Abstract
Background
The aim of this study was to compare outcome measures between conventional transabdominal laparoscopic adrenalectomy and single-incision laparoscopic adrenalectomy (SILA).
Methods
Between January 2006 and April 2010, a total of 96 patients underwent laparoscopic adrenalectomy. Of these, 74 (77.1%) underwent conventional transabdominal laparoscopic adrenalectomy (group 1) and 22 (32.9%) underwent SILA (group 2). Age, sex ratio, tumor size, operating time, blood loss, postoperative visual analog pain scale (VAS) scores, and duration of hospitalization were compared between the two groups.
Results
The mean ages of the patients in groups 1 and 2 were 43.4 ± 12.3 and 43.3 ± 10 years, respectively (P = 0.7). The female:male ratios in groups 1 and 2 were 1.6:1 and 4.5:1, respectively (P < 0.0001). The mean tumor size was significantly larger in group 1 than in group 2 (4.7 ± 1.5 vs. 3.34 ± 1.06 cm, respectively; P = 0.093). No significant difference was found between group 1 and group 2 with respect to the mean operating time (68.4 ± 20.8 vs. 63.9 ± 16.9 min, respectively; P = 0.36) or the level of intraoperative blood loss (38 ± 26.5 vs. 48.4 ± 62.4 ml, respectively; P = 0.26). The postoperative VAS score was significantly lower in group 2 than in group 1 (2.05 ± 0.57 and 3.28 ± 0.63, respectively; P < 0.0001). The length of hospital stay was significantly higher in group 1 than in group 2 (3.04 ± 1.2 and 2.45 ± 0.96 days, respectively; P = 0.04).
Conclusion
The findings of the present study suggest that SILA is as safe as conventional transabdominal laparoscopic adrenalectomy. Furthermore, SILA is associated with less pain and better cosmesis than the conventional laparoscopic procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The introduction of laparoscopic surgery has heralded a trend toward less invasive techniques and scarless surgery. The most prominent of these techniques are transumbilical single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES). NOTES is associated with numerous technical difficulties [1], and SILS has therefore attracted wider interest and popularity. This technique represents a safe alternative to NOTES, and may be used to complement standard laparoscopy in a range of surgical procedures [2–12]. However, the application of SILS is also restricted by various technical difficulties as well as a lack of suitable instrumentation.
Since its first description in 1992 by Gagner et al. [13], laparoscopic adrenalectomy has become the gold standard surgical approach for adrenal adenomas and has virtually replaced open adrenalectomy. Laparoscopic surgery for adrenal lesions has been shown to result in less pain, shorter hospital length of stay, faster recovery, and superior cosmesis. To date, only a few reports of single-incision laparoscopic adrenalectomy (SILA) have been published [14–17]. Despite residual controversies, these reports suggest that SILA may limit the morbidity and enhance the advantages of traditional laparoscopy.
The aim of the present retrospective study was to compare outcome measures between conventional transabdominal laparoscopic adrenalectomy and SILA.
Materials and methods
Between January 2006 and April 2010, a total of 96 patients underwent laparoscopic adrenalectomy in the Department of General Surgery of the Istanbul University Faculty of Medicine. Of these, 74 (77.1%) underwent conventional transabdominal laparoscopic adrenalectomy (group 1) and 22 (32.9%) underwent SILA (group 2). Age, sex ratio, tumor size, operating time, blood loss, postoperative visual analog pain scale (VAS) scores, and duration of hospitalization were compared between the two groups.
Surgical technique
Conventional transabdominal laparoscopic adrenalectomy
Patients were placed in the semilateral decubitus position, and the side with the lesion was elevated to 60°. A 10-mm trocar for the laparoscope was inserted along the midclavicular line at the level of the umbilicus. Two additional 5- or 10-mm trocars were inserted along the anterior axillary line and the midaxillary line, respectively, at points 2 cm below the costal margin. For left-sided tumors, adrenalectomy was performed through three trocars. For right-sided tumors, a fourth 5- or 10-mm trocar was inserted immediately below the xyphoid process for the purpose of liver retraction. Standard hand instruments and a 10-mm 30° lens laparoscope were used in all procedures. An incision was made in the peritoneum and Gerota’s fascia through the retroperitoneum and the adrenal gland was identified. The adrenal vein was then either clipped or sealed using a vessel-sealing system (Harmonic Ace, Ethicon Endo-Surgery, Cincinnati, OH, USA; or Ligasure, Covidien, Norwalk, CT, USA). The adrenal gland was excised together with the periadrenal fatty tissue and the specimen was extracted in a specimen bag.
Single-incision laparoscopic adrenalectomy (SILA)
Patients were placed in the semilateral decubitus position and the side with the lesion was elevated to 45°. The operative equipment included a SILS port (Covidien), a rigid 5-mm 30° lens laparoscope (Karl Storz, Tuttlingen, Germany), standard articulating hand instruments, 5-mm endoclips, and a vessel-sealing system (Harmonic Ace or Ligasure). The SILS port was placed through a 2-cm umbilical incision. For left-sided tumors, three standard trocars of the SILS port were used (Fig. 1). For right-sided tumors, an additional trocar was required for liver retraction, and the insufflation pipe of the SILS port was therefore replaced with a standard 5- or 10-mm trocar (Fig. 2). An incision was made in the peritoneum and Gerota’s fascia through retroperitoneum and the adrenal gland was identified. The adrenal vein was then either clipped or sealed using a vessel-sealing system (Harmonic Ace or Ligasure) (Fig. 3). The adrenal gland was excised together with the periadrenal fatty tissue, and the specimen was extracted in a specimen bag. The umbilical incision was closed either subcutaneously or with separated polypropylene sutures (Fig. 4).
Results
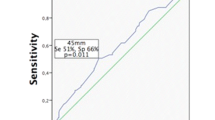
In both groups, the most common indication for surgery was pheochromocytoma, followed by Cushing’s syndrome (Table 1). The mean ages of the patients in groups 1 and 2 were 43.4 ± 12.3 and 43.3 ± 10 years, respectively (P = 0.7). The female:male ratios in groups 1 and 2 were 1.6:1 and 4.5:1, respectively (P < 0.0001). The mean tumor size was significantly larger in group 1 than in group 2 (4.7 ± 1.5 vs. 3.34 ± 1.06 cm, respectively; P = 0.093). No significant difference was found between group 1 and group 2 with respect to the mean operating time (68.4 ± 20.8 vs. 63.9 ± 16.9 min, respectively; P = 0.36) or the level of intraoperative blood loss (38 ± 26.5 vs. 48.4 ± 62.4 ml, respectively; P = 0.26). Postoperative analgesia consisted of intravenous administration of the nonsteroidal anti-inflammatory drug tenoksikam, including 40 mg on the day of operation and 20 mg on the first postoperative day. There was no additional demand for analgesia from patients in both groups. The postoperative VAS score was significantly lower in group 2 than in group 1 (2.05 ± 0.57 and 3.28 ± 0.63, respectively; P < 0.0001). All patients returned to oral intake within 6 h after adrenalectomy. Patient hospital discharge criteria included no gastrointestinal discomfort symptoms (nausea or vomiting) and maintenance of oral corticosteroid replacement therapy in patients operated on for Cushing’s syndrome. The length of hospital stay was significantly longer for group 1 than for group 2 (3.04 ± 1.2 vs. 2.45 ± 0.96 days, respectively; P = 0.04). No postoperative complications occurred in either group.
Discussion
The present retrospective study compared operating time, blood loss, postoperative VAS scores, and duration of hospitalization of patients who underwent conventional transabdominal laparoscopic adrenalectomy and patients who underwent SILA. The most important finding of the present study was the lower postoperative VAS score in the SILA group compared to the conventional laparoscopy group.
During the last two decades, laparoscopic surgery has largely supplanted the use of conventional open surgical techniques. Although the specific benefits vary according to the precise nature of the procedure, laparoscopy is widely recognized as being associated with reduced postoperative pain, a faster recovery, shorter hospitalization, and superior cosmesis. Surgeons have attempted to reduce the size and the number of ports used during laparoscopic procedures to improve the cosmesis and to decrease access-related morbidity such as hemorrhage, incisional hernia, and organ damage. NOTES eliminates the need for transabdominal incisions entirely, and SILS allows the performance of laparoscopic procedures through a single umbilical incision. However, NOTES is technically challenging and improvements in the instrumentation used are required [1]. SILS is associated with fewer of these problems and has thus gained wider popularity for procedures such as appendectomy, cholecystectomy, splenectomy, nephrectomy, colorectal surgery, bariatric surgery, and adrenalectomy [2–17]. Although difficulties with reduced triangulation, fog evacuation, and clashing of the instruments have been described in various studies, these procedures are technically successful and the results indicate that this surgical approach is feasible.
The first SILA was performed by Castelluci et al. in 2008. They performed single-port transperitoneal adrenalectomy by introducing three 5-mm trocars through a 2-cm subcostal incision [14]. The first single-multilumen-port (triport) left transperitoneal adrenalectomy was reported by Cindolo et al. in 2009 [15]. They performed a single-site transperitoneal adrenalectomy through a 3-cm subcostal incision to excise a 4-cm nonfunctional adrenal mass.
The first matched case-control study was reported by Jeong et al. in 2009 [16]. They compared nine patients who had undergone laparoendoscopic single-site adrenalectomy (LESS) with 17 patients who had undergone conventional laparoscopic adrenalectomy. The authors used a self-manufactured single-port device and a 5-mm flexible laparoscope. They found no significant difference in mean operating time or duration of postoperative hospital stay between the LESS and conventional laparoscopy groups. However, the degree of postoperative pain was significantly lower in the LESS group than in the conventional laparoscopy group. The authors concluded that LESS adrenalectomy is a safe technique that results in a superior cosmetic outcome and has the additional advantage of being minimally invasive.
The main technical problems encountered during the performance of SILA in the present study were the need for a fourth port for right-sided tumors, clashing of the instruments, and difficulties in fog evacuation. The fourth port was provided by replacing the insufflation pipe of the SILS port (Covidien, Norwalk, CT, USA) with a standard 5- or 10-mm trocar. Adequate fog evacuation was achieved by replacing one of the trocars of the SILS port with a standard 5-mm trocar. Although clashing of the instruments is inevitable during certain stages of dissection, this difficulty was minimized by using one articulated grasper and one vessel-sealing device for the dissection and then changing the articulation angle of the grasper.
In the present study, no differences in mean operating time or blood loss were observed between the two groups. The duration of hospitalization was significantly longer in group 1 than in group 2. The mean tumor size was significantly larger in the conventional laparoscopy group. This was because patients with smaller tumors were preferentially selected for the SILA procedure during the early period of experience with this procedure in our institution.
In conclusion, the findings of the present study suggest that SILA is as safe as conventional transabdominal laparoscopic adrenalectomy for the treatment of benign adrenal lesions when performed by an experienced surgeon. Furthermore, SILA is associated with less pain and better cosmesis than the conventional laparoscopic procedure. Further studies are warranted to evaluate the specific advantages of this technique.
References
Fuente SG, DeMaria EJ, Reynolds JD, Poertenier DD, Pryor AD (2007) New development in surgery: natural orifice transluminal endoscopic surgery (NOTES). Arch Surg 142:295–297
Nguyen NT, Reavis KM, Hinojosa MW et al (2009) A single-port technique for laparoscopic extended stapled appendectomy. Surg Innov 16:78–81
Desai MM, Stein R, Rao P, Canes D, Aron M, Rao PP, Haber GP, Fergany A, Kaouk J, Gill IS (2009) Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for advanced reconstruction: initial experience. Urology 73(1):182–187
Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, Kaouk JH, Gill IS (2008) Transumbilical single-port surgery: evolution and current status. Eur Urol 54(5):1020–1029
Brunner W, Schirnhofer J, Waldstein-Wartenberg N, Frass R, Weiss H (2010) Single incision laparoscopic sigmoid colon resection without visible scar: a novel technique. Colorectal Dis 12(1):66–70
Desai MM, Rao PP, Aron M et al (2008) Scarless single-port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int 101:83–88
Rane A, Ahmed S, Kommu SS et al (2009) Single-port ‘scarless’ laparoscopic nephrectomies: the United Kingdom experience. BJU Int 104(2):230–233
Rane A, Rao P, Bonadio F, Rao P (2007) Single port laparoscopic nephrectomy using a novel laparoscopic port (R-port) and evolution of single laparoscopic port procedure (SLIPP). J Endourol 21:A287
Piskun G, Rajpal S (1999) Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 9(4):361–364
Remzi FH, Kirat HT, Kaouk JH, Geisler DP (2008) Single-port laparoscopy in colorectal surgery. Colorectal Dis 10(8):823–826
Barbaros U, Dinccag A (2009) Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg 13:1520–1523
Reavis KM, Hinojosa MW, Smith BR, Nguyen NT (2008) Single laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg 18(11):1492–1494
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327:1003
Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, Harmon JD (2008) Single port access adrenalectomy. J Endourol 22:1573–1576
Cindolo L, Gidaro S, Tamburro FR, Schips L (2010) Laparo-endoscopic single-site left transperitoneal adrenalectomy. Eur Urol 57(5):911–914
Jeong BC, Park YH, Han DH, Kim HH (2009) Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol 23(12):1957–1960
Cindolo L, Gidaro S, Neri F, Tamburro FR, Schips L (2010) Assessing feasibility and safety of laparoendoscopic single-site surgery adrenalectomy: initial experience. J Endourol 24(6):977–980
Disclosure
Dr. Fatih Tunca, Dr. Yasemin Giles Senyurek, Dr. Tarik Terzioglu, Dr. Yalın Iscan, and Dr. Serdar Tezelman have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tunca, F., Senyurek, Y.G., Terzioglu, T. et al. Single-incision laparoscopic adrenalectomy. Surg Endosc 26, 36–40 (2012). https://doi.org/10.1007/s00464-011-1824-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1824-9