Abstract
Background
Laparoendoscopic single-site (LESS) surgery is an emerging laparoscopic procedure previously used for cholecystectomy and appendectomy. However, few studies have examined LESS liver resection, and its benefits require investigation. This study aimed to evaluate the feasibility and safety of LESS liver resection.
Methods
From December 2009 to October 2010, 12 patients were selected for LESS liver resection with institutional review board approval. The LESS technique was performed using a transumbilical TriPort or three 5-mm trocars with a 5-mm linear or flexible laparoscope. Conventional or articulating laparoscopic instruments were used to mobilize and transect the lesions.
Results
The LESS liver resection procedure was successfully completed for 10 patients (83.3%), with the remaining 2 patients (16.7%) undergoing conversion to conventional multiport laparoscopy. The procedures consisted of left lateral segment resection (n = 4) and partial resection (n = 8) in addition to concomitant cholecystectomy (n = 3). The mean operative time was 80.4 min (range, 35–160 min), and the mean estimated blood loss was 45 ml (range, 20–800 min). No postoperative complications were noted except for biliary leakage (200 ml/day)in one patient. The mean hospital stay was 4.3 days (range, 2–8 days). No patient required postoperative analgesia, and the pain visual analog score 48 h after surgery was 0.53 (range, 0–2). Pathology identified 10 benign and 2 malignant liver tumors with a clear margin.
Conclusions
Our preliminary data show that LESS liver resection is safe and feasible for selected patients, with potential benefits that include a fast recovery, light pain, and cosmetically acceptable scarring. However, this procedure requires advanced instruments and complicated laparoscopic techniques, with a risk of intraoperative bleeding and postoperative bile leakage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopy is a widely recognized and increasingly used minimally invasive approach that has been extensively applied in general surgery, urology, gynecology, and endocrine surgery. Laparoscopy benefits from minimal invasiveness, rapid recovery, and cosmetically improved incisions, which derive mainly from the minimization of trauma by this surgical approach.
Currently, most laparoscopic procedures use three to six trocars. The use of fewer trocars is expected to benefit patients because reduced invasiveness results in lower pain levels, a faster recovery, and more favorable cosmetic incisions and likely reduces the underlying procedural risks caused by multiple punctures.
Natural orifice transluminal endoscopic surgery (NOTES) is a newly emerging advanced minimally invasive approach that requires no abdominal incision [1]. However, due to technical and technological limitations, NOTES still is largely limited to the laboratory and preclinical areas. To date, the use of NOTES for hollow organ dissection, additional abdominal trocars, and inconvenient endoscopic manipulation remains debatable [1, 2].
Laparoendoscopic single-site (LESS) surgery, also called single-incision laparoscopy, single-port laparoscopy, and single-site laparoscopy, is another emerging and highly advanced procedure that is minimally invasive. With LESS surgery, all laparoscopic working ports for entrance to the abdominal wall must be through a single site. This principle is its main advantage. Laparoscopic surgeons find it easier to adopt LESS than to adopt NOTES because LESS surgery is more similar to conventional laparoscopy. Therefore, LESS surgery is quickly developing due to accumulated experience and improved instrumentation. Increasingly, LESS surgery for appendectomy [3, 4], cholecystectomy [5], oophorectomy [6, 7], adrenalectomy [8], and gastric band placement [9] is being reported.
The actual benefits of LESS surgery remain unclear. However, some studies [2–9] suggest that LESS results in less pain, a more acceptable incision, and greater patient satisfaction. Hodgett et al. [4] compared LESS with conventional laparoscopy for cholecystectomy, showing a comparable operative time, complication rate, and length of hospital stay between the two procedures. However, patients who underwent LESS had greater satisfaction with the procedure due to a reduction in operative pain and a favorable incision. In addition, LESS nephrectomy resulted in less blood loss and a smaller cosmetic incision than conventional laparoscopic nephrectomy [2].
However, the use of LESS surgery for complex laparoscopic procedures has been reported only for individual cases or small series [10–14]. Recently, two case reports of LESS liver resection (n = 1 each) [15, 16] and another serial report (n = 5) [17] were published. Therefore, larger-scale studies are required to confirm the feasibility of LESS liver resection.
In this study, we performed LESS liver resection in a prospective single-arm study to establish its safety and feasibility. In addition, we aimed to identify challenges and suggest solutions for LESS liver resection procedures.
Materials and methods
Patients
From December 2009 to October 2010, 12 patients with a diagnosis of liver tumors underwent selective LESS liver resection at the Chinese PLA General Hospital, Aerospace Central Hospital, and First Affiliated Hospital of Chinese PLA General Hospital. All the patients participating in this study gave informed consent before surgery. The inclusion criteria specified patients undergoing elective resection of malignant tumor smaller than 2.5 cm in diameter located in segments 3, 4b, and 5; patients with benign tumors smaller than 10 cm in diameter located in segments 2–5; and patients shorter than 180 cm who were not morbidly obese and had no history of upper abdominal surgery. The candidate patients for left lateral segment resection (LLSR) were excluded if a larger transaction section between segments 2, 3, and 4 was expected to be required.
Surgical procedures
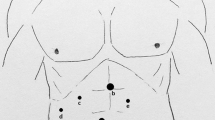
Patients were placed in the lithotomy (“French”) position under intravenous general anesthesia with either a laryngeal mask airway (n = 3) or endotracheal intubation (n = 9). A TriPort (Advanced Surgical Concepts, Wicklow, Ireland) was placed at the umbilicus in seven patients to establish the abdominal access port (Fig. 1A). Three adjacent 5-mm trocars were used in the remaining five patients, for whom three 5-mm incisions were made below the umbilicus at an interval of 5 to 10 mm and in an inverted triangle (Fig. 1B). Then, 5-mm 30° linear laparoscopes were used in 10 patients. In the remaining two patients, a 0° laparoscope and another 30° laparoscope with a flexible end (Olympus America, Center Valley, PA, USA) were used.
In addition to conventional laparoscopic instruments, this study used articulating instruments (Cambridge Endo, Framingham, MA, USA), linear staplers, a ultrasonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH, USA), a bipolar electrocauterizer, bioabsorbable vascular clamps, and an argon beam coagulator.
The laparoscope was inserted through the median access port or trocar according to routine procedure and adjusted to the other two working ports or trocars as necessary. Laparoscopic manipulation was performed by a one-handed or cross-handed maneuver under a distant vision. To minimize instrument collisions, the retrieval instrument was placed first, followed by manipulative instruments. An articulated linear stapler was used to fracture liver tissues through an ideal angle.
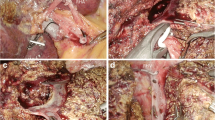
For patients undergoing LLSR, the round ligament, falciform ligament, left coronary ligament, and left triangular ligament were transected in an orderly manner using a ultrasonic scalpel to mobilize the left lateral lobe. A 5-mm grasper was inserted through the right port or trocar to retract the lobe to the left side while the arch of the retractor was placed toward the right. The liver was transected along the falciform ligament. The vascular pedicles of segments 2 and 3 were bluntly dissected and ligated with a linear stapler (Fig. 2A). Subsequently, the left hepatic vein was bluntly dissected and ligated with another linear stapler.
Laparoendoscopic single-site liver resection procedure. A Ligating vascular pedicles of segments 2 and 3 using a linear stapler (patient 1). B Transecting a hepatocellular carcinoma located at segments 4 and 5 (patient 5). C Removing a lesion of focal nodular hyperplasia at segment 4b in a left–right-down order (patient 7)
After the left lateral lobe had been completely removed, a bipolar electrocauterizer or argon beam coagulator was used for hemostasis of the liver wound. Additionally, for partial resection, the surrounding liver parenchyma was transected in a left–right-down order through the proposed division line using a ultrasonic scalpel (Fig. 2B, C). For patient 6, two linear staplers were used to resection the tumor locally rather than ultrasonic scalpel. For patients with gallbladder disorders, cholecystectomy was performed concomitantly.
For the patients who had use of the TriPort, the laparoscope and grasper were inserted through two 5-mm ports, and a retrieval bag was placed through the 10-mm port. The specimen was wrapped in the retrieval bag and extracted from the umbilical incision. After removal of the TriPort, the specimen was broken up and removed as small pieces. If drainage was required (n = 2), a 10-mm trocar and a 5-mm trocar were introduced into the peritoneal cavity, and the fascial defect was closed around the trocars. An additional 5-mm dissector was inserted through a separate fascial incision rather than through a trocar. The drain was delivered though the 10-mm trocar.
After completion of the drainage placement, the 10-mm trocar, dissector, laparoscope, and 5-mm trocar were withdrawn sequentially. When three adjacent 5-mm trocars were used, two adjacent incisions were merged to accommodate a 10-mm trocar. The retrieval bag and laparoscope were introduced through the remaining 5-mm trocar. An additional 5-mm dissector was inserted directly through a separate fascial incision without the need for a trocar. The specimen was extracted as a whole (for malignant tumors) or in small pieces (for benign tumors). No drain was placed in patients undergoing the three-trocar procedure (n = 5). Umbilical incisions were closed using subcutaneous sutures and not extended for specimen extraction (Fig. 3).
Results
The study enrolled 12 patients (7 men and 5 women) with a mean age of 41.3 ± 11.3 years (range, 25–64 years), a mean height of 170.8 ± 6.1 cm (range, 160–178 cm), and a body mass index of 26.3 ± 2.7 kg/m2 (range, 21.8–30.4 kg/m2). The liver function of all the patients rated as Child-Pugh class A.
Benign tumors were preoperatively diagnosed in 10 patients, whereas malignant tumors were diagnosed in two patients. All lesions were located in segments 2–5 and had a mean size of 4.4 ± 2.6 cm (range, 1.1–9.6 cm). Additionally, three patients had concomitant gallbladder disorders (Table 1).
For 10 patients (83.3%), LESS liver resection was successfully completed, and the remaining 2 patients (16.7%) underwent conversion to conventional laparoscopy. Conventional techniques were adopted either due to compromised laparoscopic manipulation (n = 1) or because the restricted-vision 0° laparoscope was unable to ensure operative safety (n = 1).
The procedures consisted of LLSR (n = 4), partial hepatectomy (n = 8), and concomitant laparoscopic cholecystectomy (n = 3). The mean operative time was 80.4 ± 38.3 min (range, 35–160 min), and the mean blood loss was 45 ml (range, 20–800 ml). Massive hemorrhage (800 ml) during the operation occurred for one patient. A postoperative complication occurred for one patient, who experienced a daily 200-ml bile leakage that resolved with prolonged drainage.
Notably, no narcotic analgesia was given to patients after surgery because up to 48 h after surgery, the mean pain visual analog scale still was 0.53 ± 0.80 (range, 0–2). The postoperative hospital stay was 4.3 ± 1.6 days (range, 2–8 days). Pathology performed for preoperative evaluation identified hepatocellular carcinoma (n = 2) with a clear margin, hemangioma (n = 6) with one patient having a multifocal lesion, focal nodular hyperplasia (n = 3), and hepatoadenoma (n = 1). The incision length was less than 2.5 cm. During a mean 5.2-month follow-up period, no tumor recurrence or short- or long-term wound-site complications were identified (Table 2).
Discussion
Since the 1990s, laparoscopic liver resection has become a popular and widely accepted procedure [18–22]. Multiple controlled studies have shown its procedural benefits and comparable effectiveness [20, 21]. The most frequently performed and accepted procedures for laparoscopic liver resection are laparoscopic LLSR and partial resection due to their effectiveness and safety [18–22].
Recently, LESS surgery has been shown to have additional benefits of reduced pain, a more cosmetic incision, and a rapid recovery [2–14]. However, few studies have investigated LESS liver resection [15–17], which implies that the safety and feasibility of LESS liver resection requires evaluation.
Single-port access LLSR recently has been performed on the liver of a patient with metastatic colon cancer. An additional trocar was required to assist manipulation, with subsequent extension (3.5 cm) for removal of the specimen [15]. Similarly, LLSR has been performed successfully through a single port without an additional trocar or an extended incision (8 cm) [16].
In addition, an initial five-case series of LESS liver resection has been reported. The patients were managed using GelPort due to the absence of a supplemental port [17]. In all five cases, liver resection was performed successfully without any intra- or postoperative complications and with a reduction in blood loss and operative time. However, a 50-mm incision compromised the cosmetic outcome. Such a large incision is in stark contrast with the incision size required for LESS. Moreover, it is not known whether LESS surgery is suitable for patients with a history of abdominal surgery.
The LESS approach is not without its drawbacks. It results in crowded instruments, problems with in-line viewing, loss of triangulation, and a limited range of motion, especially during complex procedures [18–22]. Overcoming these drawbacks is essential for LESS surgery to become feasible. The technical difficulties of LESS liver resection lie in a requirement of massive liver dissection, frequent alternation and adjustment of instruments, compromised wound hemostasis, a shifted division line, restriction by the length of the laparoscopic instrument (especially the linear stapler), and an inappropriate placement of the drain.
In our study, partial resection, a simpler procedure, was successfully completed without complications for seven (87.5%) of eight patients within a short period of 60.0 ± 23.6 min. However, we observed that LLSR required more complicated manipulations than partial resection, which resulted in a longer operative time in cases 1 to 4 (mean, 121.3 ± 26.6 min). Massive intraoperative bleeding complicated with bile leakage occurred for patient 2 after the first stapling. Such an intraoperative event failed to be appropriately resolved using LESS, indicating that it causes postoperative bile leakage (Fig. 4).
For patient 4, LESS was converted to conventional laparoscopic surgery due to an inconvenient manipulation with the 0° laparoscope. The remaining two cases of LLSR did not have additional complications, although the frequent alternation and adjustment of instruments was both laborious and time consuming. The placement of drainage using the single-access site gave rise to a similar inconvenience, especially when the TriPort was used. Our results indicate that some underlying technical obstacles still need to be solved.
To overcome the obstacles encountered in LESS liver resection, we adopted the following methods based on previous experience with LESS cholecystectomy and fenestration of liver and spleen cysts. Only small tumors (<3 cm) located in proximity to the liver surface of segments 2–4 were indicated for partial resection. For LLSR, the transection surface between segments 2/3 and 4b was minimized. Furthermore, massive liver dissection and transection were avoided. The TriPort also was used to facilitate further manipulation, which reduced collisions due to crowded instruments.
In addition, 30° rather than 0° laparoscopy is recommended because a flexible-tip laparoscope can produce a better visual field than that advocated for simple procedures [3]. However, these laparoscopes are delicate and subject to mechanical damages in the process of complex movements in a tight space. Additionally, some specialized instruments such as low-profile trocars, articulating instruments, short-handled instruments of various lengths, and coaxial light-tipped laparoscopes could also improve operative ergonomics [23]. Suspension of ligaments also should be used as intrinsic retractors to allow a smooth sequential dissection.
Liver dissection should focus on manipulation that minimizes damage to the patient. We also recommend that the patient not be taller than 180 cm or morbidly obese because in such cases conventional laparoscopic instruments, such as the linear stapler, are of an insufficient length to reach the posterior space of the liver when inserted from the umbilical site.
Patience plays a critical role in the success of LESS liver resection. In addition, LESS procedures reportedly have been improved by magnetic navigation laparoscopes [5], magnetic retractors [24–26], a laparoscopic adjustable suture and retractor [4], prebent laparoscopic instruments [23], and a 2-mm needlescopic trocar and micro instruments [26–28]. We propose that 2-mm needlescopic instruments would improve LESS liver resection. These instruments can be inserted into the peritoneal cavity without any skin incision, and they facilitate liver retraction, ensuring procedural safety. Robot-assisted LESS is reported to be a promising method, but further investigation is required to confirm its applicability [7, 29].
The variety of trocar placements available might extend the applicability of LESS. In 1 of 12 patients (patient 8), LESS surgery was converted to conventional laparoscopy because manipulation of the tumor was compromised due to its proximity to the diaphragmatic dome. We suggest that a right superior quadrant surgical site might avoid this complication. The use of the left superior quadrant trocar has been reported for LESS splenectomy [30].
Our results confirmed the safety of LESS liver resection, which had minimal complications resulting in adverse events. The patients had a fast recovery. The gastric tube was removed from eight patients immediately after surgery without any subsequent discomfort. Five patients (41.7%) started oral intake 6 h after surgery, and the patients resumed oral intake at a mean of 0.83 days. The mean hospital stay was only 4.3 days, which was extremely short for liver resection. Skin incisions had an improved cosmetic effect (Fig. 3) because they were smaller than 2.5 cm and could easily be disguised by umbilical skin folds. Mental stress was reduced due to the cosmetic nature of the incision and pain reduction.
We suggest that LESS liver resection can produce the same surgical outcome as conventional laparoscopic liver resection. Its only disadvantages in this study were the longer operative time and the slightly greater risk of procedural complications.
The applicability of LESS surgery is disputed in the literature [2, 13, 31–33]. Whether the well-recognized cosmetic outcome and reduced pain with LESS outweighs its poorer cost effectiveness, intricate maneuvers, prolonged duration, and increased procedural risk requires confirmation through randomized controlled trials.
Laparoscopic radiofrequency ablation is another excellent option for malignant tumors smaller than 3 cm because it results in a favorable and comparably long-term patient survival compared with surgical resection [34, 35]. An overlap in the functionality of LESS and laparoscopic radiofrequency might exist. However, LESS surgery still is the preferred option for lesions in proximity to the gallbladder, for hepatic hilar, and for histologic biopsies. In case of malignant tumors, the principle of en bloc resection still applies to prevent iatrogenic dissemination and metastasis.
Extension of the trocar incision still can compromise the advantages of LESS surgery [2, 8]. Therefore, LESS is relatively contraindicated for malignant tumors larger than 3 cm in diameter [16]. The shortest incision needs to be clearly defined for LESS procedures.
In conclusion, for selected patients, LESS liver resection is feasible and safe. Compared with multiport laparoscopy, LESS has a faster recovery, less pain, and more cosmetically acceptable scarring. However, this procedure requires advanced laparoscopic techniques and instruments, which increases the risks of intraoperative bleeding and postoperative bile leakage. These risks should be reduced through improvements in instrumentation and technological innovation, which have the potential to improve the applicability of LESS liver resection.
References
Sodergren MH, Clark J, Athanasiou T, Teare J, Yang GZ, Darzi A (2009) Natural orifice translumenal endoscopic surgery: critical appraisal of applications in clinical practice. Surg Endosc 23:680–687
Raman JD, Bagrodia A, Cadeddu JA (2009) Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol 55:1198–1204
Binenbaum SJ, Teixeira JA, Forrester GJ, Harvey EJ, Afthinos J, Kim GJ, Koshy N, McGinty J, Belsley SJ, Todd GJ (2009) Single-incision laparoscopic cholecystectomy using a flexible endoscope. Arch Surg 144:734–738
Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, Oh SJ, Park SM (2009) Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A 19:75–78
Fagotti A, Fanfani F, Marocco F, Rossitto C, Gallotta V, Scambia G (2009) Laparoendoscopic single-site surgery (LESS) for ovarian cyst enucleation: report of first 3 cases. Fertil Steril 92(1168):e13–e16
Fader AN, Escobar PF (2009) Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol 114:157–161
Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, Desai MR, Rao PP, Sotelo R, Stein R, Gill IS (2009) Laparoendoscopic single-site surgery: initial hundred patients. Urology 74:805–812
Teixeira J, McGill K, Binenbaum S, Forrester G (2009) Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc 23:1409–1414
Barbaros U, Dinccag A (2009) Single-incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg 13:1520–1523
Bucher P, Pugin F, Morel P (2008) Single-port access laparoscopic right hemicolectomy. Int J Colorectal Dis 23:1013–1016
Leroy J, Cahill RA, Asakuma M, Dallemagne B, Marescaux J (2009) Single-access laparoscopic sigmoidectomy as definitive surgical management of prior diverticulitis in a human patient. Arch Surg 144:173–179; discussion 179
Kaouk JH, Goel RK (2009) Single-port laparoscopic and robotic partial nephrectomy. Eur Urol 55:1163–1169
Mantke R, Wicht S (2010) Single-port liver cyst fenestration combined with single-port laparoscopic cholecystectomy using completely reusable instruments. Surg Laparosc Endosc Percutan Tech 20:e28–e30
Patel AG, Belgaumkar AP, James J, Singh UP, Carswell KA, Murgatroyd B (2011) Single-incision laparoscopic left lateral sectionectomy of colorectal liver metastasis. Surg Endosc 25:649–650
Aldrighetti L, Guzzetti E, Ferla G (2011) Laparoscopic hepatic left lateral sectionectomy using the laparoendoscopic single site approach: evolution of minimally invasive liver surgery. J Hepatobiliary Pancreat Sci 18:103–105
Gaujoux S, Kingham TP, Jarnagin WR, D’Angelica MI, Allen PJ, Fong Y (2011) Single-incision laparoscopic liver resection. Surg Endosc 25:1489–1494
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:385–389
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS, World Consensus Conference on Laparoscopic Surgery (2009) The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 250:825–830
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection: 2,804 patients. Ann Surg 250:831–841
Abu Hilal M, McPhail MJ, Zeidan B, Zeidan S, Hallam MJ, Armstrong T, Primrose JN, Pearce NW (2008) Laparoscopic versus open left lateral hepatic sectionectomy: a comparative study. Eur J Surg Oncol 34:1285–1288
Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, Brock G, McMasters KM (2008) Experience with more than 500 minimally invasive hepatic procedures. Ann Surg 248:475–486
Romanelli JR, Earle DB (2009) Single-port laparoscopic surgery: an overview. Surg Endosc 23:1419–1427
Langwieler TE, Nimme T, Back M (2009) Single-port access in laparoscopic cholecystectomy. Surg Endosc 23:1138–1141
Raman JD, Scott DJ, Cadeddu JA (2009) Role of magnetic anchors during laparoendoscopic single-site surgery and NOTES. J Endourol 23:781–786
Dominguez G, Durand L, De-Rosa J, Danguise E, Arozamena C, Ferraina PA (2009) Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg Endosc 23:1660–1666
Desai MM, Stein R, Rao P, Canes D, Aron M, Rao PP, Haber GP, Fergany A, Kaouk J, Gill IS (2009) Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for advanced reconstruction: initial experience. Urology 73:182–187
Aron M, Canes D, Desai MM, Haber GP, Kaouk JH, Gill IS (2009) Transumbilical single-port laparoscopic partial nephrectomy. BJU Int 103:516–521
Kaouk JH, Goel RK, Haber GP, Crouzet S, Stein RJ (2009) Robotic single-port transumbilical surgery in humans: initial report. BJU Int 103:366–369
Targarona EM, Pallares JL, Balague C, Luppi CR, Marinello F, Hernández P, Martínez C, Trias M (2010) Single-incision approach for splenic diseases: a preliminary report on a series of 8 cases. Surg Endosc 24:2236–2240
Rane A, Ahmed S, Kommu SS, Anderson CJ, Rimington PD (2009) Single-port “scarless” laparoscopic nephrectomies: the United Kingdom experience. BJU Int 104:230–233
Connor S (2009) Single-port-access cholecystectomy: history should not be allowed to repeat. World J Surg 33:1020–1021
Prasad A (2010) Single-incision laparoscopic surgery. World J Gastroenterol 16:2705–2706
Vanagas T, Gulbinas A, Pundzius J, Barauskas G (2010) Radiofrequency ablation of liver tumors (II): clinical application and outcomes. Medicina Kaunas 46:81–88
Asahina Y, Nakanishi H, Izumi N (2009) Laparoscopic radiofrequency ablation for hepatocellular carcinoma. Dig Endosc 21:67–72
Acknowledgments
We thank Medjaden Bioscience Limited and Professor Duo Li from Aerospace Central Hospital for their valuable language assistance in the preparation of the manuscript.This work was not supported by any outside research funding.
Disclosures
Guodong Zhao, Minggen Hu, Rong Liu, Dabin Xu, Caiguo Ouyang, Yong Xu, Huabo Jiao, Baofu Wang, Xin Gu have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guodong Zhao and Minggen Hu contributed equally to this study.
Rights and permissions
About this article
Cite this article
Zhao, G., Hu, M., Liu, R. et al. Laparoendoscopic single-site liver resection: a preliminary report of 12 cases. Surg Endosc 25, 3286–3293 (2011). https://doi.org/10.1007/s00464-011-1706-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1706-1