Abstract
Aim
To identify variables that predict in-hospital length of stay (LOS) after laparoscopic ventral hernia repair (LVHR).
Methods
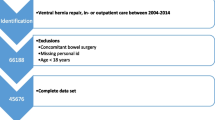
Univariate analysis of patient and intraoperative variables was conducted on an operating room database of LVHRs performed from April 2001 to April 2009. Analysis was performed using either chi-square or linear trend analysis, as appropriate. A multivariate logistic regression model was created manually, to determine independent variables that predict LOS. p Value <0.05 was considered significant.
Results
A total of 221 patients, with mean age of 56 years (range 25–88 years) underwent LVHR, for a total of 121 incisional and 100 primary ventral hernias. Of patients, 40% had incarcerated hernias and 25% had complex hernias (defined as multiple points of weakness on the anterior abdominal wall). The overall conversion rate to open operation was 6%. Mean LOS was 1.54 days (range 0–22 days). Eighty-six patients (39%) were discharged on the day of the procedure. Variables associated with significantly longer LOS on univariate analysis were incisional hernia (p = 0.000009), mesh size (p = 0.00007), complex hernia (p = 0.00009), incarcerated hernia (p = 0.0004), patient age (p = 0.0006), need for lysis of adhesions (p = 0.001), and female gender (p = 0.01). American Society of Anesthesiologists (ASA) grade >2, conversion to open procedure, and recurrent hernia were not associated with longer LOS. Four factors were independently associated with significant longer length of stay on multivariate logistic regression analysis (p < 0.05): mesh size (p = 0.00005), incarcerated hernia (p = 0.002), patient age (p = 0.018), and complex hernia (p = 0.035).
Conclusions
Mesh size, incarcerated hernia, patient age, and complex hernia predict longer length of stay after laparoscopic ventral hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Incisional hernias complicate 3–13% of the 4–5 million laparotomies performed in the USA every year [1–6]. Ventral hernias are the second most common abdominal hernias after inguinal hernias [7].
Laparoscopic ventral hernia repair (LVHR) has been associated with reduced length of hospital stay (LOS), and lower rates of wound complications and recurrence. LVHR facilitates visualization of secondary defects and, in turn, allows more accurate placement of the prosthesis with adequate overlap. This may account for lower recurrence rates.
Every ventral hernia repair poses a challenge to the surgeon, with various patient and hernia factors potentially affecting postoperative outcomes. The aim of this study is to identify patient and intraoperative variables that significantly predict in-hospital LOS after LVHR.
Patients and methods
Charts of all patients who underwent LVHR at a teaching hospital from April 2001 through April 2009 were reviewed. LVHR included repair of incisional, umbilical, epigastric, and spigelian hernias. Data were retrieved from an operating room database prospectively maintained by the hospital, the hospital’s electronic medical records, and chart review of outpatient visits. Data analyzed included the following: basic demographic information; ASA grade; hernia location; hernia complexity (defined as multiple points of weakness on the anterior abdominal wall); primary versus recurrent hernia; incisional versus primary hernia; intraoperative technical details such as mesh type, mesh size (as a surrogate for hernia size), lysis of adhesions (LOA), and details of mesh fixation; conversion; length of procedure (LOP); intraoperative and postoperative complications; and length of stay. Analysis was performed using either chi-square or linear trend analysis, as appropriate. A multivariate logistic regression model was created manually, to determine independent variables predicting LOS. The study was approved by the hospital’s Institutional Review Board.
Technique of repair
Pneumoperitoneum is achieved either with a lateral upper-quadrant Veress needle, open Hasson technique, or an optical port system, as per surgeon preference. Incarcerated hernias are then reduced, and lysis of adhesions are undertaken to define the hernia. Prosthetic mesh is then secured in an intraperitoneal fashion with transfascial fixation sutures and tacks with 3–5 cm overlap from the edges of the hernia. Transfascial sutures are usually placed at 3, 6, 9, and 12 O’clock positions in order to secure the mesh. Tacks are then placed in between the sutures at 1-cm intervals. If a large hernia is encountered, further transfascial sutures are placed in order to secure the mesh.
Results
Descriptive analysis
A total of 221 patients, with mean age of 56.54 years (range 25–88 years), underwent LVHR. Fifty-one percent of patients were female. There were a total of 121 incisional and 100 primary hernias (79 umbilical hernias, 16 epigastric hernias, and 5 spigelian hernias).
There were fifty-five patients with ASA grade >2. One hundred eighty-one patients (82%) were undergoing their first hernia operation. Mean body mass index (BMI) of the patients in the cohort was 32.3 kg/m2 (±6.2 kg/m2, range 17–50 kg/m2). Fifty-four (24.5%) of the patients were found to have complex hernias. Eighty-seven patients (40%) had incarcerated hernias. Seventy-five percent of these patients had incarceration of the omentum; the remaining patients had incarceration of the intestines. Eighteen percent of the patients had no adhesions; the remaining patients needed varying extents of LOA. The omentum was the most common organ involved in the LOA (58%), followed by small bowel (20%), colon (3%), and small bowel and colon (1%).
Mean mesh area was 192.65 cm2 (60–2,367 cm2). Transfascial sutures were used for mesh fixation in 88% of the patients. Commonly, either one central or four transfascial sutures were placed at the borders of the mesh, as mentioned earlier in the “Technique of repair” section (sutures used per case: mean 2, median 4). Composite mesh made of polypropylene and polytetrafluoroethylene (PTFE) was used in the majority (60%) of patients. Polypropylene mesh with a differential coating to the visceral surface was used in 21% of the patients. The rest of the patients were repaired using PTFE mesh.
Mean LOP was 94 min (range 28–418 min). Estimated blood loss was <50 cc in 95% of cases (range <50 to 500 cc). The overall conversion rate was 5.8%. Cases were converted to open when it was deemed unsafe to proceed with laparoscopic lysis of adhesions. There were no inadvertent or unrecognized hollow viscous injuries in any of the patients.
Mean LOS was 1.54 days (range 0–22 days). Eighty-six patients (38.9%) were discharged on the same day as the procedure. Sixty percent of patients with primary hernias were discharged on the same day, and 90% were discharged on postoperative day 1. Mean surface area of mesh used to repair patients with primary hernias who stayed longer than postoperative day 1 was 224 cm2. This approximated the mean mesh size used to repair incisional hernias (241 cm2). LOS was significantly higher among patients with incarcerated hernias (2.31 versus 1.04 days). Mean LOS among patients with incarcerated intestines was 3.63 days, which was significantly higher compared with patients whose hernias were incarcerated with omentum (1.89 days). LOS was significantly longer among patients aged 65 years or older (2.3 versus 1.1 days).
Postoperative complications are presented in Table 1. Ileus was the most common postoperative complication and occurred in 17 patients (7.7%). Patients who developed postoperative ileus stayed in hospital for significantly longer (5.94 versus 1.97 days). Ileus rates were also higher among patients with incarcerated hernias (12.6 versus 4.4%). Patients who had intestinal involvement in the incarcerated hernia had a higher ileus rate compared with patients with omental involvement (18 versus 10.7%).
Three patients who were independent prior to admission were discharged to a skilled nursing facility. All three of these patients were older than 75 years, and their postoperative course was complicated by ileus, atrial fibrillation, and mesh infection, respectively.
Univariate analysis
Variables associated with significantly longer LOS on univariate analysis were incisional hernia (p = 0.000009), mesh size (p = 0.00007), complex hernia (p = 0.00009), incarcerated hernia (p = 0.0004), patient age (p = 0.0006), LOA (p = 0.001), and female gender (p = 0.01). ASA grade >2, conversion to open procedure, recurrent hernia, and BMI were not associated with longer length of stay (Table 2).
Logistic regression analysis
Four factors were independently associated with longer LOS on multivariate logistic regression analysis (p < 0.05): hernia mesh size (p = 0.00005), incarcerated hernia (p = 0.002), patient age (p = 0.018), and complex hernia (p = 0.035) (Table 3).
Discussion
Since Leblanc et al. [8] reported the first LVHR in 1992, this technique has generated significant interest with its reduced LOS, and lower rate of wound complications and recurrence rates [9–12]. These benefits, however, are offset by higher risk of procedure-related complications, especially unrecognized hollow viscous injury, which can lead to sepsis and death [13]. LVHR is based on the open underlay technique of hernia repair, as described by Stoppa [14], Rives et al. [15], and Wantz [16], with placement of the mesh in intraperitoneal position with significant overlap.
Association between primary ventral hernia repair, decreased need for adhesiolysis, and decreased complication and failure rates as compared with repair of incisional ventral hernias has been reported [17]. Open repair of large (>10 cm) as compared with small (<6 cm) incisional ventral hernia is associated with higher incidence of seroma formation and wound infection [18, 19]. Mean mesh size used to repair primary hernias among patients who stayed longer than one postoperative day approximated the mean mesh size used in patients with incisional hernias, illustrating the significance of hernia size as a predictor of LOS.
In a study of a relatively small cohort of 50 patients who underwent LVHR, Raftopoulos et al. [20] found two factors associated with longer LOS: hernia size and repair of incisional ventral hernia. Their conclusions agree with the results of the univariate analysis of the current study. Shah et al., in their review of 112 patients, showed that the laparoscopic approach could be safely applied in repair of incarcerated ventral hernia [21]. Mean in-hospital LOS in their study was similar to the LOS of the 87 patients with incarcerated hernia in the current study (2.8 versus 2.31 days). Saber et al. [22] and Tessier et al. [23] showed that LVHR in the elderly is associated with longer LOS as compared with a younger group of patients. In our experience, mean LOS is significantly longer among older patients, and a smaller percentage of older patients were discharged on the same day as their procedure.
Incisional hernia repairs have been reported to be twice as common in female as compared with male patients [24, 25]. It has been hypothesized that the higher incidence of incisional hernia among female patients may be due to the higher number of laparotomy incisions related to obstetric and gynecologic indications, especially hysterectomy [26]. Incisional hernias are seen more frequently in females and are associated with greater need for adhesiolysis. Incisional hernias tend to be larger, frequently incarcerated, and more complex as compared with primary hernias. They are also commonly seen in the elderly population as compared with primary ventral hernias. Consequently, this may explain the fact that incisional hernia, female gender, and need for lysis of adhesions, which are significant predictors of LOS on linear regression and univariate analysis, do not add to the multivariate logistic regression model.
A shortcoming of the current study is its retrospective nature. Studies where the data is collected prospectively, including size of the hernia itself, are required to confirm the findings of the current study. Although incisional hernia, LOA, and female gender were found to be associated with longer LOS on univariate analysis, these factors were not found to independently enhance the predictive ability of the regression model that was created.
Conclusions
Mesh size, incarcerated hernia, patient age, and complex hernia predict longer length of stay after laparoscopic ventral hernia repair.
References
Lomanto S, Iyer G, Shabbir A, Cheah WK (2006) Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc 20:1030–1035
Mudge M, Hughes LE (1985) Incisional hernia: a 10-year prospective study of incidence and attitudes. Br J Surg 72:70–71
Lewis RT, Wiegand FM (1989) Natural history of vertical abdominal parietal closure: prolene versus dexon. Can J Surg 32:196–200
Hoer J, Lawong G, Klinge (2002) Factors influencing the development of incisional hernia: a retrospective study of 2983 laparotomy patients over a period of 10 years. Chrirug 73:474–480
National Center for Health Statistics (2007) Combined surgery data (NHDS and NSAS) data highlights. Available at http://www.hesonline.nhs.uk
Sajid M, Bokhar S, Mallick A, Cheek E, Baig MK (2009) Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg 197:64–72
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83(5):1045–1051
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3(1):39–41
Ramshaw BJ, Estaria P, Schwab J, Mason EM, Wilson RA, Duncan TD, Miller J, Lucas GW, Promes J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65:827–831
Holzman MD, Purut CM, Reintgen K, Pappa TN (1997) Laparoscopic ventral and incisional hernioplasty. Surg Endosc 11:32–35
Ballem N, Parikh R, Berber E, Siperstein A (2008) Laparoscopic versus open ventral hernia repairs: 5 year recurrence rates. Surg Endosc 22:1935–1940
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized control trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Perrone JM, Soper NJ, Eagon JC, Klingensmith ME, Aft RL, Frisella MM, Brunt LM (2005) Perioperative outcomes and complications of laparoscopic and ventral hernia repair. Surgery 138(4):708–715
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Rives J, Pire JC, Flament JB, Palot JP, Body C (1985) Treatment of large eventrations. New therapeutic indications apropos of 322 cases. Chirurgie 111:215–225
Wantz GE (1991) Incisional hernioplasty with mersilene. Surg Gynecol Obstet 172:129–137
Koehler RH, Voeller G (1999) Recurrences in laparoscopic incisional hernia repairs. A personal series and review of the literature. J Soc Laparoendosc Surg 133:378–382
Luijendijk RW, Hop WC, Van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruininckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
White TJ, Santos MC, Thompson JS (1998) Factors affecting wound complications in repair of ventral hernias. Am Surg 64:276–280
Raftopoulos I, Vanuno D, Khorsand J, Ninos J, Kouraklis G, Lasky P (2002) Outcome of laparoscopic ventral hernia repair in correlation with obesity, type of hernia, and hernia size. J Laparoendosc Adv Surg Tech 12(6):425–429
Shah RH, Sharma A, Khullar R, Soni V, Baijal M, Chowbey PK (2009) Laparoscopic repair of incarcerated ventral abdominal wall hernias. Hernia 12(5):457–463
Saber A, Elgamal M, Mancl T, Norman E, Boros M (2008) Advanced age: Is it an indication or contraindication for laparoscopic ventral hernia repair? JSLS 12:46–50
Tessier DJ, Swain JM, Harold KL (2006) Safety of laparoscopic ventral hernia repair in older adults. Hernia 10:53–57
Townsend (2007) Sabiston textbook of surgery. Chapter 44: Ventral hernias, 18th edn. W.B. Saunders, Philadelphia
Read RC, Yoder G (1989) Recent trends in the management of incisional herniation. Arch Surg 124:485–488
Bendavid R (2001) Abdominal wall hernias: principles and management. Chapter 88: Epidemiology of hernias in the female. Springer, New York, p 617
Disclosures
Authors Ashwin Kurian, Sidhbh Gallagher, Abhiman Cheeyandira, and Robert Josloff have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurian, A., Gallagher, S., Cheeyandira, A. et al. Predictors of in-hospital length of stay after laparoscopic ventral hernia repair: results of multivariate logistic regression analysis. Surg Endosc 24, 2789–2792 (2010). https://doi.org/10.1007/s00464-010-1048-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1048-4