, Derossis AM, Antoniuk M, Sigman HH, Fried GM (2000) A simplified simulator for the training and evaluation of laparoscopic skills. Surg Endosc 14:149–153
Risucci D, Geiss A, Gellman L, Pinard B, Rosser J (2001) Surgeon-specific factors in the acquisition of laparoscopic surgical skills. Am J Surg 181:289–293
Scott DJ, Young WN, Tesfay ST, Frawley WH, Rege RV, Jones DB (2001) Laparoscopic skills training. Am J Surg 182:137–142
Korndorffer JR Jr, Stefanidis D, Scott DJ (2006) Laparoscopic skills laboratories: current assessment and a call for resident training standards. Am J Surg 191:17–22
Bonrath EM, Buckl L, Bruwer M, Senninger N, Rijcken E (2012) Education in laparoscopic surgery: national survey on current strategies and relevance of simulation training. Zentralbl Chir 137(2):160–164
Schmidt C, Collette F, Cajochen C, Peigneux P (2007) A time to think: circadian rhythms in human cognition. Cogn Neuropsychol 24:755–789
Kvint S, Bassiri B, Pruski A, Nia J, Nemet I, Lopresti M, Perfetti B, Moisello C, Tononi G, Ghilardi MF (2011) Acquisition and retention of motor sequences: the effects of time of the day and sleep. Arch Ital Biol 149:303–312
Bonrath EM, Weber BK, Fritz M, Mees ST, Wolters H, Senninger N, Rijcken E (2012) Laparoscopic simulation training: testing for skill acquisition and retention. Surgery 152(1):12–20
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17:964–967
Vassiliou MC, Ghitulescu GA, Feldman LS, Stanbridge D, Leffondre K, Sigman HH, Fried GM (2006) The MISTELS program to measure technical skill in laparoscopic surgery: evidence for reliability. Surg Endosc 20:744–747
Fried GM, Derossis AM, Bothwell J, Sigman HH (1999) Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator. Surg Endosc 13:1077–1081 discussion 1082
Van Sickle KR, Ritter EM, Smith CD (2006) The pretrained novice: using simulation-based training to improve learning in the operating room. Surg Innov 13:198–204
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463
Edelman DA, Mattos MA, Bouwman DL (2010) FLS skill retention (learning) in first year surgery residents. J Surg Res 163:24–28
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 202:599–603
Chang L, Petros J, Hess DT, Rotondi C, Babineau TJ (2007) Integrating simulation into a surgical residency program: is voluntary participation effective? Surg Endosc 21:418–421
van Dongen KW, van der Wal WA, Rinkes IH, Schijven MP, Broeders IA (2008) Virtual reality training for endoscopic surgery: voluntary or obligatory? Surg Endosc 22:664–667
Uchal M, Tjugum J, Martinsen E, Qiu X, Bergamaschi R (2005) The impact of sleep deprivation on product quality and procedure effectiveness in a laparoscopic physical simulator: a randomized controlled trial. Am J Surg 189:753–757
Tomasko JM, Pauli EM, Kunselman AR, Haluck RS (2012) Sleep deprivation increases cognitive workload during simulated surgical tasks. Am J Surg 203:37–43
Kahol K, Leyba MJ, Deka M, Deka V, Mayes S, Smith M, Ferrara JJ, Panchanathan S (2008) Effect of fatigue on psychomotor and cognitive skills. Am J Surg 195:195–204
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2001) Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ 323:1222–1223
Acknowledgments
This work was funded by a Grant from Rolf Dierichs-Stiftung Muenster 2008 to ER and EB.
Disclosures
Drs. Esther Bonrath, Mathias Fritz, Soeren T. Mees, Barbara K. Weber, Teodor P. Grantcharov, Norbert Senninger, and Emile Rijcken have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonrath, E.M., Fritz, M., Mees, S.T. et al. Laparoscopic simulation training: does timing impact the quality of skills acquisition?. Surg Endosc 27, 888–894 (2013). https://doi.org/10.1007/s00464-012-2529-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2529-4