Abstract
Background
The preemptive intravenous and intraperitoneal application of local anesthetics is known to improve the postoperative outcome in abdominal surgery. The aim of this study was to compare the analgesic effect of intravenous lidocaine injection to that of intraperitoneal lidocaine instillation in patients who were undergoing laparoscopic appendectomy (LA).
Method
Sixty-eight patients who were undergoing LA for unperforated appendicitis were randomly divided into three groups. Group IP (the intraperitoneal instillation group) received intraperitoneal instillation of lidocaine and intravenous normal saline injection. Group IV (the intravenous injection group) received intravenous lidocaine injection and intraperitoneal instillation of normal saline. In group C (the placebo control group), normal saline was given both intravenously and intraperitoneally. The visual analog scale (VAS) of pain scores was measured after surgery. The needs for additional intravenous fentanyl were evaluated and the integrated fentanyl consumption (PCA delivered + additional fentanyl) was assessed. The incidence of shoulder tip pain and postoperative nausea and vomiting (PONV) were noted.
Results
Reduction of the VAS score and of fentanyl consumption was noted in the IV and IP groups and compared to that of group C (P < 0.05). The shoulder tip pain and PONV were reduced in groups IP and IV compared to that in group C (P < 0.05). However, no significant differences were found between the IP and IV groups for all the studied variables. There was no adverse effect from intravenous lidocaine throughout the study.
Conclusion
Intravenous lidocaine injection is as effective as intraperitoneal instillation for reducing pain and fentanyl consumption. The major benefit of intravenous injection is that this is an easily and universally applicable procedure compared to that of intraperitoneal instillation. Lidocaine intravenous administration is a better alternative for reducing the pain of patients who are undergoing laparoscopic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic surgery has had improved outcomes compared to those of conventional open procedures in terms of quicker recovery, less postoperative pain, better cosmesis, and, in some cases, less morbidity [1–3]. Despite the brief recovery time and the generally good result compared to the open technique, the effect of peritoneal irritation by the desiccated gas used for pneumoperitoneum is underestimated and this leads to aggravated peritoneal and referred postoperative pain [2, 4–6]. Various methods of pain control have been attempted because better pain control could enhance the advantages of laparoscopic techniques and facilitate earlier discharge and better patient satisfaction.
Preemptive analgesia (i.e., the administration of drugs that modulate the development of the nociceptive process before the pain stimuli appear) is used to control postoperative pain and minimize opioid consumption and the development of subsequent complications. Tissue and peripheral nerve injury leads to a local inflammatory reaction accompanied by increased levels of proinflammatory cytokines, which induce peripheral and central nervous system sensitization that leads to hyperalgesia [7]. Many clinical studies have demonstrated the inhibitory effect of preemptive analgesia on the development of post-traumatic hyperalgesia, and this results in the reduction of postoperative pain and the total analgesic requirement [8, 9]. It is known that intraperitoneal instillation of local anesthetics before laparoscopic procedures reduces postoperative pain, analgesic requirement, and stress response, and it lengthens the period to the first postoperative analgesic requirement [9–11]. However, spraying lidocaine during a laparoscopic procedure to reduce postoperative pain can be an addition to the workload of a surgeon, especially when the operation is a complicated one.
An alternative approach to reduce postoperative pain and thus accelerate recovery after an operation is intravenous lidocaine. Intravenous lidocaine has analgesic, anti-inflammatory, and antihyperalgesic properties that have been reported to reduce postoperative pain [12–15]. The drug’s benefits are enhanced by its low cost and easy accessibility and safety [16]. The aim of this study was to compare the analgesic effect of intravenous lidocaine infusion with that of intraperitoneal lidocaine instillation.
Materials and methods
Patients
The study protocol was approved by the local ethics committee and the study was registered in the Australian New Zealand Clinical Trial Records (ACTRN12610000649011). This study was carried out according to the principle of the Declaration of Helsinki 2000, and written informed consent was obtained from all the participants before inclusion in the trial.
A total of 83 consecutive patients (age range = 18–65) who underwent laparoscopic appendectomy (LA) for unperforated appendicitis at Chung-Ang University Hospital, Seoul, Korea, between March 2009 and December 2009 were considered eligible for the study. The exclusion criteria were a body weight below 45 kg or greater than 100 kg, a history of severe underlying cardiovascular, pulmonary, renal, or hepatic disease, and an allergic reaction to local anesthetics. The decision to enroll or exclude a patient was made by the investigator, who did not otherwise participate in conducting the study or collecting data.
Study design and randomization
This is a randomized, double-blinded, placebo-controlled study. Randomization into one of the three groups was based on Excel (Microsoft Corp., Redmond, WA) random-number generation. The details of the series, which were generated by a statistician who did not otherwise participate in this study, were unknown to the investigators and the patients, and the numbers were contained in a set of sealed envelopes. After admitting the patient into the operating room and just before the induction of anesthesia, the numbered envelope was opened and the card inside determined into which group the patient would be placed. In order to keep the surgeon and the anesthesiologist “blind” to the patient’s group, the patients were given lidocaine or normal saline as placebo, unlabeled, by an investigator who read the card. The anesthesiologists were given 0.55 ml/kg of 1% lidocaine or normal saline of the same volume for intravenous injection. The surgeons were given 1.75 ml/kg of 0.2% lidocaine (3.5 mg/kg) or the same volume of normal saline for intraperitoneal instillation.
The patients were divided into three groups according to the intravenous and intraperitoneal solutions given. The patients assigned to group IP (the intraperitoneal instillation group) received intraperitoneal instillation of 3.5 mg/kg lidocaine at the initiation of the pneumoperitoneum and intravenous normal saline injection. Those in group IV (the intravenous injection group) were given an intravenous bolus injection of 1.5 mg/kg lidocaine followed by a continuous infusion of 2 mg/kg/h and normal saline intraperitoneal instillation. For the patients who were assigned to group C (the placebo control group), intravenous normal saline was given and intraperitoneal instillation of normal saline was applied.
Two investigators who were blinded to the details of the study collected the postoperative data. Oral intake of solid food was started as soon as the patients could tolerate it and when bowel function became adequate. Patients were discharged as soon as they were adequately ingesting food orally and they were mobile.
General anesthesia
All the patients were transferred to the operating room without premedication. Anesthesia was induced with intravenous thiopental (5 mg/kg) and rocuronium (0.6 mg/kg). The trachea was intubated and ventilation was adjusted to keep the end tidal CO2 between 35 and 40 mmHg. Anesthesia was maintained using 2–3% sevoflurane and 50% nitrous oxide in oxygen. Noninvasive arterial blood pressure, electrocardiography, and pulse oximetry were monitored continuously. Lactated Ringer’s solution (3–6 ml/kg/h) was infused throughout surgery. No additional intravenous opioids were injected.
Surgical technique
All the operations were carried out by the same surgical team. The patient was placed in a slight Trendelenburg position. The insufflation pressure was automatically regulated and maintained at 12–15 mmHg. LA was performed using a two-handed, three-trocar technique. A 10-mm subumbilical port was introduced for the 5-mm-diameter telescope. Subsequently, 5-mm ports were placed in the suprapubic region and in the right upper quadrant. The telescope was then shifted to the 5-mm port in the right upper quadrant. The mesoappendix was dissected using a dissector and it was ligated using a hemoclip. The appendix was ligated twice with a 3-0 Vicryl loop at its base and then it was divided. To avoid contamination, the appendix was removed in a laparoscopic retrieval bag. The appendectomy site was washed at the end of surgery with a small volume of saline (100–200 ml) to evacuate any hematoma and other debris.
Intraperitoneal and intravenous solutions
Intraperitoneal instillation of lidocaine solution (total instillation dose: 3.5 mg/kg) or placebo solution was administered as follows. Immediately after the creation of the pneumoperitoneum and 10 min before beginning surgery, the surgeon sprayed one quarter of the total solution on the upper surface of the liver under the right subdiaphragmatic space and another one quarter of the total solution under the left subdiaphragmatic space. In order to allow the sprayed solution to diffuse under the diaphragmatic space, the Trendelenburg position was maintained for about 2 min. After the Trendelenburg position was withdrawn, an additional half of the total solution was sprayed around the appendectomy site. This was performed using the catheters inserted into the subumbilical area and the right upper quadrant trocars under direct laparoscopic control.
The patients in group IV received an intravenous bolus injection of lidocaine (1.5 mg/kg) 2 min before orotracheal intubation, followed by continuous intravenous infusion at 2 mg/kg/h during the operation. The patients in groups C and IP received the same amount of intravenous normal saline as placebo.
Postoperative pain control
To control postoperative pain, intravenous fentanyl with a computerized intravenous patient-controlled analgesia (PCA) system (Automed 3300TM, ACE Medical Corp. Ltd., Seoul, Republic of Korea) was used. The mode of PCA was a bolus of 0.1 μg/kg, a lockout interval of 15 min, and a continuous infusion of 0.1 μg/kg/h (total regimen: 10 μg/kg/100 ml). The patients were taught to push the button of the PCA system to get a bolus of drug each time pain occurred. In the case of persistent pain greater than a visual analog scale (VAS) pain score of 30 mm, an additional 50 μg of fentanyl was injected intravenously by the investigator until the pain was relieved to a level below a VAS pain score of 30 mm. No other analgesics such as NSAIDs or acetaminophens were included.
The studied variables
For each patient, the age, gender, the American Society of Anesthesiologists (ASA) physical status, the duration of anesthesia (from injection of thiopental to extubation), and the duration of the operation (from skin incision to closure) were recorded. The primary outcome measure of the study was the VAS pain score (0–100 mm), which was measured by an investigator who was blind to the study. The VAS was measured at 2, 4, 8, 12, 24, and 48 h after surgery. Additional analyses were performed with regard to fentanyl consumption, the incidence of shoulder tip pain, and the frequency of postoperative nausea and vomiting (PONV).
The need for additional intravenous fentanyl was evaluated and the integrated fentanyl consumption (PCA delivered + additional fentanyl) was assessed at the same time intervals for each patient. The total amount of injected fentanyl for the postoperative period was compared between the groups.
In addition, time values that represented the recovery rate were collected from each patient; these included the time of first flatus, the time of first ingesting a regular diet, and the length of the hospital stay.
Statistical analysis
To estimate the group size, we conducted a pilot study to measure the VAS pain score at 2 h after surgery in ten patients who received normal saline intraperitoneally and intravenously. The standard deviation of the VAS pain score in this group was 21 mm. For our power calculation, we assumed an equal standard deviation in group IP and group IV. We wanted to be able to show a difference of 20 mm in the VAS pain score at 2 h after surgery among the groups. With α = 0.05, two-tailed, and a power of 80%, we needed 22 patients per group. Considering a compliance rate of 80%, we asked 83 patients to participate in this study.
For intergroup comparisons, the distribution of the data was first evaluated for normality using the Shapiro–Wilk test. The normally distributed data are presented here as the mean ± standard deviation, and groups were compared using analysis of variance and a post hoc Tukey test. The non-normally distributed data are expressed as medians (interquartile range) and it was analyzed using the Kruskal–Wallis test with Bonferroni’s correction. The lidocaine consumption between group IV and group IP was compared using Student’s t-test.
Descriptive variables were subjected to χ2 analysis or Fischer’s exact test, as appropriate, and P < 0.05 was considered statistically significant. Pearson’s correlation coefficient was used to measure the correlation between the VAS pain score and fentanyl consumption. The data in the figures is mean ± standard error. Statistical analysis was performed using SPSS 15.0 (SPSS Inc., Chicago, IL).
Results
There were no differences among the groups in terms of age, BMI, ASA class, duration of anesthesia, and the operation time (Table 1). There were no differences between groups IP and IV with respect to the amount of used lidocaine.
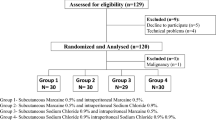
Of the 83 patients who were eligible for the study from March 2009 to December 2009, 6 patients refused to participate and 9 patients were excluded because they suffered from morbid obesity, cardiac, pulmonary, and/or hepatic disease, or were allergic to anesthetics. Of the 68 patients remaining, 21 were randomized to group C, 25 to group IP, and 22 to group IV (Fig. 1).
The results of the VAS pain scores are shown in Fig. 2. Despite the administration of rescue analgesic, the VAS pain score in group C was above 30 mm until 8 h. There was a significant reduction of pain scores between 2 and 12 h in group IP compared with that of group C (P < 0.05). The VAS was lower in group IV than that in group C until 8 h (P < 0.05). No significant differences were seen between groups IP and IV at all the time intervals. In all the groups, the pain gradually diminished during the time sequence.
In all the time periods, the fentanyl consumption was significantly higher in group C than that in groups IP and IV (Fig. 3). Fentanyl consumption was slightly lower in group IP than in group IV; however, there were no significant differences between the two groups. The amount of fentanyl consumption was significantly less in groups IP and IV than in group C, and significantly less in group IP than that in group IV (Fig. 4).
Shoulder tip pain was reduced a great degree in groups IP and IV compared to that of group C (P < 0.05). No significant difference of shoulder pain was found between groups IP and IV (Table 2). In general, the VAS pain score correlated well with fentanyl consumption (ρ = 0.323, P < 0.001).
Nausea was less frequent in groups IP and IV than that in group C, but this was not statistically significant (Table 2). The length of hospital stay, time to first flatus, and time to resuming a regular diet were slightly decreased in groups IV and IP, but there was no significant difference among all the groups.
Discussion
This study demonstrated that preemptive intraperitoneal lidocaine instillation and intravenous lidocaine injection significantly reduced postoperative pain and opioid consumption compared to control in LA patients. The VAS pain scores were lower in groups IP and IV than in group C during the overall estimated time. None of the patients was excluded from the study because of undesirable surgical outcomes or patient intolerance. To the best of our knowledge, this is the first study that has compared the postoperative pain outcomes of intraperitoneal instillation of lidocaine and intravenous injection of lidocaine in patients who underwent laparoscopic surgery.
The number of laparoscopic procedures performed has been rapidly increasing because of their reduced invasiveness and the reduced peritoneal injury and tissue trauma [2]. Notwithstanding the merit of minimal invasiveness, laparoscopic surgery is certainly not pain free. In a recent randomized controlled trial, laparoscopic procedures were reported to cause more intense pain during the immediate postoperative period [17]. Pain remains a major morbidity, which leads to increased consumption of analgesics, delayed bowel function, and subsequent complications. Furthermore, the requirement for rescue analgesics increases the need for costly medical attention and the length of the hospital stay, especially in patients who undergo LA, which is performed on a day-case basis or fast-track basis for which early postoperative pain relief is imperative. There have been few studies on LA, which may be explained by the fact that the pain after LA is less severe than that after other laparoscopic procedures and so this attracts less attention by investigators. However, it has been reported that procedures commonly considered routine, such as LA, were rated to be especially painful by the patients [18]. This study showed an elevated VAS score in group C above 30 mm until 8 h, which means there was significant postoperative pain even for LA.
Various attempts have been made to reduce the postoperative pain of laparoscopic surgery, including intraperitoneal instillation [19], preincisional infiltration [20], intraperitoneal nebulization [21], epidural administration, and continuous intravenous infusion of local anesthetics [16]. Many clinicians have demonstrated that intraperitoneal instillation of local anesthetic reduces postoperative pain and the need for analgesic medications [22–24]. A recent meta-analysis reported that preemptive intraperitoneal instillation of local anesthetic can be recommended, which is in line with the concept that the operative period is of particular importance for the pain sensitization process [25, 26]. However, it is always a burden to perform extra procedures and to maintain constant instillation under circumstances of panperitonitis, loculated peritoneal fluid collections, and whenever analogous environments are present in the operation field.
Intravenous administration of lidocaine is easy, safe, and inexpensive. The analgesic effect of systemic lidocaine is biphasic. It has a peripheral suppression effect on acute chemically induced pain [27, 28], and also a central antihyperalgesic effect [29, 30]. Its modes of action have been studied and it is assumed that systemic lidocaine mediates various actions, including sodium channel blockade [14], muscarinic receptor blockade [31], N-methyl-d-aspartate (NMDA) receptor blockade [32] and inhibition of polymorphonuclear leukocyte priming and activation [33].
The local macrophages control the increased levels of cytokines in injured tissue, and these cytokines magnify the pain and cause hyperalgesia. For treating this phenomenon, the administration of systemic lidocaine can simply reduce pain by its cytokine-modulating properties. Moreover, previous studies have shown that the conduction velocities in mechanosensitive and insensitive nociceptors, which are mediated by and involved in hyperalgesia, and the axon flare reaction are profoundly decreased under a lidocaine environment by way of the drug’s sodium channel suppression-supporting analgesic effect [34, 35]. Lidocaine also reduces NMDA and neurokinin receptor-mediated postsynaptic depolarization, which plays a major role in central analgesics [32, 36].
Perioperative continuous low-dose intravenous infusion of lidocaine (2–3 mg/min) has been studied by Groudine and Koppert [12, 13]. These previous studies emphasized its benefits such as an early return of bowel function and reduction of pain and opioid consumption. In those studies, the plasma lidocaine concentration was monitored and low-dose intravenous lidocaine injection did not approach the toxic level throughout the study, and there were no side effects. The safety of low-dose intravenous lidocaine was also shown in a meta-analysis that reported no toxicity in any trials [15]. Although there is no standard protocol in these earlier studies, the dosage and the duration of lidocaine injection differed mainly in the postoperative period. Its preoperative and intraoperative doses were similar in the previous studies because of the consensus that lidocaine, as an intervening analgesia in the preoperative and intraoperative periods, is significant. We also investigated the preoperative and intraoperative effects of lidocaine in this study.
Our results indicated that both intraperitoneal instillation of lidocaine and intravenous lidocaine injection provided clinical benefits in terms of the postoperative factors. Still, there are some points to be considered when using intraperitoneal instillation of lidocaine in a patient with an intra-abdominal infection like acute appendicitis. Although the primary cause of the intra-abdominal infection is removed and controlled, pelvic instillation entails the risk of changing a localized infection to generalized peritonitis. When considering the clinical conditions, intravenously injecting analgesics would probably be better than intraperitoneal instillation in the setting of serious intra-abdominal inflammatory conditions.
The weakness of this investigation is the lack of comparison of the plasma lidocaine concentrations between groups IP and IV. Therefore, although apparent observational comparisons were possible, the absorption rate of intraperitoneally instilled lidocaine and its systemic effect added to the local effect in group IP, compared to the systemically injected lidocaine in group IV, could not be investigated. A large-scale investigation will be required to assess the pharmacodynamic properties, which could be useful in determining which delivery method is superior and may well lead to discovering a better protocol.
The proper and superior method for intravenous delivery is not yet established. In previous studies, when lidocaine was injected in large toxic bolus infusions, a direct analgesic and morphine-sparing effect was observed, and continuous low-dose lidocaine infusions were shown to be beneficial only in postoperative properties failing in pain reduction [12, 16]. Therefore, in our study, in order to achieve a lasting analgesic effect and favorable postoperative outcomes, both bolus and continuous injection of lidocaine were used.
Another limitation of this study is that we excluded the patients with comorbidities. Therefore, the results cannot be extrapolated to all patients, nor can rare complications be completely ruled out.
An interesting point of this study is that intravenous lidocaine reduced the incidence of shoulder tip pain as well as did intraperitoneal lidocaine. Because the proposed cause of shoulder tip pain in laparoscopic procedures is diaphragmatic stretching with phrenic nerve neuropraxia [23, 37], it is not strange that intraperitoneal instillation of local anesthetic has been shown to effectively reduce shoulder tip pain. The effect of intravenous lidocaine on shoulder tip pain was previously not known. However, this result implies that the development of shoulder tip pain can be blocked by a systemic mechanism and not just by a peripheral block (diaphragm and phrenic nerve) alone.
Conclusion
In the US, many patients routinely receive a bolus of lidocaine injection prior to the administration of IV propofol. In spite of its popular use, the consequences of its use were neglected for a considerable time. Lidocaine administration in laparoscopy settings reduces postoperative pain when given either intravenously or intraperitoneally. Intraperitoneal instillation of lidocaine provides a significant reduction of pain and the requirement for postoperative analgesia without complications. However, the burden of an additional procedure during surgery and the probable risk for peritoneal contamination in patients with grave inflammation may be factors that limit its use. We demonstrated that preemptive administration of intravenous lidocaine injection is as effective as intraperitoneal instillation for reducing fentanyl consumption. The magnitude of pain reduction with intravenous lidocaine was equivalent to that of intraperitoneal instillation of a similar dosage without any adverse effects throughout the study. The major benefit of intravenous injection is that the steps of this procedure seem much easier and universally applicable regardless of the intra-abdominal condition, compared to that of peritoneal instillation.
We conclude by recommending that intravenous administration of lidocaine is not only effective, but is also a safe procedure and it can be a better alternative for reducing the pain of patients who are undergoing laparoscopic surgery.
References
Alexander JI (1997) Pain after laparoscopy. Br J Anaesth 79:369–378
Mouton WG, Bessell JR, Otten KT, Maddern GJ (1999) Pain after laparoscopy. Surg Endosc 13:445–448
Soper NJ, Brunt LM, Kerbl K (1994) Laparoscopic general surgery. N Engl J Med 330:409–419
Pasqualucci A, de Angelis V, Contardo R, Colo F, Terrosu G, Donini A, Pasetto A, Bresadola F (1996) Preemptive analgesia: intraperitoneal local anesthetic in laparoscopic cholecystectomy. A randomized, double-blind, placebo-controlled study. Anesthesiology 85:11–20
Neuhaus SJ, Watson DI (2004) Pneumoperitoneum and peritoneal surface changes: a review. Surg Endosc 18:1316–1322
Wills VL, Hunt DR (2000) Pain after laparoscopic cholecystectomy. Br J Surg 87:273–284
Watkins LR, Maier SF, Goehler LE (1995) Immune activation: the role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain 63:289–302
Cervini P, Smith LC, Urbach DR (2002) The effect of intraoperative bupivacaine administration on parenteral narcotic use after laparoscopic appendectomy. Surg Endosc 16:1579–1582
Ng A, Smith G (2002) I: Intraperitoneal administration of analgesia: is this practice of any utility? Br J Anaesth 89:535–537
Barczynski M, Konturek A, Herman RM (2006) Superiority of preemptive analgesia with intraperitoneal instillation of bupivacaine before rather than after the creation of pneumoperitoneum for laparoscopic cholecystectomy: a randomized, double-blind, placebo-controlled study. Surg Endosc 20:1088–1093
Maestroni U, Sortini D, Devito C, Pour Morad Kohan Brunaldi F, Anania G, Pavanelli L, Pasqualucci A, Donini A (2002) A new method of preemptive analgesia in laparoscopic cholecystectomy. Surg Endosc 16:1336–1340
Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, Hering W (2004) Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg 98:1050–1055
Groudine SB, Fisher HA, Kaufman RP Jr, Patel MK, Wilkins LJ, Mehta SA, Lumb PD (1998) Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg 86:235–239
Hollmann MW, Durieux ME (2000) Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology 93:858–875
Marret E, Rolin M, Beaussier M, Bonnet F (2008) Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg 95:1331–1338
Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL (2007) Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology 106(1):11–18; discussion 15–16
Bellows CF, Berger DH (2006) Infiltration of suture sites with local anesthesia for management of pain following laparoscopic ventral hernia repairs: a prospective randomized trial. JSLS 10:345–350
Meissner W, Mescha S, Rothaug J, Zwacka S, Goettermann A, Ulrich K, Schleppers A (2008) Quality improvement in postoperative pain management: results from the QUIPS Project. Dtsch Arztebl Int 105:865–870
Labaille T, Mazoit JX, Paqueron X, Franco D, Benhamou D (2002) The clinical efficacy and pharmacokinetics of intraperitoneal ropivacaine for laparoscopic cholecystectomy. Anesth Analg 94:100–105
Klein JR, Heaton JP, Thompson JP, Cotton BR, Davidson AC, Smith G (2000) Infiltration of the abdominal wall with local anaesthetic after total abdominal hysterectomy has no opioid-sparing effect. Br J Anaesth 84:248–249
Kaufman Y, Hirsch I, Ostrovsky L, Klein O, Shnaider I, Khoury E, Pizov R, Lissak A (2008) Pain relief by continuous intraperitoneal nebulization of ropivacaine during gynecologic laparoscopic surgery—a randomized study and review of the literature. J Minim Invasive Gynecol 15:554–558
Tsimoyiannis EC, Siakas P, Tassis A, Lekkas ET, Tzourou H, Kambili M (1998) Intraperitoneal normal saline infusion for postoperative pain after laparoscopic cholecystectomy. World J Surg 22:824–828
Tsimoyiannis EC, Glantzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H (1998) Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc 8:416–420
Papaziogas B, Argiriadou H, Papagiannopoulou P, Pavlidis T, Georgiou M, Sfyra E, Papaziogas T (2001) Preincisional intravenous low-dose ketamine and local infiltration with ropivacaine reduces postoperative pain after laparoscopic cholecystectomy. Surg Endosc 15:1030–1033
Coughlin SM, Karanicolas PJ, Emmerton-Coughlin HM, Kanbur B, Kanbur S, Colquhoun PH (2010) Better late than never? Impact of local analgesia timing on postoperative pain in laparoscopic surgery: a systematic review and metaanalysis. Surg Endosc 24:3167–3176
Koppert W, Dern SK, Sittl R, Albrecht S, Schuttler J, Schmelz M (2001) A new model of electrically evoked pain and hyperalgesia in human skin: the effects of intravenous alfentanil, S(+)-ketamine, and lidocaine. Anesthesiology 95:395–402
Koppert W, Ostermeier N, Sittl R, Weidner C, Schmelz M (2000) Low-dose lidocaine reduces secondary hyperalgesia by a central mode of action. Pain 85:217–224
Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E, Watanabe H, Namiki A (2002) Experimental incision-induced pain in human skin: effects of systemic lidocaine on flare formation and hyperalgesia. Pain 100:77–89
Wallace MS, Ridgeway BM, Leung AY, Gerayli A, Yaksh TL (2000) Concentration-effect relationship of intravenous lidocaine on the allodynia of complex regional pain syndrome types I and II. Anesthesiology 92:75–83
Orstavik K, Weidner C, Schmidt R, Schmelz M, Hilliges M, Jorum E, Handwerker H, Torebjork E (2003) Pathological C-fibres in patients with a chronic painful condition. Brain 126:567–578
Aguilar JS, Criado M, De Robertis E (1980) Inhibition by local anesthetics phentolamine and propranolol of [3H]quinuclydinyl benzylate binding to central muscarinic receptors. Eur J Pharmacol 68:317–326
Sugimoto M, Uchida I, Mashimo T (2003) Local anaesthetics have different mechanisms and sites of action at the recombinant N-methyl-d-aspartate (NMDA) receptors. Br J Pharmacol 138:876–882
Hollmann MW, Gross A, Jelacin N, Durieux ME (2001) Local anesthetic effects on priming and activation of human neutrophils. Anesthesiology 95:113–122
Rabert DK, Koch BD, Ilnicka M, Obernolte RA, Naylor SL, Herman RC, Eglen RM, Hunter JC, Sangameswaran L (1998) A tetrodotoxin-resistant voltage-gated sodium channel from human dorsal root ganglia, hPN3/SCN10A. Pain 78:107–114
Akopian NS, Sarkisian NV, Karapetian MA (1999) Involvement of central and peripheral cholinergic structures in regulation of cerebral electric activity and cardiac function in rabbits during hypoxia. Aviakosm Ekolog Med 33:28–31
Nagy I, Woolf CJ (1996) Lignocaine selectively reduces C fibre-evoked neuronal activity in rat spinal cord in vitro by decreasing N-methyl-d-aspartate and neurokinin receptor-mediated post-synaptic depolarizations; implications for the development of novel centrally acting analgesics. Pain 64:59–70
Palmes D, Rottgermann S, Classen C, Haier J, Horstmann R (2007) Randomized clinical trial of the influence of intraperitoneal local anaesthesia on pain after laparoscopic surgery. Br J Surg 94:824–832
Acknowledgment
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A100054).
Disclosures
Drs. Tae Han Kim, Hyun Kang, Joon Hwa Hong, Jun Seok Park, Chong Wha Baek, Jin Yun Kim, Yong Hun Jung, and Hyang Kyoung Kim have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, T.H., Kang, H., Hong, J.H. et al. Intraperitoneal and intravenous lidocaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. Surg Endosc 25, 3183–3190 (2011). https://doi.org/10.1007/s00464-011-1684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1684-3