Abstract
Background
Currently, laparoscopic appendectomy (LA) provides a safe and effective alternative to open appendectomy (OA), but its use remains controversial. This study aimed to evaluate the efficiency and safety of LA through a metaanalysis.
Methods
Randomized controlled trials (RCTs) comparing LA and OA published between January 1992 and February 2010 were included in this study. Strict literature appraisal and data extraction were carried out independently by two reviewers. A metaanalysis then was performed to evaluate operative time, hospital cost, postoperative complications, length of analgesia, bowel function recovery, day liquid diet began, hospital stay, and return to work and normal activity.
Results
The metaanalysis comprised 25 RCTs involving 4,694 patients (2,220 LA and 2,474 OA cases). No significant differences were found between the LA and OA groups in terms of age, gender, body mass index (BMI), or type of appendiceal inflammation. Compared with OA, LA showed advantages of fewer postoperative complications (odds ratio [OR], 0.74; 95% confidence interval [CI], 0.55–0.98; p = 0.04), less pain (length of analgesia: weighted mean difference [WMD], −0.53; 95% CI, −0.91 to −0.15; p = 0.007), earlier start of liquid diet (WMD, −0.51; 95% CI, −0.75 to −0.28; p < 0.0001), shorter hospital stay (WMD, −0.68; 95% CI, −1.02 to −0.35; p < 0.0001), and earlier return to work (WMD, −3.09; 95% CI, −5.22 to −0.97; p = 0.004) and normal activity (WMD, −4.73; 95% CI, −6.54 to −2.92; p < 0.00001), but a comparable hospital cost (WMD of LA/OA ratio, 0.11; 95% CI, −0.18 to 0.40; p = 0.47) and a longer operative time (WMD, 10.71; 95% CI, 6.76–14.66; p < 0.00001).
Conclusion
Despite the longer operative time, LA results in less postoperative pain, faster postoperative rehabilitation, a shorter hospital stay, and fewer postoperative complications than OA. Therefore, LA is worth recommending as an effective and safe procedure for acute appendicitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic appendectomy was first described by Semm [1] in 1983. Subsequently, Pier et al. [2] reported on a large case series of laparoscopic appendectomy (LA) for acute appendicitis and demonstrated that this technique was safe and could achieve the same results as open appendectomy (OA). In the past 20 years, numerous randomized prospective studies, metaanalyses, and reviews have been published comparing LA with OA [3–8].
Supporters of LA maintain that in addition to improved diagnostic accuracy, LA confers advantages to patients in terms of fewer wound infections [9], less pain [10], faster recovery [3], and earlier return to work [11]. However, some researchers disapprove of using LA because it is more time consuming, has increased hospital costs, and offers no advantages in terms of postoperative recovery [5]. Moreover, definitive conclusions still cannot be drawn due to the heterogeneity of measured variables in different trials and many other defects in methodology [12]. Therefore, the use of LA remains controversial, in contrast to the wide acceptance of laparoscopic cholecystectomy since its innovation.
To compare LA with OA, we performed a metaanalysis of randomized controlled trials (RCTs) conducted between 1992 and 2010 to evaluate operative time, hospital cost, postoperative complications, length of analgesia, bowel function recovery, day liquid diet began, hospital stay, and return to work and normal activity.
Materials and methods
Literature search
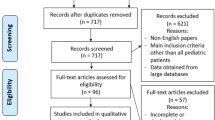
A comprehensive literature search of the Medline, Embase, Current Contents, and PubMed databases under the headings of “acute appendicitis,” “appendectomy,” and “laparoscopic appendectomy” was performed electronically for the span between January 1992 and February 2010. The search was limited to RCTs published in English. All the full texts or abstracts and their related citations were scanned and reviewed.
Inclusion criteria
The inclusion criteria specified RCT literatures comparing the effectiveness and safety of LA and OA for acute appendicitis; studies concerning operative time, hospital cost, postoperative complications, length of analgesia, bowel function recovery, day liquid diet began, hospital stay, and return to work and normal activity; inclusion of only the most recent article from the same institution when several studies reporting the same patients were found; and studies with any sample size.
Exclusion criteria
The exclusion criteria ruled out articles of less information by the aforementioned criteria; studies in which at least four variables of interest could not be derived from the published results; and studies that used variations on the standard laparoscopic technique including laparoscope-assisted or single-trocar appendectomy.
Methods of review
The quality of the pooled studies was assessed strictly by two authors (B.W. and H.B.W.), especially the randomization. The data extraction and critical appraisal were performed independently by the same two authors. First, the elementary data of the patients including age, gender, body mass index (BMI), and types of appendiceal inflammation were extracted to evaluate the concordance of the subject. Second, the items of safety including operative time, hospital cost ratio, and postoperative complications were collected.
As described in the included trials, the operative time was recorded as the time from the first incision to the placement of the last suture in the skin. Because the hospital costs of the two procedures differed tremendously in terms of ages and countries, we used the hospital cost ratio (LA/OA) to compare the total costs of LA and OA.
The postoperative complications were summed including wound infection, postoperative ileus, bleeding from the appendicular artery or place of trocar insertion, intraabdominal abscess, pulmonary complications, and wound infection. The overall postoperative complications and the subcategory including wound infection, intraabdominal abscess, and ileus were compared. In general, only a trifle of blood loss occurred and hardly any postoperative mortality, so these two variables were not included. Finally, the length of analgesia, bowel function recovery, day liquid diet began, hospital stay, and return to work or normal activity were extracted to evaluate the effectiveness of the two procedures for postoperative rehabilitation.
The length of analgesia usage included the days that analgetic medication was given to the patient on demand. Bowel function recovery was determined by bowel tones and breaks wind from anal. Patients were discharged after reaching full mobility and after clinical examinations, body temperature, and white blood cell counts were normal. The length of hospital stay was recorded as the number of days in the hospital after the day of surgery. The days needed for a return to work or normal activity were determined by patient follow-up assessment for at least 1 month.
During the data extracting, when the trials had reported medians and ranges instead of means and standard deviations, we assumed that medians were equal to means and that the estimated standard deviation was equivalent to one-fourth of the reported range. If neither a range nor any other measure of dispersion was available, then the standard deviation was estimated by halving the mean or the median.
Statistical analysis
The analysis was completed using the Review Manager 4.2.5 statistical package by Cochrane Collaboration (Guangzhou city, China). Continuous data presented in the same scale (e.g., operating time, length of analgesia, and postoperative hospital stay) were analyzed using weight mean difference (WMD) with 95% confidence intervals (CIs). Due to the rarity of some events, dichotomous data (e.g., postoperative complications) were analyzed using Petos odds ratios (ORs). A randomized-effects model was used due to the clinical heterogeneity of the included studies. Heterogeneity was evaluated using the chi-square test. All p values less than 0.1 were considered significant for heterogeneity. A p value less than 0.05 was considered significant for overall effects.
Results
Characteristics of the pooled RCTs
The metaanalysis included 25 studies involving 4,694 patients (2,220 LA and 2,474 OA cases). The characteristics, including modified Jadad scales of the pooled RCTs, are summarized in Table 1. Most of the pooled RCTs were high-quality trials (88%) according to modified Jadad scales [13]. The two groups did not differ significantly in terms of age (Z = 0.08; p = 0.94), gender (Z = 1.09; p = 0.28), BMI (Z = 1.19; p = 0.23), or type of appendiceal inflammation (Z = 1.05; p = 0.33).
Tests for heterogeneity and results of the metaanalysis
The pooled data (WMDs or ORs) for the nine outcomes are summarized in Table 2.
Operative time
The test for heterogeneity showed that the two groups were heterogeneous (p < 0.00001) in operative time, and a randomized-effect model was used. The operative time was 10.71 min longer in the LA group than in the OA group (WMD, 10.71; 95% CI, 6.76–14.66; p < 0.00001), as shown in Fig. 1a.
Hospital cost ratio (LA/OA)
Considering the different operative costs for different age groups and countries, we used the hospital cost ratio (LA/OA) to compare the total costs for LA and OA. The results showed that hospital cost for LA was 11% higher than for OA. But there was no significant cost difference between two procedures (Z = 0.73; p = 0.47), as shown in Fig. 1b.
Postoperative complications
The effect size of the difference in OR was analyzed by a randomized-effect model (χ = 37.49; p = 0.02). The combined data from 23 trials showed that the total incidence of LA was 9.90% (208/2,100), significantly less than the 13.34% (314/2,354) for OA (Z = 2.09; p = 0.04). The randomized-effect OR was 0.74 (95% CI, 0.55–0.98), indicating that LA carries a reduced incidence of postoperative complications, as shown in Fig. 1c.
A subcategory analysis of postoperative complications including wound infection, intraabdominal abscess, and postoperative ileus was performed. The results showed that the incidence of wound infection for LA was significantly less than for OA (Z = 5.55; p < 0.00001; 95% CI, 0.30–0.56), but no significant difference was found for intraabdominal abscess (Z = 1.62; p = 0.11; 95% CI, 0.93–2.14) or postoperative ileus (Z = 0.97; p = 0.33; 95% CI, 0.44–1.32) (Fig. 2).
Length of analgesia
Only seven trials reported the postoperative length of analgesia, with five trials showing a statistically significant reduction in the LA group compared with the OA group. The result showed that the length of analgesia in the LA group was significantly less than in the OA group (WMD, −0.53; 95% CI, −0.91 to −0.15; p = 0.007) using a randomized-effect model (test for heterogeneity: χ2 = 112.38; p < 0.00001), as shown in Fig. 3a.
Bowel function recovery and day liquid diet began
Five trials reported postoperative bowel function recovery, and seven trials reported the day liquid diet began. The result showed no significant difference in bowel function recovery between LA and OA (WMD, −0.15; 95% CI, −0.40 to 0.09; p = 0.23), but the day liquid diet began in the LA group was 0.51 days earlier than in the OA group (WMD, −0.51; 95% CI, −0.75 to −0.28; p < 0.0001), as shown in Fig. 3b, c.
Hospital stay
Of the 23 trials reporting the postoperative hospital stay, 16 showed a significantly shorter stay in the LA group than in the OA group. The results of the metaanalysis showed a significantly shorter hospital stay in the LA group than in the OA group (Z = 4.02; p < 0.0001), with a randomized-effect WMD of −0.68 (95% CI, −1.02 to −0.35), as shown in Fig. 4a.
Return to work and normal activity
The results showed that the LA group had an earlier return to work (WMD, −3.09; 95% CI, −5.22 to −0.97; p = 0.004) and normal activity (WMD, −4.73; 95% CI, −6.54 to −2.92; p < 0.00001) than the OA group. The differences were significant, as shown in Fig. 4b, c.
Sensitivity and bias test
A randomized- or fixed-effects model was used due to the test of heterogeneity of the included studies. A fixed-effects model was used if the heterogeneity test had no significance, and a randomized-effects model was used when test of heterogeneity showed a significant difference. In this study, the results for all variables were heterogeneous, so randomized-effects models were used.
The funnel plot is a scatter plot of the treatment effects estimated from individual trials on the horizontal axis (WMD or OR) against a measure of study size on the vertical axis (SE [WMD] or SE [log OR]). The plot resembles a symmetric inverted funnel (the 95% CI). The name “funnel plot” is based on the fact that precision in estimating the underlying treatment effect increases as the sample size of the component studies increases. Funnel plots provide an estimate of the robustness and bias of the findings.
Figure 5 suggests that the findings for all variables were quite robust, resembling a symmetric funnel, and that the publication biases were absent or not very serious. A funnel plot functioning as a sensitivity test together with an exhaustive literature search conferred a substantial degree of confidence in the findings of this metaanalysis.
Discussion
Appendectomy has become the gold standard surgical intervention for appendicitis since its first description by McBurney [32] in 1894. It has remained virtually unchanged for more than a century because of its proven efficacy and safety. More than 20 years have elapsed since LA was first reported by Semm [1]. However, because studies have failed to demonstrate overwhelming benefits with LA (as were visible with laparoscopic cholecystectomy), its use had not been widely accepted and was the subject of continuous debate [33–38].
Late in the last century, numerous RCTs failed to demonstrate any benefit of the laparoscopic over the open approach. For example, an increased operative time, a comparable hospital stay, and no difference in return to normal activity were noted for LA [33]. These flaws outweighed any improvement in wound complication, recovery time, or cosmesis.
With the development of minimally invasive surgery and laparoscopic techniques, the popularity of LA has increased. Current studies indicate a shift in favor of LA, probably due to the increase in laparoscopic exposure at all levels of surgical training. Currently, LA is considered to be a safe and effective alternative to OA [39, 40]. It is associated with benefits of visualization, diminution of incisional complication rates, decreased hospital stay, reduced time until return to activity, and improved cosmesis [41–44].
To investigate further the safety and effectiveness of LA, we present a systematic review and metaanalysis of the therapeutic outcomes from randomized trials of laparoscopic versus open appendectomy. The metaanalysis is a statistical tool that can be used to evaluate the literature in both qualitative and quantitative ways, accounting for variations in characteristics that can influence the overall estimate of outcomes of interest. It can increase the sample size and decrease the β error as extensively as possible, and it has been used extensively as a statistical method for systematic review [38, 45].
The results of this metaanalysis suggested that LA took significantly longer than OA (WMD, 10.71; 95% CI, 6.76–14.66; p < 0.00001). However, considering the increased instrumentation during laparoscopic surgery and the setup time involved, it is not surprising that LA takes longer than its open equivalent. Moreover, the benefit of LA is unlikely to be the length of operation but rather the quicker healing, with smaller operative wounds and earlier recovery.
The social economics of the procedure was another important factor in the spread of LA. As reported by some authors, the hospital cost for LA was higher than for OA due to the use of consumables and the high dependency on laparoscopic apparatus and instruments. But in the current study, the hospital cost showed no significant difference between LA and OA (WMD, 0.11; 95% CI, −0.18 to 0.40; p = 0.47). The length of analgesia was shorter in the LA group than in the OA group (WMD, −0.53; 95% CI, −0.91 to −0.15; p = 0.007).
The assessment of postoperative pain was blurry because of its subjectivity, and in some trials, visual analog pain scores (VAS) were used. But in this study, we used length of analgesia to represent postoperative pain in order to unify this index in different studies. The result indicated reduced pain with LA.
The outcomes showed an apparent tendency favoring LA in terms of postoperative bowel function recovery (WMD, −0.15; 95% CI, −0.40 to 0.09; p = 0.23), but the difference was not significant. Moreover, it must be noted that the number of studies reporting this variable was small. The day that a liquid diet began was earlier in the LA group than in the OA group (WMD, −0.51; 95% CI, −0.75 to −0.28; p < 0.0001). This may be explained by the smaller interference to enterokinesia and the internal environment of the abdominal cavity during LA surgery.
The hospital stay differed significantly among the included trials, although the hospital discharge criteria differed from country to country due to differences in health care systems. The results for the metaanalysis of hospital stays suggested that LA patients were discharged earlier than OA patients (WMD, −0.68; 95% CI, −1.02 to −0.35; p < 0.0001). The outcomes also showed that the LA patients returned to work and normal activity earlier due to the smaller invasion of laparoscopic surgery.
Postoperative complications usually are considered an assessment of a procedure’s safety. The common complications of appendectomy are wound infection, intraabdominal abscess, postoperative ileus, bleeding, and the like. In the current review, we used the overall incidence of postoperative complications to assess the safety of LA. The metaanalysis results showed that the overall incidence of postoperative complications in LA group was lower than in the OA group (Z = 2.09; p = 0.04). The subcategory analysis indicated a lower incidence of wound infection in the LA group (Z = 5.55; p < 0.00001) and a similar lower incidence of intraabdominal abscess and postoperative ileus than in the OA group. However, there were tendencies supporting OA (e.g., less intraabdominal abscess) and tendencies supporting LA (e.g., less ileus). There may be some explanations. First, laparoscopy reduced wound infection because the inflamed appendix was extracted within the trocar and did not touch the abdominal wall. Second, although LA allowed complete survey of the peritoneal cavity and superior visualization, thorough disposal of the inflammatory exudation did not surpass that of OA. Finally, the minimally invasive technique reduced the interference to the microenvironment and injury to the intestinal serous membrane, then lightened the adherence between the intestines, thus decreasing the incidence of adhesive ileus.
We can therefore draw the conclusion that despite a longer operative time, LA results in less postoperative pain, faster postoperative rehabilitation, a shorter hospital stay, and fewer postoperative complications than OA. Therefore, LA is worth recommending as an effective and safe procedure for acute appendicitis.
However, as matter of course, metaanalysis has its own limitations, such as a slight difference in methodology and definition of criteria for some items among different studies, a different outcome assessment between studies, a deficiency of blindness, and the like. These limitations may decrease the reliability of the metaanalysis. Therefore, it is important to assess the quality and sensitivity of the metaanalysis. In this study, heterogeneity of the sample was tested, and a randomized- effect model was used to maintain its sensitivity. Moreover, the funnel plot was used to test publication bias.
Due to the restriction of items of interest, some aspects of interest were neglected. For example, the subgroup of obese patients with a high BMI was not investigated in this systematic review. As another example, the symptoms of some acute abdomens can be similar to those of appendicitis and difficult to diagnose differentially. The disorders that can be confused with appendicitis include Meckel diverticulitis, cholecystitis, and colic perforation, especially adnexitis, ovarian cysts, and extrauterine pregnancies in women. Laparoscopy allows a complete survey of the peritoneal cavity. This can be considered as another benefit in favor of LA. Therefore, the study further highlights the need for a large sample and high-quality randomized trials.
Conclusion
The current metaanalysis showed that although LA has a longer operative time, it results in less postoperative pain, faster postoperative rehabilitation, a shorter hospital stay, and fewer postoperative complications than OA. Therefore, the LA procedure is a useful tool in the treatment of acute appendicitis and worth recommending as an effective and safe procedure for this disorder.
References
Semm K (1983) Endoseopic appendectomy. Endoscopy 15:59–64
Pier A, Gotz F, Bacher C (1991) Laparoscopic appendectomy in 625 cases: from innovation to routine. Surg Laparosc Endosc 1:8–13
Klingler A, Henle KP, Beller S, Rechner J, Zerz A, Wetscher GJ, Szinicz G (1998) Laparoscopic appendectomy does not change the incidence of postoperative infectious complications. Am J Surg 175:232–235
Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyö G, Graffner H, Hallerbäck B, Johansson B, Anderberg B, Wenner J, Ringqvist I, Sörensen S (1999) Prospective randomized multicentre study of laparoscopic versus open appendicectomy. Br J Surg 86:48–53
Williams MD, Collins JN, Wright TF, Fenoglio ME (1996) Laparoscopic versus open appendectomy. South Med J 89:668–674
Bennett J, Boddy A, Rhodes M (2007) Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech 17:245–255
Kim CB, Kim MS, Hong JH, Lee HY, Yu HS (2004) Is laparoscopic appendectomy useful for the treatment of acute appendicitis in Korea? A meta-analysis. Yonsei Med J 45:7–16
Eypasch E, Sauerland S, Lefering R, Neugebauer EA (2002) Laparoscopic versus open appendectomy: between evidence and common sense. Dig Surg 19:518–522
Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, Menzies BL (1996) Laparoscopic versus open appendectomy: prospective randomized trial. World J Surg 20:17–21
Milewczyk M, Michalik M, Ciesielski M (2003) A prospective, randomized, unicenter study comparing laparoscopic and open treatments of acute appendicitis. Surg Endosc 17:1023–1028
Heikkinen TJ, Haukipuro K, Hulkko A (1998) Cost-effective appendectomy: open or laparoscopic? A prospective randomized study. Surg Endosc 12:1204–1208
Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R (2005) Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 242:439–450
Jadad AR, Moore RA, Carroll D (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Kum CK, Ngoi SS, Goh PM, Tekant Y, Isaac JR (1993) Randomized controlled trial comparing laparoscopic and open appendicectomy. Br J Surg 80:1599–1600
Tate JJ, Dawson JW, Chung SC, Lau WY, Li AK (1993) Laparoscopic versus open appendicectomy: prospective randomised trial. Lancet 342:633–637
Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, Custer MD III, Harrison JB (1994) A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg 219:725–731
Martin LC, Puente I, Sosa JL, Bassin A, McKenney MG, Ginzburg E, Sleeman D (1995) Open versus laparoscopic appendectomy: a prospective randomized comparison. Ann Surg 222:256–261 discussion 261–262
Cox MR, McCall JL, Toouli J, Padbury RT, Wilson TG, Wattchow DA, Langcake M (1996) Prospective randomized comparison of open versus laparoscopic appendectomy in men. World J Surg 20:263–266
Mutter D, Vix M, Bui A, Evrard S, Tassetti V, Breton JF, Marescaux J (1996) Laparoscopy not recommended for routine appendectomy in men: results of a prospective randomized study. Surgery 120:71–74
Minné L, Varner D, Burnell A, Ratzer E, Clark J, Haun W (1997) Laparoscopic vs open appendectomy: prospective randomized study of outcomes. Arch Surg 132:708–712
Macarulla E, Vallet J, Abad JM, Hussein H, Fernández E, Nieto B (1997) Laproscopic versus open appendectomy: a prospective randomized trial. Surg Laparosc Endosc 7:335–339
Kazemier G, de Zeeuw GR, Lange JF, Hop WC, Bonjer HJ (1997) Laparoscopic vs open appendectomy: a prospective randomized clinical trial. Surg Endosc 11:336–340
Long KH, Bannon MP, Zietlow SP, Helgeson ER, Harmsen WS, Smith CD, Ilstrup DM, Baerga-Varela Y, Sarr MG (2001) A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: clinical and economic analyses. Surgery 129:390–400
Pedersen AG, Petersen OB, Wara P, Ronning H, Qvist N, Laurberg S (2001) Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg 88:200–205
Lintula H, Kokki H, Vanamo K (2001) Single-blind randomized clinical trial of laparoscopic versus open appendicectomy in children. Br J Surg 88:510–514
Oka T, Kurkchubasche AG, Bussey JG, Wesselhoeft CW Jr, Tracy TF Jr, Luks FI (2004) Open and laparoscopic appendectomy are equally safe and acceptable in children. Surg Endosc 18:242–245
Ignacio RC, Burke R, Spencer D, Bissell C, Dorsainvil C, Lucha PA (2004) Laparoscopic versus open appendectomy: what is the real difference? Results of a prospective randomized double-blinded trial. Surg Endosc 18:334–337
Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, Montgomery A (2005) Randomized clinical trial of laparoscopic versus open appendicectomy for confirmed appendicitis. Br J Surg 92:298–304
Olmi S, Magnone S, Bertolini A, Croce E (2005) Laparoscopic versus open appendectomy in acute appendicitis: a randomized prospective study. Surg Endosc 19:1193–1195
Tzovaras G, Liakou P, Baloyiannis I, Spyridakis M, Mantzos F, Tepetes K, Athanassiou E, Hatzitheofilou C (2007) Laparoscopic appendectomy: differences between male and female patients with suspected acute appendicitis. World J Surg 31:409–413
Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, Guo WP, Chen TF, Wang TB (2010) Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc 24:266–269
McBurney C (1894) The incision made in the abdominal wall in case of appendicitis with a description of a new method of operating. Ann Surg 20:38–43
Fischer CP, Castaneda A, Moore F (2002) Laparoscopic appendectomy: indications and controversies. Semin Laparosc Surg 9:32–39
Schroder DM, Lathrop JC, Lloyd LR, Boccaccio JE, Hawasli A (1993) Laparoscopic appendectomy for acute appendicitis: is there really any benefit? Am Surg 59:541–548
Temple LK, Litwin DE, McLeod RS (1999) A meta-analysis of laparoscopic versus open appendectomy in patients suspected of having acute appendicitis. Can J Surg 42:377–383
Meynaud-Kraemer L, Colin C, Vergnon P et al (1999) Wound infection in open versus laparoscopic appendectomy: a meta-analysis. Int J Technol Assess Health Care 15:380–391
Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B (1999) Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc 9:17–26
Chung RS, Rowland DY, Li P, Diaz J (1999) A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg 177:250–256
Slim K, Chipponi J (2006) Laparoscopy for every acute appendicitis? Surg Endosc 20:1785–1786
Näf R, Buchmann P (2005) Is open appendectomy still up-to-date? Ther Umsch 62:111–117
Sauerland S, Lefering R, Neugebauer EA (2004) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 18:CD001546
Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B (1995) A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy: Laparoscopic Appendectomy Study Group. Am J Surg 169:208–213
Azaro EM, Amaral PC, Ettinger JE, Souza EL, Fortes MF, Alcântara RS, Regis AB, Sousa MM, Fogagnoli WG, do Carmo VM, Galvão TD, Stagliorio EP, Santana PA Jr, Fahel E (1999) Laparoscopic versus open appendicectomy: a comparative study. JSLS 3:279–283
Attwood SE, Hill AD, Murphy PG, Thornton J, Stephens RB (1992) A prospective randomized trial of laparoscopic versus open appendectomy. Surgery 112:497–501
Sauerland S, Lefering R, Holthausen U, Neugebauer EA (1998) Laparoscopic vs conventional appendectomy: a meta-analysis of randomised controlled trials. Langenbecks Arch Surg 383:289–295
Acknowledgment
The study was supported by the Medical Science Found of Guangdong Province (no. 2009078).
Disclosures
Bo Wei, Cui-Lling Qi, Tu-Feng Chen, Zong-Heng Zheng, Jiang-Long Huang, Bao-Guang Hu, and Hong-Bo Wei have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Bo Wei, Cui-Lliang Qi authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wei, B., Qi, CL., Chen, TF. et al. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc 25, 1199–1208 (2011). https://doi.org/10.1007/s00464-010-1344-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1344-z